Technology and insertion techniques for cardiac temporary internal pacing have experienced a remarkable development over the last few years. Despite this fact, the procedure continues to have potentially fatal associated complications. Temporary internal pacing is indicated for the treatment of bradyarrhythmias or tachyarrhythmias refractory to conventional treatment, or arrhythmias causing cardiovascular or clinical instability of the patient. On the other hand, the indications of temporary cardiac pacing are far less well defined than those of permanent pacing. Since the decision of implementing temporary pacing is complex and delicate, it should always be carefully considered, and over-indication should be avoided. We must base these decisions on robust knowledge of the arrhythmias that may benefit from temporary internal pacing, and should also acquire the habit of considering external temporary pacing among other less aggressive treatments, and to make the best use of new technologies such as echocardiography that add accuracy to the procedure.
La estimulación transitoria intravenosa ha experimentado en los últimos años grandes avances tanto a nivel de la técnica de implantación como a nivel tecnológico, a pesar de lo cual es una técnica que puede llegar a presentar graves complicaciones. Habitualmente, se implantan marcapasos provisionales por bradiarritmias o taquiarrítmias refractarias a tratamientos conservadores, o cuando se produce inestabilidad hemodinámica o clínica del paciente. Si sumamos que las indicaciones son mucho menos claras que las de la estimulación cardiaca definitiva, comprobamos que la decisión de implantar un marcapasos provisional intravenoso es siempre complicada y arriesgada, por lo que debemos evitar una sobreutilización de este tipo de estimulación. Para enfrentarnos con mayor garantía a esta situación, debemos valernos de un mejor conocimiento de las arritmias que nos hacen plantearnos el implante, valorar alternativas menos agresivas, como el marcapasos transcutáneo, y valernos de las nuevas tecnologías, como la ecografía, que facilitarán el desarrollo de esta técnica.
Since Zoll1 first applied two electrodes connected to a generator to the thorax via the hypodermic route in 1952, temporary cardiac pacing has experienced great advances in terms of both technology and the techniques employed. This has resulted in a notorious increase in the use of temporary internal (transvenous) pacemakers (TVPs) in recent years. Indeed, excessive use is sometimes made of these devices, and the indications may be rather questionable.
Although the learning curve is not too demanding, the technique is not without complications—many of which can be serious.2
Internal pacing seeks to achieve clinical and hemodynamic stabilization in patients who present acute electrical instability due to bradyarrhythmias or tachyarrhythmias. However, the indications of TVP are far less clear than those of permanent cardiac pacing, since they are based on clinical experience rather than on scientific evidence.3–5
In general, TVP is indicated in bradyarrhythmias with hemodynamic alterations that do not respond to conservative management (positive chronotropic drugs, treatment of the underlying cause, etc.) or in situations where permanent pacemaker (PPM) implantation is not indicated at the time or is not possible, or where the risk of PPM implantation outweighs its benefits. In any case, the cause triggering the arrhythmia always should be treated if possible.
The decision to implant a TVP is sometimes difficult. Caution should accompany the decision, since implantation in situations of paroxysmal atrioventricular block (AVB) can cause the latter to become dependent upon the pacemaker – with the consequent risk of cardiac arrest in the event of accidental electrode displacement.
Likewise, in the case of tachyarrhythmias, and once the etiological and drug treatment options have been exhausted, we can resort to cardiac overdrive or overstimulation in an attempt to revert the situation, as in patients with torsades de pointes or polymorphic ventricular tachycardias associated to prolongation of the QT interval.6,7
As a general rule, patients will require TVP if they suffer syncope, cardiac arrest or hemodynamic instability secondary to bradycardia/tachycardia, once the conservative measures have failed or are difficult to apply in a rapid and effective manner.
The big problem is defining hemodynamic instability. What do we mean by “instability”? Hypotension? The need for vasoactive drugs? And if so, at what doses? Do we take the shock index to be a subjective piece of information? Oliguria? Hypoperfusion? Diminished consciousness? Can we really improve the hemodynamic condition of a patient suffering from bradycardia with the implantation of a single-chamber PPM in VVI pacing mode, knowing that this may lead to a loss of atrioventricular synchronization with a consequent drop in cardiac output?8 It is not always easy to make a decision.
The present study aims to analyze the indications and complications of TVP implantation, following a review of the series found in the literature—an arduous task considering the diversity of published results.
In addition to TVP, there are other temporary pacing options, e.g., transcutaneous, epicardial or transesophageal pacing modes, each with different advantages and inconveniences—though such systems will not be addressed here.9–11
IndicationsThe indications of TVP are classified according to the urgency of the situation. However, they lack clear supporting evidence, except in the case of syncope, cardiac arrest or hemodynamic instability secondary to bradycardia or tachycardia.
It is common for this kind of situation to manifest in acute myocardial infarction (AMI). In the event of AVB in the context of inferior AMI, we usually observe a suprahisian escape rhythm, associated to a good prognosis and favorable response to positive chronotropic drugs. Both the sinus node (SN) and the atrioventricular node (AVN) are irrigated by the circumflex artery or the right coronary artery; as a result, conduction alterations in the context of inferior AMI are transient and rarely progress. Other mechanisms are the activation of chemoreceptors in the posterior wall of the left ventricle, the release of adenosine, and an increased effect of the parasympathetic tone. In contrast, in anterior AMI, the appearance of blocking phenomena is indicative of a poor prognosis due to the degree of block, which in this case is associated to ventricular escape rhythms with bundle block morphology, since the His-Purkinje system is usually irrigated by the anterior descending artery or some of its branches. Such situations progress towards complete block in an unpredictable and abrupt manner. Furthermore, the great extent of myocardium affected by ischemia in these cases (interventricular septum and anterior wall) results in important ventricular dysfunction and a poor short-term prognosis.12 Such conditions were relatively common in the pre-percutaneous angioplasty era. At present, however, and thanks to early coronary revascularization, any such phenomena that may arise are quickly resolved once coronary flow has been restored.13
Outside the context of AMI, in the case of symptomatic bradycardia, TVP is indicated conditioned to the clinical and hemodynamic tolerance of the patient, and depending on the stability of the ventricular escape rhythm, when the heart rate drops to under 40bpm and the rest of conservative measures (such as transcutaneous pacing) have failed.
Therefore, management without TVP should be attempted in patients with high degree block, sick sinus syndrome, etc., in the absence of excessive symptoms, reducing possible complications and leaving the venous accesses free for posterior PPM implantation.14 The indication of TVP must always be established on an individualized basis according to the clinical condition and course—special consideration being placed on the history of the disease process leading to the arrhythmia and the earliness of PPM implantation.
Clinical guidesAfter reviewing the guides of the different scientific societies, we have established a number of recommendations for the implantation of TVP. The only guides that establish grades of recommendation are those corresponding to acute coronary syndrome with ST-segment elevation of the American Heart Association (AHA) of 2004,15 and only in the context of AMI, while no such mention is made in the rest of the guides.16–20
There are a number of possible scenarios:
- 1.
Situations giving rise to symptomatic bradycardia that are revertible in time and do not require PPM implantation:
- -
Damage to the SN, AVN or His-Purkinje system may occur after heart surgery. In these cases, and in order to maintain adequate hemodynamic stability in situations of dilated or hypertrophic myocardiopathy, the implantation of a provisional dual-chamber pacemaker may be of benefit. Following coronary revascularization surgery, damage to the SN or AVN is usually reversible. However, damage to the AVN or His-Purkinje system after valve replacement surgery tends to be permanent and ultimately require PPM implantation.
- -
Different forms of myocarditis (Lyme disease).
- -
Heart transplantation (usually associated to reversible alterations of the SN).
- -
Cardiac contusion in the context of chest injuries implies a risk of AVB.
- -
Electrolytic or metabolic alterations, intoxications or side effects of different drugs.
- -
Situations of left bundle block, and possible right bundle alterations at insertion of a pulmonary artery catheter.
- -
The perioperative period in patients with bifascicular or incomplete trifascicular block and a history of syncope. In such cases pacemaker implantation may be indicated on a prophylactic basis.
- -
Recurrent supraventricular and ventricular tachycardias, such as polymorphic ventricular tachycardia associated to prolongation of the QT interval, or ventricular tachycardias or fibrillations associated to bradycardia and refractory to conservative management. Pacemaker implantation can be used to terminate or prevent such situations.
- -
- 2.
Recommendations in the context of AMI (Table 1).
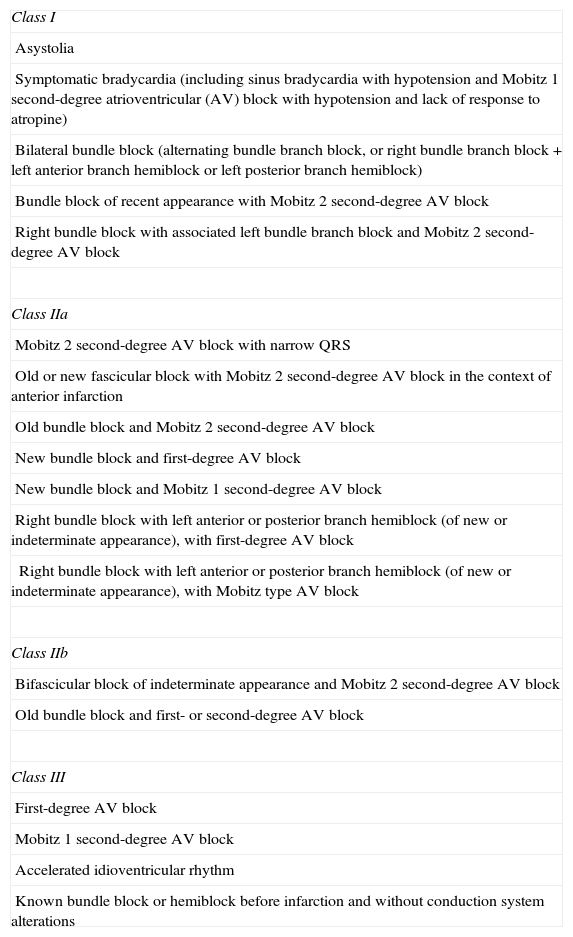
Table 1.Indications of temporary internal (transvenous) pacing in acute myocardial infarction.
Class I Asystolia Symptomatic bradycardia (including sinus bradycardia with hypotension and Mobitz 1 second-degree atrioventricular (AV) block with hypotension and lack of response to atropine) Bilateral bundle block (alternating bundle branch block, or right bundle branch block+left anterior branch hemiblock or left posterior branch hemiblock) Bundle block of recent appearance with Mobitz 2 second-degree AV block Right bundle block with associated left bundle branch block and Mobitz 2 second-degree AV block Class IIa Mobitz 2 second-degree AV block with narrow QRS Old or new fascicular block with Mobitz 2 second-degree AV block in the context of anterior infarction Old bundle block and Mobitz 2 second-degree AV block New bundle block and first-degree AV block New bundle block and Mobitz 1 second-degree AV block Right bundle block with left anterior or posterior branch hemiblock (of new or indeterminate appearance), with first-degree AV block Right bundle block with left anterior or posterior branch hemiblock (of new or indeterminate appearance), with Mobitz type AV block Class IIb Bifascicular block of indeterminate appearance and Mobitz 2 second-degree AV block Old bundle block and first- or second-degree AV block Class III First-degree AV block Mobitz 1 second-degree AV block Accelerated idioventricular rhythm Known bundle block or hemiblock before infarction and without conduction system alterations - 3.
In symptomatic bradycardia of degenerative origin, without response to drug treatment and which almost surely will require PPM implantation, TVP is indicated in the presence of:
- -
SN dysfunction
- -
Second- or third-degree AVB
- -
- 4.
As a general rule, TVP is to be avoided or used with great caution:
- -
In the presence of mild, intermittent or well tolerated symptoms, independently of the primary conduction alteration involved.
- -
During the implantation of a tricuspid valve prosthesis or in right ventricle infarctions, since ventricular capture may prove difficult.
- -
In situations of coagulopathy, where the administration of platelets and prothrombin complexes is advisable in order to reduce the risk of bleeding.
- -
Temporary internal pacing is usually performed in extreme emergencies secondary to severe arrhythmia. The affected patients are often elderly, in poor general condition, with hemodynamic instability, a low cardiac output, and scantly cooperative. All this favors the development of complications, which may be minor (hematoma at the puncture site), serious (e.g., cardiac tamponade) or even fatal.2
An analysis of the literature on such complications is greatly complicated by the fact that the different series make use of different definitions. In some articles, local infection at the puncture site is regarded as a minor complication, while other studies do not even mention such problems.
In 2006, McCann21 analyzed 15 studies including 3700 patients covering the period 1973–2004, in an attempt to homogenize the results. The incidence of complications was 26.5% (range 10–60%). Volkmann et al.,22 in 1983, underscored the existence of a low incidence of complications (13.7%), with no deaths. On the other hand, in 1996, Murphy23 reported a complications rate of 35% with a mortality rate of 28%, in a series of 194 patients. In 2004, López-Ayerbe et al.,2 in another series of 530 cases, reported a complications rate of 18.5% with a mortality rate of 6%—though only three deaths were attributable to the pacemaker.
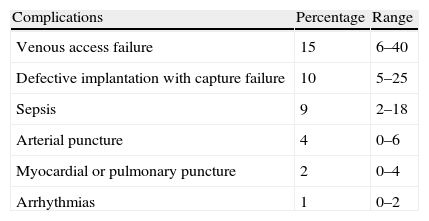
The incidences of the different complications according to the analysis of McCann21 are reported in Table 2.
Reducing the number of complications requires an analysis of the underlying causes. Murphy24 related the incidence of complications to the experience of the implanting professionals (general practitioners or specialists in training), supervision, and the geographical setting. However, the solution is not simple, considering the difficulty of ensuring the presence of specialists in the field in the different hospitals, the absence of 24-h a day coverage, the heterogeneity of the training programs, and the extreme emergency with which pacemaker implantation is carried out.
In our opinion, the incidence of complications could be reduced by adequate protocolization of the indication of temporary internal pacing, taking into account the existence of alternatives other than TVP, such as transcutaneous pacing. Another contributing element would be improved training of the personnel in charge of performing the technique outside the specialized units, through temporary training stays in units that see many patients of his kind, or in cardiac pacing reference centers.
Access routesHaving established the indication of temporary internal pacing, the first difficulty we face is central venous catheterization. The learning curve is crucial in this respect, since the insertion process can give rise to an important number of complications (hematomas, pseudoaneurysms, pneumothorax, hemothorax, etc.). Ultrasound guidance can lessen the complications of catheterization. The greatest level of evidence supporting the use of this technique corresponds to catheterization of the internal jugular vein (level A2), with greater controversy in the case of the subclavian vein (level C2) or femoral vein (level D).25
In effect, the use of one access route or other has been the subject of controversy in recent years.
The British Society of Cardiology26 recommends the right internal jugular vein as the access of choice, particularly in scantly experienced hands, since it represents the most direct route to the right ventricle and appears to be associated to fewer complications such as electrode displacement (with an incidence of only 8%), compared with other alternatives such as the antecubital route, which is presently little used for TVP.17
López-Ayerbe et al.2 used the femoral route in 99% of their 530 patients. The reported complications rate was 19%, though the data appear to be somewhat ambiguous, since they do not appear to include deaths. Furthermore, the authors use terms such as “serious” and “severe”, which have different interpretations.
The subclavian vein is another commonly used route, though it is associated with a higher incidence of pneumothorax, and hemostasis moreover proves difficult in the event of arterial puncture.
In our opinion, the use of an extra-thoracic access route should be the first choice, with the purpose of keeping the mentioned veins free in case future permanent pacemaker implantation proves necessary. Nevertheless, other authors prefer the right jugular and subclavian veins, because they provide easier access to the right ventricle.27
ConclusionsTemporary internal pacing is often a difficult decision, since its indications are not as clear as in the case of permanent cardiac pacing—the indications being based more on clinical experience than on scientific evidence. As a general rule, TVP is indicated in the case of clinical and hemodynamic instability secondary to bradyarrhythmias and tachyarrhythmias, once other more conservative measures have failed, since the technique is associated to complications that may even prove fatal. Avoiding such problems requires good training in the TVP implantation technique, sound knowledge of arrhythmias of this kind, and the support of additional tools such as ultrasound. In any case, the decision to introduce temporary internal pacing should be established on an individualized basis depending on the characteristics of each patient.
Conflicts of interestThe authors declare that they have no conflicts of interest.
Gonzalo Hernández-Martínez (Department of Intensive Care Medicine, Infanta Sofía University Hospital, Madrid); Mar Juan-Díaz, Ainhoa Serrano-Lázaro (Department of Intensive Care Medicine, Valencia University Clinic Hospital); María del Carmen Espinosa-González, María Jesús Polanco-Rayo, Antonio Hernández-Madrid (Department of Cardiology, Ramón y Cajal Hospital, Madrid); Alfonso Ambrós-Checa (Department of Intensive Care Medicine, Ciudad Real University General Hospital).