Dispatch-assisted bystander cardiopulmonary resuscitation in out-of-hospital cardiac arrest has been shown as an effective measure to improve the survival of this process. The development of a unified protocol for all dispatch centers of the different emergency medical services can be a first step toward this goal in our environment. The process of developing a recommendations document and the realization of posters of dispatch-assisted cardiopulmonary resuscitation, agreed by different actors and promoted by the Spanish Resuscitation Council, is presented.
El soporte telefónico a la reanimación cardiopulmonar por testigos en casos de parada cardiaca extrahospitalaria se ha demostrado como una medida eficaz para mejorar la supervivencia de este proceso. El desarrollo de un protocolo unificado para todos los centros coordinadores de los diferentes servicios de urgencias extrahospitalarias puede ser un primer paso para conseguir en nuestro entorno dicho objetivo. Se presenta el proceso de elaboración de un documento de recomendaciones y su concreción en carteles o pósters de reanimación cardiopulmonar asistida por teléfono, elaborado y acordado por diferentes agentes e impulsado por el Consejo Español de Resucitación Cardiopulmonar.
Out-of-hospital cardiac arrest (OHCA) is a public health problem in Spain and in the rest of Europe, and has been acknowledged as such by the European Parliament.1 Since publication of the first article documenting the effectiveness of external cardiac massage,2 many studies have been made with a view to improving the survival and neurological recovery of patients with OHCA.3
Over 50 years later, early intervention on the part of bystanders, starting patient resuscitation, has become established as one of the key determinants of final patient outcome.4–8 However, despite its importance, early resuscitation by bystanders is performed less often that desired. Although the statistics vary greatly, such resuscitation is recorded in barely 30% of the cases of OHCA.9 In our setting the figure is even lower.10–15
There are contrasted data in the literature showing that telephone support of resuscitation by bystanders (dispatcher-assisted bystander cardiopulmonary resuscitation [CPR]) in both adults and children improves survival following OHCA.16 The resuscitation guides of 2010 recommend the adoption of protocols in the dispatch centers of out-hospital emergency medical services (EMS) designed to identify OHCA and provide first instructions for bystander resuscitation, based on a high level of evidence.16,17
Dispatcher-assisted CPR is defined as the series of instructions delivered by telephone from the EMS coordinating centers with the purpose of favoring collaboration and helping bystanders to apply basic life support measures.18–21
In Spain there has been a great increase in scientific production referred to OHCA in recent years. In addition to the results obtained, interest has focused on specific aspects of the different links in the chain of survival,22–31 aspects related to the resuscitators,32 and strategies following resuscitation (post-resuscitation care and non-heart beating donation programs).33–36 Notoriously, however, no publications in our country have analyzed dispatcher-assisted bystander resuscitation. In fact, a recent survey of the Spanish public EMS conducted in 2013 has shown that only 12 out of 27 services have specific CPR protocols,37 and each service has moreover developed its own protocol.
These data point to the possibility of improvement, reinforcing transit between the first and second link in the chain of survival by adopting a simple organizational intervention. Clear and homogeneous dispatcher-assisted CPR protocols are needed that are easy to apply in all urgency and emergency care coordination centers in our country. Such protocols should be accompanied by specific training of the dispatchers in identifying OHCA and providing instructions referred to basic life support maneuvers.9,38
ObjectiveThe aim of the present project was to develop an expert document on recommendations for promoting dispatcher-assisted bystander cardiopulmonary resuscitation from the EMS coordination centers.
MethodsThe Spanish Cardiopulmonary Resuscitation Council (Consejo Español de Resucitación Cardiopulmonar, CERP) is a non-profit scientific-healthcare association founded in 1999 and constituted by different scientific societies, public institutions and EMS with accredited activity in the field of cardiac arrest, life support and CPR.
The CERCP impulsed the creation of a specific work group in urgency and emergency care coordination. The group was formed by the representatives in the CERP of the EMS belonging to Andalusia, Asturias, Galicia and Madrid (SAMUR-Protección Civil). In accordance with the established aim, the group developed a document and a poster draft following a MEDLINE (http://www.ncbi.nlm.nih.gov/PubMed/), EMBASE (http://www.embase.com) and IME-Biomedicine search (http://bddoc.csic.es:8080/index.jsp) of articles published between February 2010 and October 2014. The search terms were “dispatch-assisted”, “cardiopulmonary resuscitation” and “emergency medical system”. Some articles were not identified in a first search but were obtained from the references found in that search. A first proposal was forwarded to a panel of experts composed of representatives of the EMS; participants in the Out-of-Hospital Spanish Cardiac Arrest Registry (Registro Español de Parada Cardiaca Extra-Hospitalaria, OHSCAR), a project impulsed by the CERCP and financed by the Spanish Fondo de Investigaciones Sanitarias with the participation of 20 EMS from all over the country (the 17 Spanish Autonomous Communities, the municipal services of Madrid and Zaragoza, and the Emergencies Service of Ceuta) (www.ohscar.org); the members of the Spanish Group of Pediatric and Neonatal Cardiopulmonary Resuscitation (Grupo Español de Reanimación Cardiopulmonar Pediátrica y Neonatal); and the advisory Scientific Committee of the CERCP.
The basic premises for drafting the recommendations were:
- •
Short messages containing key words.
- •
Dispatch (telephone) deliverable.
- •
Understandable (simple language).
- •
Performable by a lay person under difficult conditions.
- •
Presentation in poster format, comprising steps that are easy to follow, with identification and reinforcement of the key actions required.
To this effect an analysis was made of the steps to be followed in dispatcher-assisted life support instructions, with the identification of a series of key issues:
- 1.
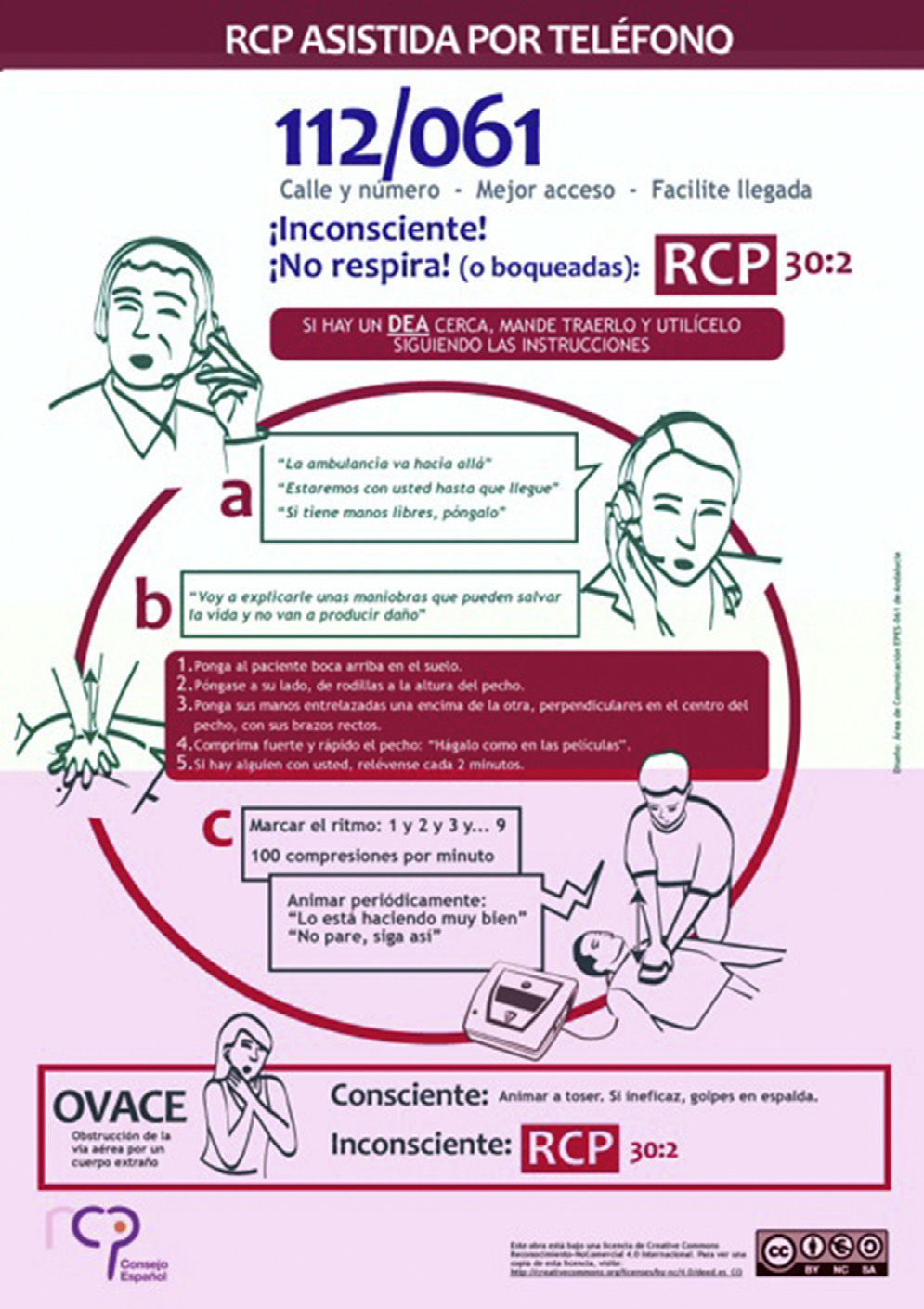
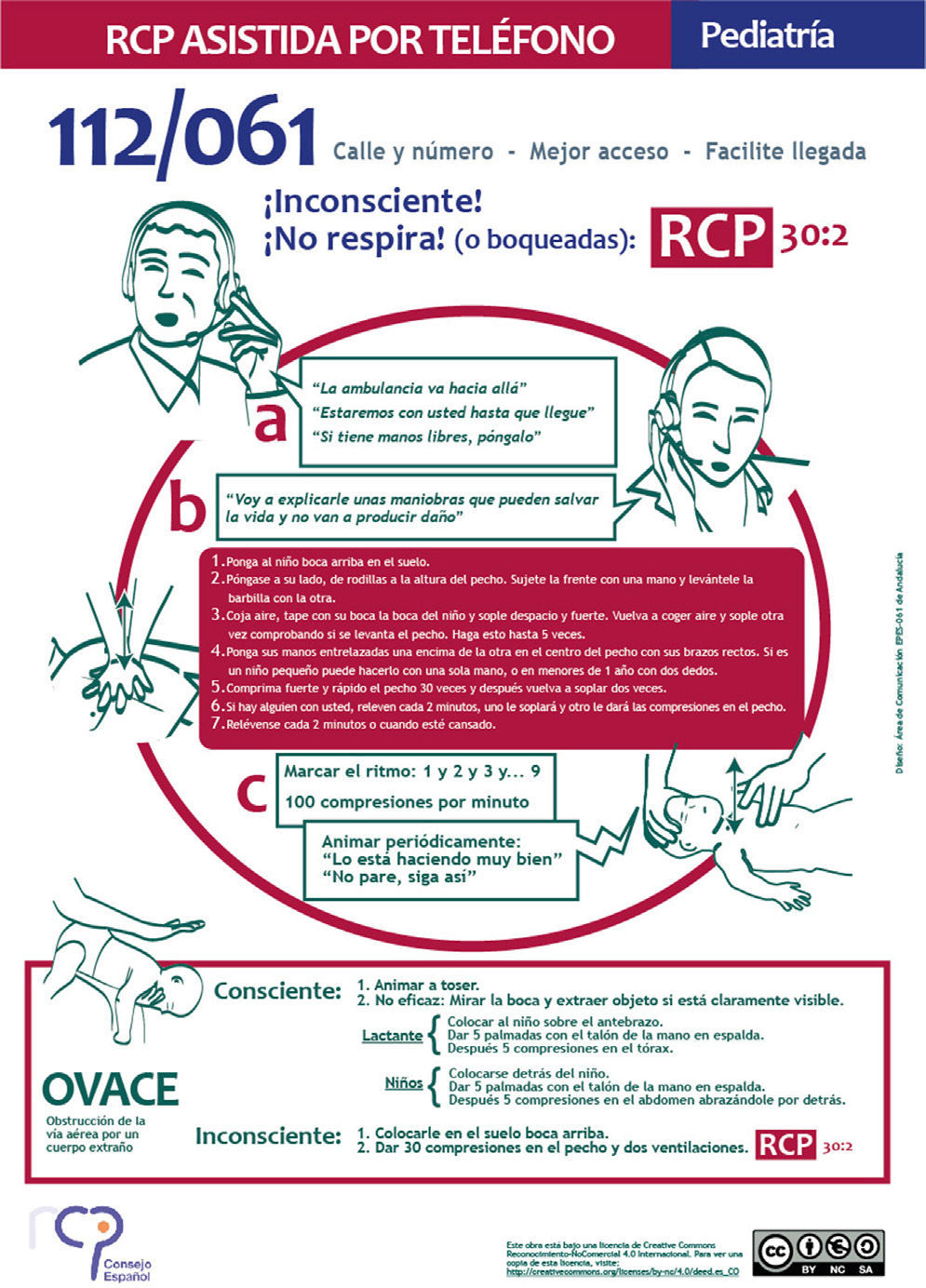
Recognition of OHCA, identification of the absence of breathing or of ineffective breathing (gasping),38–40 and indication of an automated external defibrillator.
- 2.
The provision of instructions to reduce possible rejection to perform CPR on the part of bystanders,41,42 giving them confidence in performing the necessary maneuvers.
- 3.
Evidence on the specific telephone instructions regarding the recommended strategy, i.e., CPR only with chest compression versus conventional resuscitation with chest compression and ventilation in the adult. The evidence referred to the different age groups was also analyzed.43–45 Likewise, interventional recommendations were included for cases of foreign body-caused airway obstruction.
- 4.
Consideration of the need for a simple, homogeneous protocol for all the EMS, allowing evaluation of its suitability and impact following the standards recommended in the international literature.46
Two rounds of open suggestions were held on the key elements to be included in the recommendations document. After these consultations, the corresponding document and poster were drafted, followed by e-mail distribution to all the participants for their definitive approval.
Two proposals integrating the dispatcher-assisted bystander cardiopulmonary resuscitation recommendations in a single element were analyzed. Given the difficulty of embodying instructions for adults and for children in one same document, the decision was made to develop two separate supportive elements (shown in Figs. 1 and 2). These posters are accessible in the four official languages in Spain, and can be found on the CERCP website (www.cercp.org).
DiscussionThe unification of protocols can contribute to better identification of situations of OHCA, and to increased CPR interventions by bystanders. This constitutes an intermediate step for promoting training of the coordination center personnel in dispatcher-assisted bystander cardiopulmonary resuscitation (basic life support measures). Likewise, it facilitates the evaluation and comparison of efforts by the emergency coordination centers46 and, in sum, may be a positive intervention from the public health perspective.9 The different EMS should measure effort in dispatcher-assisted bystander cardiopulmonary resuscitation as part of their quality assurance program.
Once these protocols have been published and distributed among the different EMS, it will be necessary to evaluate their degree of implementation, and in later phases an analysis will be needed of their possible repercussions upon the medical care and survival of patients with OHCA. According to the first unpublished data on the OHSCAR project (prior to this initiative), the dispatcher-assisted bystander cardiopulmonary resuscitation rate is in the order of 5%.
The development and publication of these protocols is an initiative of the CERCP to unify and improve OHCA care through different tools, following the international recommendations,16 and opens the door to new areas of research in OHCA and CPR.
We consider the presentation and publication of these protocols to be a key element for their diffusion among all the professionals in different settings who are involved and interested in this field of knowledge, and may contribute (as has been demonstrated in other scenarios) to increase the practice of dispatcher-assisted bystander cardiopulmonary resuscitation and improve the survival outcomes in OHCA47 –though this requires the commitment and participation of all the parts involved.
Conflicts of interestThe authors declare that they have no conflicts of interest.
Please cite this article as: García del Águila J, López-Messa J, Rosell-Ortiz F, De Elías Hernández R, Martínez del Valle M, Sánchez-Santos L, et al. Recomendaciones para el soporte telefónico a la reanimación por testigos desde los centros de coordinación de urgencias y emergencias. Med Intensiva. 2015;39:298–302.