Patients who undergo heart transplants (HT) have many complications and multiorgan failure (MOF), which increases morbimortality.1,2 No studies so far have analyzed the impact of post-HT MOF in children. Some studies have shown the predictive value of THE inotropic index (II) in cardiac surgery3,4 and HT in children.5 The goal of this study was to analyze the prognostic utility of MOF scores and the II in HT in children in relation to mortality, the length of admission in the pediatric intensive care unit (PICU) and the duration of mechanical ventilation (MV).
One observational, retrospective, single-center study approved by the local ethics committee was conducted including 65 children (mean age, 57 months-old) admitted to the PICU after sustaining HTs between the years 2003 and 2014. The worst scores of clinical severity and MOF, Pediatric Logistic Organ Dysfunction (PELOD)6 and Pediatric Multiple Organ Dysfunction Score (PMODS),7 Pediatric Risk of Mortality III (PRISM III),8 Pediatric Index of Mortality 2 (PIM2)9 were estimated within the first 48h after the transplant. The value of II=dopamine+dobutamine+100×adrenaline+100×noradrenaline+10×milrinone (all in μg/kg/min)+10,000×vasopressin (mU/kg/min) was estimated as well.3,4 We studied the correlation between the scores and PICU mortality and the length of the PICU stay and the duration of MV. In order to complete the statistical analysis, the chi-square test, Fisher's exact test, Mann–Whitney U test, and Spearman's Rho tests were used. P values <.05 were considered statistically significant.
Fifty-point-eight percent (50.8%) had congenital heart disease, 47.7% cardiomyopathy, and 4.6% myocardial tumors. The PRISM III score was 12.6% (P25–P75: 3.5–25.9) and the PIM 2 score was 19% (P25–P75: 3.4–27.8). Other scores were: PELOD 11 (P25–P75: 2–13) and PMODS 5 (P25–P75: 3–8). The II was 22 (P25–P75: 15–36). There was a moderate correlation between the II and the PRISM III (r=.260; P=.036), PELOD (r=.370; P=.003), and PMODS scores (r=.300; P=.002) but not with the PIM2 scores (r=.300; P=.120).
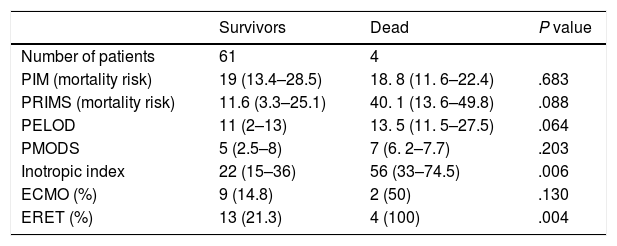
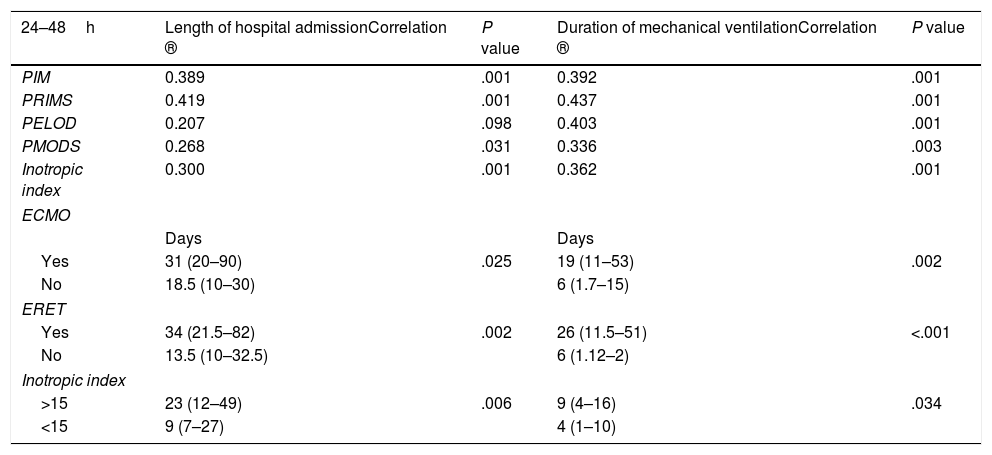
Four patients died (6.2%) during the PICU admission, but only one due to MOF. There was no correlation whatsoever between the MOF scores or the clinical severity scores and mortality (Table 1). The II was significantly higher among dead children (Table 1). The mortality differences seen among children with II>15 (8.1%) and <15 (0%) were not statistically significant (P=.565). Children who died required ECMO and the extrarenal epuration technique (ERET) more often than survivors did, yet the differences were only statistically significant with the ERET (Table 1). There was a moderate correlation between the II and clinical severity and MOF scores (except for PELOD) and the length of PICU admission and duration of MV (Table 2). Patients with II>15 after the HT had the longest PICU stays.
Correlation between mortality and clinical severity and multiorgan failure scores, inotropic index, and need for ECMO and ERET within the first 48h after heart transplant.
| Survivors | Dead | P value | |
|---|---|---|---|
| Number of patients | 61 | 4 | |
| PIM (mortality risk) | 19 (13.4–28.5) | 18. 8 (11. 6–22.4) | .683 |
| PRIMS (mortality risk) | 11.6 (3.3–25.1) | 40. 1 (13. 6–49.8) | .088 |
| PELOD | 11 (2–13) | 13. 5 (11. 5–27.5) | .064 |
| PMODS | 5 (2.5–8) | 7 (6. 2–7.7) | .203 |
| Inotropic index | 22 (15–36) | 56 (33–74.5) | .006 |
| ECMO (%) | 9 (14.8) | 2 (50) | .130 |
| ERET (%) | 13 (21.3) | 4 (100) | .004 |
Values are expressed as means and P25–P75 or as absolute values and percentages.
ECMO, extracorporeal membrane oxygenation; ERET, extrarenal epuration technique; PELOD, Pediatric Logistic Organ Dysfunction; PIM2, Pediatric Index of Mortality 2; PMODS, Pediatric Multiple Organ Dysfunction Score; PRISM III, Pediatric Risk of Mortality III.
Correlation between the length of hospital admission and mechanical ventilation and clinical severity and multiorgan failure scores, and need for ECMO and ERET within the first 48h after heart transplant.
| 24–48h | Length of hospital admissionCorrelation ® | P value | Duration of mechanical ventilationCorrelation ® | P value |
|---|---|---|---|---|
| PIM | 0.389 | .001 | 0.392 | .001 |
| PRIMS | 0.419 | .001 | 0.437 | .001 |
| PELOD | 0.207 | .098 | 0.403 | .001 |
| PMODS | 0.268 | .031 | 0.336 | .003 |
| Inotropic index | 0.300 | .001 | 0.362 | .001 |
| ECMO | ||||
| Days | Days | |||
| Yes | 31 (20–90) | .025 | 19 (11–53) | .002 |
| No | 18.5 (10–30) | 6 (1.7–15) | ||
| ERET | ||||
| Yes | 34 (21.5–82) | .002 | 26 (11.5–51) | <.001 |
| No | 13.5 (10–32.5) | 6 (1.12–2) | ||
| Inotropic index | ||||
| >15 | 23 (12–49) | .006 | 9 (4–16) | .034 |
| <15 | 9 (7–27) | 4 (1–10) | ||
Values are expressed as means and P25–P75.
ECMO, extracorporeal membrane oxygenation; ERET, extrarenal epuration technique; PELOD, Pediatric Logistic Organ Dysfunction; PIM2, Pediatric Index of Mortality 2; PMODS, Pediatric Multiple Organ Dysfunction Score; PRISM III, Pediatric Risk of Mortality III.
Our study is the first one ever to study MOF in HTs performed in children. In our study, MOF scores were high although mortality was low (6.1%), similar to the one reported previously.2,4,5 We did not find a significant correlation between MOF and mortality although the fact that only 4 children died limits the statistical comparison.
In children who have undergone cardiac surgery, a correlation has been found between high II values and a higher mortality rate.3,4 Sanil and Aggarwal found that an II>15 was associated with a higher mortality rate in 51 children after sustaining HTs.5 In our study, those patients who died had significantly higher IIs compared to survivors whereas all the children who died had II values >15, which confirms the prognostic value of II after HT in children. However, the values of II were significantly higher than those found by Sanil and Aggarwal.5 On the other hand, we should take into consideration here that in children on ECMO, the II may underestimate the child's actual clinical severity since they may require lower doses of vasoactive drugs.
HT children with II values >15 had the longest PICU stays which is consistent with what Sanil and Aggarwal described.5 The correlation between the II values and the length of the PICU stay was moderate. Also, there was a moderate correlation between clinical severity and MOF scores and the length of the PICU stay. However, the scores of clinical severity and MOF obtained within the first 48h after the HT do not seem to have a significant predictive value on the length of the PICU stay or the duration of MV in HT children. Larger studies are needed to analyze this.
On the contrary, and same as it happens with other studies, our data show that the need for ECMO and ERET after the transplant keeps an evident correlation with significantly longer stays at the PICU,3,4,10 indicative that the need for these techniques is a significant prognostic marker.
The main limitation of our study is its long-term, retrospective, single-center nature and, although it has a large series, the number of dead patients is too low to be able to make a proper analysis of mortality with one multivariate study. Also, the scores of clinical severity and MOF can be affected in patients treated with ECMO and ERET, since they show values that are falsely low.
In sum, during the postoperative period that follows a heart transplant, children show high levels of MOF scores and a high number of complications. However, their mortality rate is relatively low. The II can be a prognostic indicator of mortality and PICU admission. The MOF scores keep a moderate correlation with the length of the PICU stay and the duration of MV, but not with mortality. Large multicenter studies are needed to analyze the repercussion of MOF in the progression of CT in children.
AuthorsStudy design, statistical analysis, data interpretation, and writing of the manuscript: Jorge López.
Data mining, data interpretation, and writing of the manuscript: María Slöcker, Elena Heras, Daniela Ríos, Laura Barrio, Rosalía Cebrián, and Débora Gómez.
Study design, data interpretation, writing of the manuscript, and study supervision: Jesús López-Herce.
We wish to thank the medical roster and nurses from the Pediatric Intensive Care Unit of the Hospital General Universitario Gregorio Marañón for their collaboration in this study.
Please cite this article as: López J, Slöcker M, Heras E, Ríos D, Barrio L, Cebrián R, et al. Utilidad pronóstica de las puntuaciones de fallo multiorgánico y del índice inotrópico en el postoperatorio de trasplante cardiaco en niños. Med Intensiva. 2019;43:441–443.