Venous thromboembolic disease (VTD) includes both the development of deep vein thrombosis (DVT) and pulmonary thromboembolism (PTE) and is one of the most significant complications of severe traumatic disease. The incidence rate of PTE is between 1% and 6% yet the presence of asymptomatic PTE is documented in up to 24% of the cases on the computed tomography scans performed during the first 7 days of disease progression.1
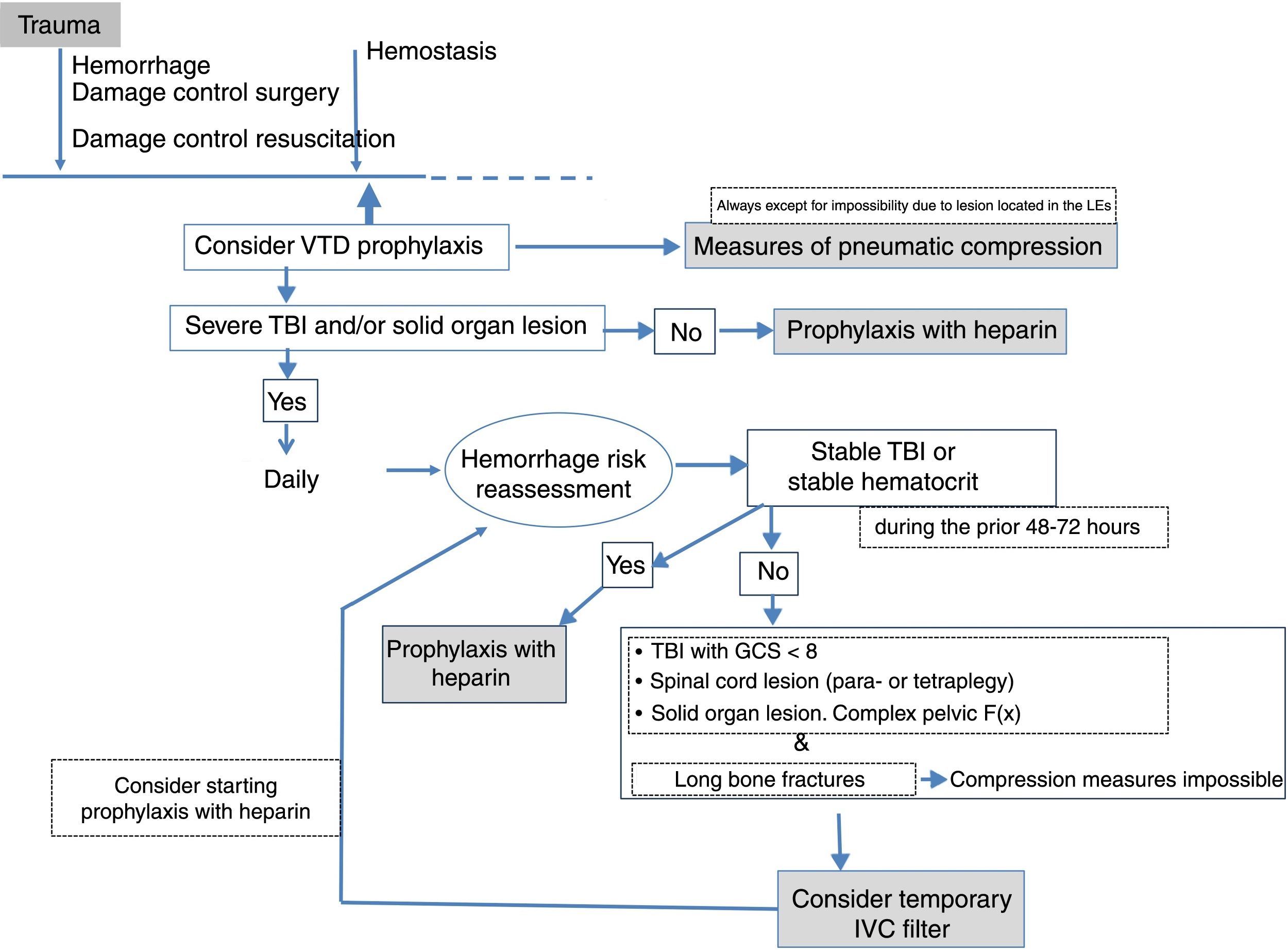
The clinical guidelines for the management of trauma patients recommend prophylaxis with low molecular weight heparin and compression measures.2,3 However, the coexistence of potentially fatal bleeding risk and the impossibility to apply physical measures of compression (due to the presence of long bone fracture in extremities) limit the options of prophylaxis. The use of prophylactic filters for the inferior vena cava (IVC) is suggested here as an alternative therapeutic option for the prevention of VTD even though to this day its indications, removal, and utility are issues still under discussion.
Indications for temporary inferior vena cava filtersIVC filters have been used in the clinical practice since the 1970s and to this day several tests support the use of therapeutic filters for the management of severe traumatic disease yet do not support its prophylactic indication and there are no widely accepted patterns on this regard either.3
A review of the indications for IVC filter placement suggests that these devices can be considered in trauma patients with high risk of developing VTD who are not eligible to receive anticoagulation therapy.3 The ideal candidates to receive these filters would be patients with serious traumatic brain injuries (TBI), spinal cord injuries with para- and tetraplegy, solid organ lesions, or complex pelvic fractures accompanied by long bone fractures that make prophylaxis with the corresponding compression measures absolutely impossible. However, the guidelines established by the American College of Chest Physicians in its last two iterations or the 4th edition of the European Guidelines for the Management of Traumatic Coagulopathy do not recommend the use of these filters for routine prophylactic purposes.2,4,5 Here the lack of solid and conclusive evidence and the existence of contradictory guidelines from different scientific societies has brought variability to the prophylactic insertion of IVC filters in the trauma setting. This means that among same-level hospitals6,7 the use of IVC filters is not regulated, which has led to completely different insertion rates being reported somewhere between 0.6 and 9.6%.8,9
Effectiveness of temporary inferior vena cava filtersThere is this idea that the prophylactic use of IVC filters is good enough to prevent VTD, yet several studies published have documented the development of DVT even with these devices already implanted.10,11 There are three (3) possible causes for this. In the first place, it may be due to the development of thrombi in pulmonary circulation or DVT in upper extremities, territories where the filter does no act upon. On the other hand, it may be showing the lateralization-related ineffectiveness of the device. Also, most devices are implanted within the first week following a severe trauma when the risk of bleeding is at its peak. Yet there is a prothrombotic phase when drug prophylaxis should be considered (7–10 days after filter insertion).10
The medical literature provides heterogeneous results when it comes to the effectiveness of these filters. Several publications including a recent meta-analysis conducted back in 2014 confirmed that the prophylactic insertion of IVC filters was associated with a lower incidence of PTEs and massive PTEs in trauma patients, but without an effect on the overall mortality.7,8,12 Also, cost-effectiveness analyses show low benefits, indicative that the selection of patients needs to be flawless.13 We believe that these studies should be interpreted with caution since, in many of them, mortality data were obtained from trauma registries with the corresponding limitations. Also, in the context of severe traumatic disease, several variables may impact mortality as confounding factors.
Complications associated with inferior vena cava filtersIVC filters have complications, among which we may find vena cava perforations,14 the displacement-migration of the device (2.2%),10 and the thrombosis/occlusion of the filter (7.8%).11 On the other hand, we should remember that although these filters are temporary, they are not always removed due to the lack of follow-up.9,15 This perpetuates the situation of foreign body with the corresponding comorbidities since these filters do not reduce the risk of VTD to zero. The longer the filter remains in the body, the more thrombotic processes we may encounter with the corresponding complications during the extraction process.11,15 High scores in the Injury Severity Score, long bone fractures, and delays when initiating drug prophylaxis have been reported as independent factors associated with the development of PTE after the insertion of a prophylactic device.10 For all these reason, the presence of these filters inside the body should be minimal and drug prophylaxis should be initiated once the risk of hemorrhage is gone (Fig. 1). For now it is hard to tell what the best moment is to remove the device, but there should be a follow-up on these filters, and their indication should be reconsidered once there is confirmation that VTD (drug or mechanical) prophylaxis is possible. The new generation of filters and the results recently published on this regard confirm that it is safe to remove them in much longer periods of time (up to 120 days).10
ConclusionsThe IVC filter may play an important role in the prevention of VTD in severe trauma patients, yet the scarce evidence available on its indications and effectiveness added to the possible complications that may arise have prevented its widespread use. Trauma patients with contraindications to receive anticoagulation due to risk of bleeding and who are not eligible for mechanical prophylaxis should be a possible indication. Its implementation and follow-up should take place in selected centers in order to minimize associated secondary damages.
We believe there is this pressing needs to identify the best clinical practice for the management of VTD in the setting of trauma patients. This study would give us the evidence we need to establish management guidelines and reduce variability in clinical practice.
Conflicts of interestThe authors declared no conflicts of interest whatsoever.
Please cite this article as: Ballesteros MÁ, Llompart-Pou JA, Egea-Guerrero JJ. Filtros temporales de vena cava inferior en traumatismo grave. Med Intensiva. 2019;43:500–502.