To analyze the characteristics and variables associated with prolonged noninvasive ventilation performed completely in Emergency Departments (NIV-ED) and its influence upon effectiveness.
DesignA prospective, multicenter, observational multipurpose cohort study was carried out.
SettingVNICAT Registry.
SubjectsPatients in which NIV-ED was performed in 11 Catalan hospitals in the months of February or March 2015.
InterventionNo.
VariablesThe study variable was NIV-ED, which as a function of time was defined as prolonged or not prolonged. The efficacy variable was the success of the technique in terms of patient improvement.
ResultsA total of 125 patients were included, with a median NIV-ED duration of 12 h, which was the cut-off point for the comparator groups. In 60 cases (48%) NIV-ED was not prolonged (<12 h), while in 65 cases (52%) ventilation was prolonged (≥12 h). Non-prolonged NIV-ED was associated to the indication of acute heart failure and prolonged ventilation to the presence of diabetes. There were no differences between non-prolonged and prolonged NIV-ED in terms of efficacy, and the success rate in terms of improvement was 68.3% and 76.9%, respectively, with an adjusted odds ratio of 1.49 (95%CI 0.61–3.60).
ConclusionsProlonged NIV-ED is a frequent situation, but few variables associated to it have been studied. The presence of prolonged ventilation did not influence the success rate of NIV.
Analizar las características y variables asociadas con la ventilación no invasiva realizada completamente en los servicios de urgencias hospitalarios (VNI-SUH) de manera prolongada y su influencia en la eficacia de la técnica.
DiseñoEstudio multicéntrico observacional prospectivo de cohorte multipropósito.
ÁmbitoRegistro VNICat.
ParticipantesPacientes en los que se realiza VNI-SUH en 11 hospitales catalanes en los meses de febrero o marzo del 2015.
IntervenciónNinguna.
VariablesLa variable de estudio fue la VNI-SU, que en función del tiempo se definió como prolongada o no prolongada. La variable de eficacia fue él éxito de la técnica por mejoría.
ResultadosSe incluyeron 125 pacientes con una mediana de tiempo de VNI-SUH de 12 h, que fue el punto de corte para los dos grupos comparados. En 60 (48%) la VNI-SUH fue no prolongada (<12 h) y en 65 (52%) prolongada (≥12 h). La VNI-SUH no prolongada se asoció con la indicación de insuficiencia cardiaca aguda y la prolongada con la presencia de diabetes. Entre la VNI-SUH no prolongada y prolongada no hubo diferencias en la eficacia, éxito por mejoría del 68,3% y 76,9%, respectivamente, con un odds ratio ajustado de 1,49 (intervalo de confianza del 95% de 0,61 a 3,60).
ConclusionesLa VNI-SUH prolongada es una situación frecuente, pero las variables estudiadas que se asocian a ella son escasas. Su presencia no influyo en el éxito de la VNI.
Noninvasive ventilation (NIV) is part of the management of acute respiratory failure (ARF). Its main goals are to reduce the need for orotracheal intubation, and the rate of overall complication and infections associated with techniques of invasive ventilation.1 ARF is common cause for consultation at the hospital emergency services (HES), and NIV is a technique that can be used in this setting,2–4 especially in 2 chronic and prevalent heart conditions like acute heart failure (AHF), and acute chronic obstructive pulmonary disease (COPD) where evidence regarding better disease progression and prognosis by adding NIV to conventional medical therapy has already been proven.5,6 Currently, NIV is also used in HES in other emergent clinical scenarios like pneumonia or acute asthma, although with very few clinical trials clearly backing up its benefits.7–9 The success of NIV is directly associated with how soon it is implemented based on the patient’s clinical signs10 being the continuous monitoring of technique and patient necessary. Also, the healthcare personnel involved needs to be properly trained, and the right environment is required to guarantee the implementation of NIV under the safest possible conditions.1 Taking into account that the use of NIV in HES has become popularized we often see that it is used in an already overloaded healthcare setting and with drainage difficulties. Nonetheless, despite the changes made to HES in things like training and specialization, it should become an early and transient tool as part of the patient’s end-of-life decision.11 In this sense, the Spanish Ministry of Health, Consumer Affairs, and Social Welfare claims that the mean overall stay at the HES setting should be <4 hours. The admission-to-hospitalization time should be <4 hours as well.12 The VNICat study reported that in 83% of the patients, NIV was implemented completely at the HES setting from the beginning until it was removed following clinical improvement or failure.4 Consequently, cases of prolonged NIV can be seen. These cases collapse the entire healthcare system and can have a negative effect on the efficacy of the technique at the emergency setting.13 Therefore, the objective of our study was to analyze the characteristics and variables associated with prolonged times of completely implemented prolonged NIV at the HES setting (NIV-HES). Also, to study the impact this has on the efficacy of the technique.
MethodThis study was intended as a sub-analysis of the data mined in the VNICat registry that included patients in whom NIV had been initiated and removed at the HES setting. The VNICat registry was a multicenter, analytical, prospective, cohort study with consecutive inclusion of patients treated with NIV in 11 HES and in the Sistema d’Emergencies Mèdiques (SEM) at pre-hospital level for 1 month between February and March of 2015. The inclusion criteria were patients aged >18 years treated with NIV, and a prior written informed consent duly signed by the patients. Exclusion criteria were the patient’s refusal to participate in the registry or the impossibility to sign the informed consent. The decision to start treating the patient with NIV was left to the physician’s criterion. The patient’s response to NIV was studied following the clinical assessment and gasometric criteria established in the clinical practice guidelines.1 NIV was administered by trained personnel in this technique at the HES setting. Specific turbine-based ventilators, and the right interfaces were used to administer NIV. The lead investigator of each center reviewed all the events recruited. Duplicate events were excluded.
A total of 23 variables were collected and studied. Two demographical variables, age, and sex. A total of 9 variables of past medical history were collected too: smoking, arterial hypertension, diabetes, chronic kidney disease, stroke, COPD, previous heart failure, active neoplasm, and the Charlson Comorbidity Index (CCI). A total of 7 variables were associated with characteristics of NIV per se: its indication (AHF, COPD, pneumonia, and other clinical scenarios not included in the former ones), the modality of support pressure, positive end-expiratory pressure, continuous positive airway pressure, titrated support pressure, time on NIV (in hours), life-sustaining treatment limitation (LSTL) established by the treating physician, and efficacy of NIV. For efficacy assessment purposes, NIV was considered successful when it could be delayed due to the patient’s improvement. However, it was considered a failure when it had to be delayed due to intolerance to the technique, need for orotracheal intubation or death. The variable type of respiratory failure was assessed with data from the arterial gasometry at the HES admission. Three different scenarios were defined then: presence of ARF with hypercapnia with PaCO2 > 45 mmHg, ARF with hypoxemia with PaO2 < 60 mmHg, and respiratory acidosis with PaCO2 > 45 mmHg, and pH <7.35. Finally, 4 evolutionary variables were collected: need for hospitalization, hospital stay, and mortality at the emergency and at the hospital settings. The median of the duration of NIV-HES was estimated in hours. Also, 2 different groups were defined based on this value: duration of NIV-HES below the median and same or above the median. The study variable was the efficacy of NIV.
Qualitative variables were expressed as absolute and relative frequencies. Quantitative variables were expressed as mean and standard deviation when they followed a normal distribution that was confirmed using the Kolmogorov–Smirnov test or otherwise as median and interquartile range. For the comparison of qualitative variables, the chi-square test or Fisher’s exact test were used, when appropriate. For the comparison of quantitative variables, the Student t test for independent data with normal distribution was used. The non-parametric Mann–Whitney U test was used when the principle of normalcy was broken. Adjusted odds ratios (OR) with their 95% interval of confidence (95%CI) were estimated using a logistic regression model with entry method including all the variables with P values <.10 in the univariable analysis. This model included the efficacy of NIV, in particular delayed NIV due to improvement, to study how inter-group differences impacted this variable. Differences were considered statistically significant with P values <.05 or when the 95%CI of the OR excluded the value 1. The statistical software used was the SPSS 24.0 statistical package (Inc, Chicago, IL, United States).
The study was conducted in observance of the Declaration of Helsinki. Also, it was approved by Hospital Universitari de Bellvitge clinical research ethics committee, and the participant centers local committees.
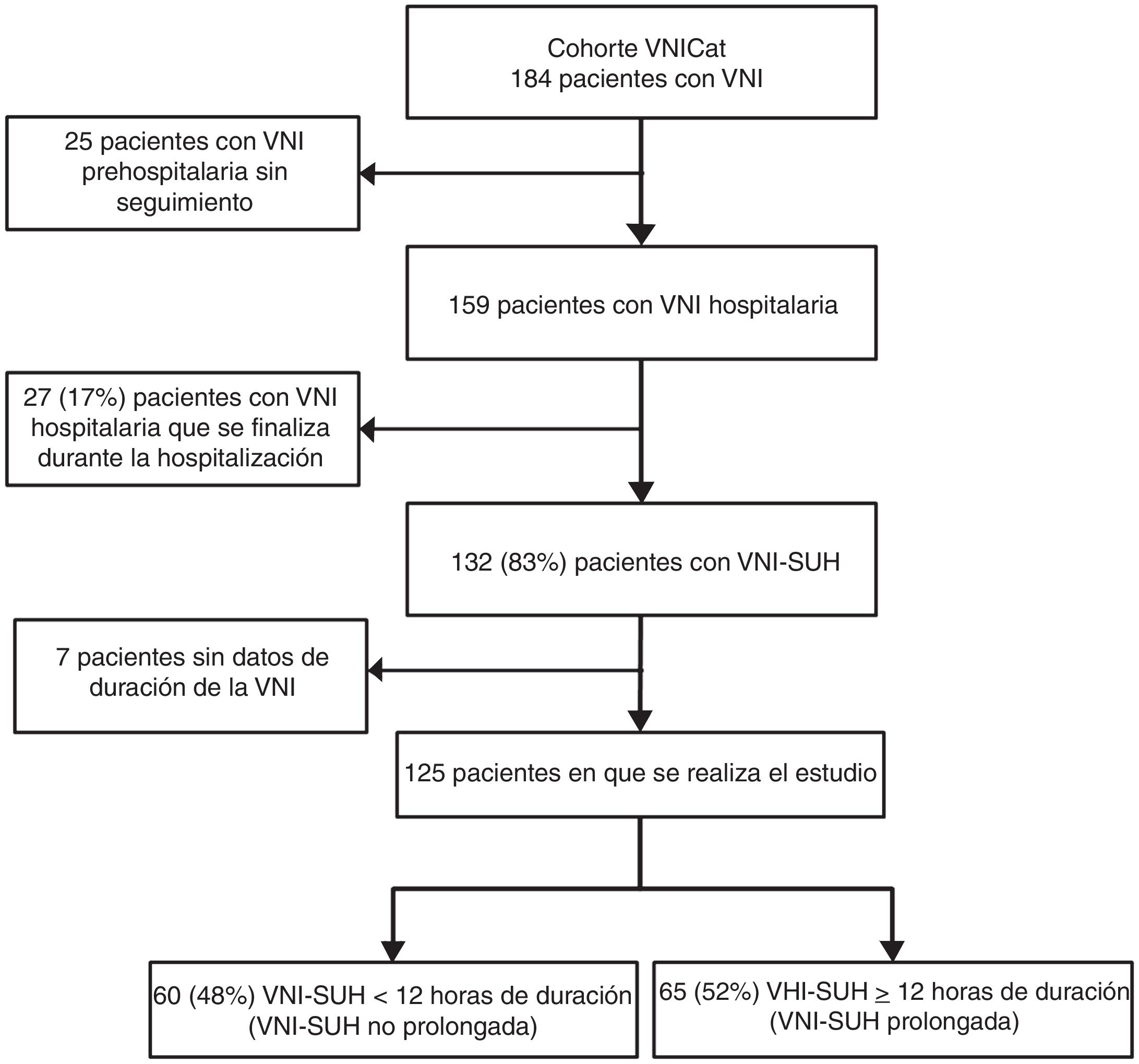
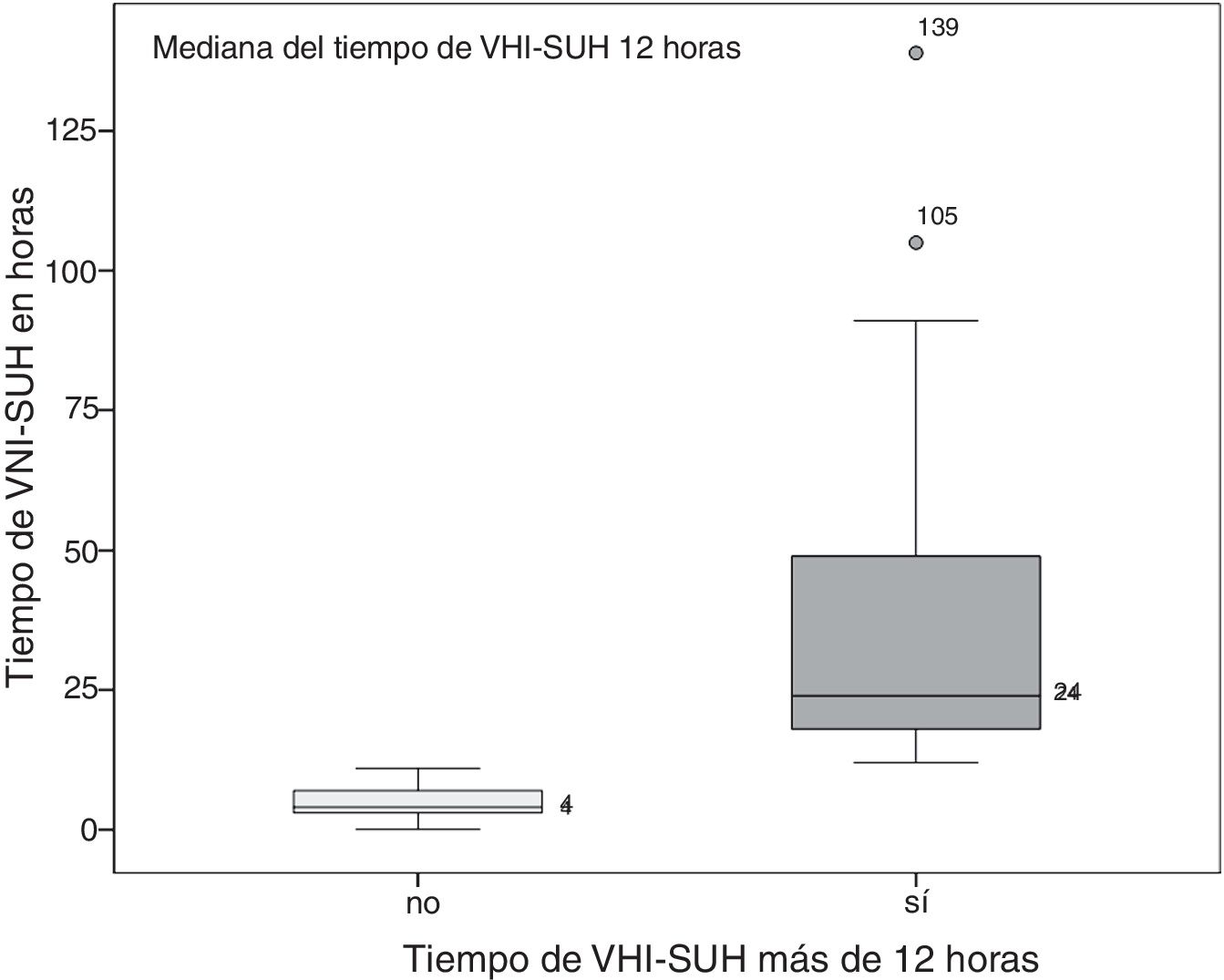
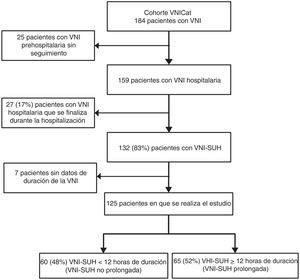
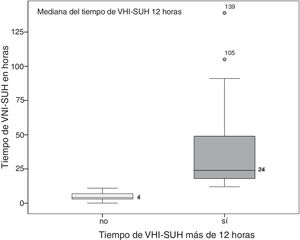
ResultsThe VNICat study collected data from 184 patients treated with NIV, and recruited from 11 hospitals from Catalunya, Spain, and at pre-hospital level, by the SEM. Fig. 1 shows the study flow chart. A total of 25 patients recruited by the SEM at pre-hospital level were excluded. In 132 (83%) out of the 159 patients the NIV was started and finished at the HES setting. The duration of NIV was unknown in 7 patients, which is why they were excluded in the final analysis. The study final cohort ended up including 125 patients and the median time on NIV-HES was 12 h, which is why 2 groups with this cut-off value were created (Fig. 2). One group of 60 patients (48%) on non-prolonged NIV-HES (overall NIV-HES duration <12 h), and another group of 65 patients (52%) on prolonged NIV-HES (overall NIV-HES duration ≥12 h).
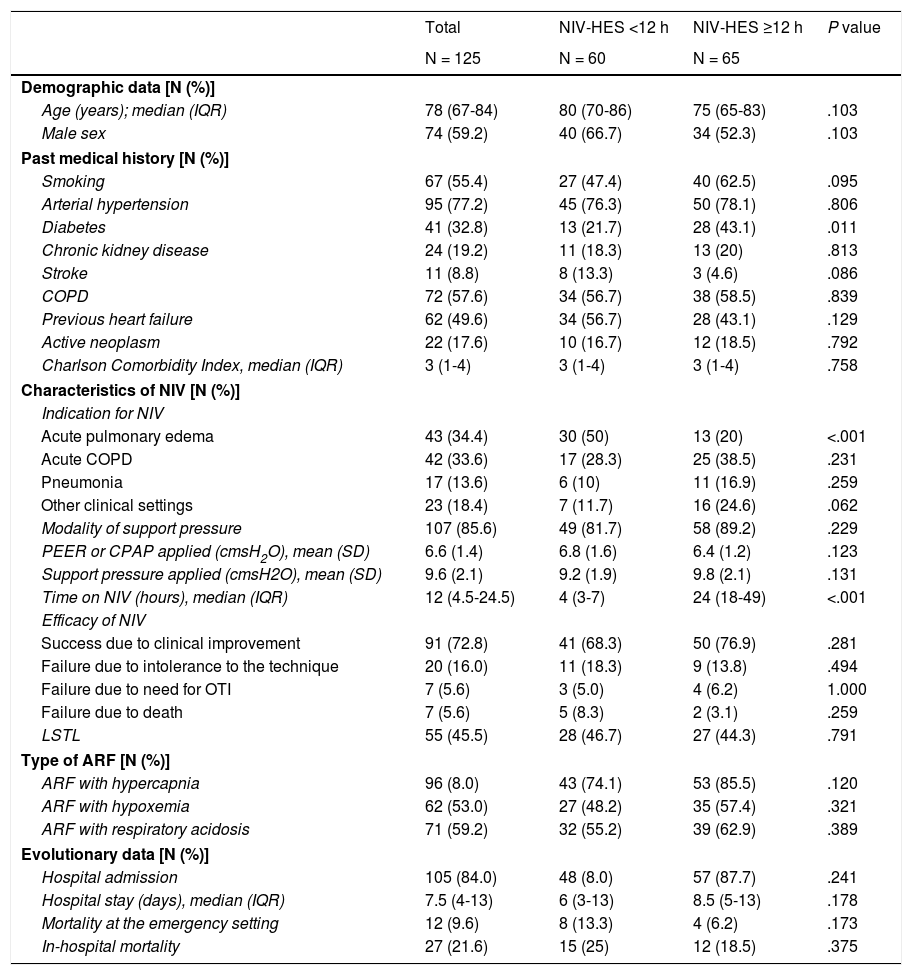
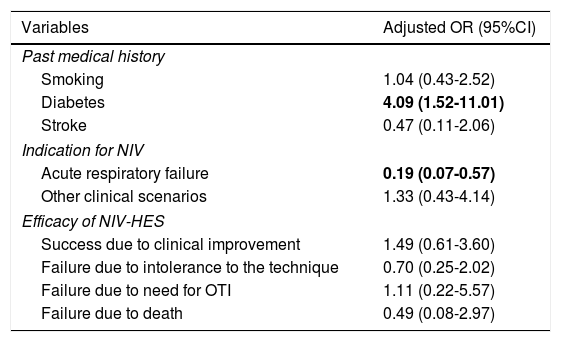
Table 1 shows the overall outcomes and the comparative study based on the duration of NIV-HES. Old age plus a high rate of comorbidities were significant in the overall population. The 2 main indications for NIV-HES were AHF, and COPD (68% combined). In 72.8% of the cases, NIV-HES was successful, and it could be delayed following clinical improvement. The in-hospital mortality rate was 21.6%. The statistically significant differences between the 2 groups on non-prolonged and prolonged NIV-HES were scarce. In patients on prolonged NIV-HES the presence of diabetes was more common, and there were fewer indications for AHF. No differences were reported regarding efficacy or in the success reported due to clinical improvement of 68.3% and 76.9%, respectively or in the in-hospital mortality rate, of 25% and 18.5%, respectively. Table 2 shows the results of the multivariate analysis adjusted by the variables that showed significant differences in the univariate model. Regarding the efficacy of NIV-HES, the variable of prolonged NIV-HES did not seem to play a significant role when adjusted by the differences between the 2 groups or in the success reported due to clinical improvement or in the difference scenarios of failure either.
Univariable analysis of the overall population in whom NIV was removed in the emergency unit, and bivariable analysis based on NIV times ≥12 hours.
| Total | NIV-HES <12 h | NIV-HES ≥12 h | P value | |
|---|---|---|---|---|
| N = 125 | N = 60 | N = 65 | ||
| Demographic data [N (%)] | ||||
| Age (years); median (IQR) | 78 (67-84) | 80 (70-86) | 75 (65-83) | .103 |
| Male sex | 74 (59.2) | 40 (66.7) | 34 (52.3) | .103 |
| Past medical history [N (%)] | ||||
| Smoking | 67 (55.4) | 27 (47.4) | 40 (62.5) | .095 |
| Arterial hypertension | 95 (77.2) | 45 (76.3) | 50 (78.1) | .806 |
| Diabetes | 41 (32.8) | 13 (21.7) | 28 (43.1) | .011 |
| Chronic kidney disease | 24 (19.2) | 11 (18.3) | 13 (20) | .813 |
| Stroke | 11 (8.8) | 8 (13.3) | 3 (4.6) | .086 |
| COPD | 72 (57.6) | 34 (56.7) | 38 (58.5) | .839 |
| Previous heart failure | 62 (49.6) | 34 (56.7) | 28 (43.1) | .129 |
| Active neoplasm | 22 (17.6) | 10 (16.7) | 12 (18.5) | .792 |
| Charlson Comorbidity Index, median (IQR) | 3 (1-4) | 3 (1-4) | 3 (1-4) | .758 |
| Characteristics of NIV [N (%)] | ||||
| Indication for NIV | ||||
| Acute pulmonary edema | 43 (34.4) | 30 (50) | 13 (20) | <.001 |
| Acute COPD | 42 (33.6) | 17 (28.3) | 25 (38.5) | .231 |
| Pneumonia | 17 (13.6) | 6 (10) | 11 (16.9) | .259 |
| Other clinical settings | 23 (18.4) | 7 (11.7) | 16 (24.6) | .062 |
| Modality of support pressure | 107 (85.6) | 49 (81.7) | 58 (89.2) | .229 |
| PEER or CPAP applied (cmsH2O), mean (SD) | 6.6 (1.4) | 6.8 (1.6) | 6.4 (1.2) | .123 |
| Support pressure applied (cmsH2O), mean (SD) | 9.6 (2.1) | 9.2 (1.9) | 9.8 (2.1) | .131 |
| Time on NIV (hours), median (IQR) | 12 (4.5-24.5) | 4 (3-7) | 24 (18-49) | <.001 |
| Efficacy of NIV | ||||
| Success due to clinical improvement | 91 (72.8) | 41 (68.3) | 50 (76.9) | .281 |
| Failure due to intolerance to the technique | 20 (16.0) | 11 (18.3) | 9 (13.8) | .494 |
| Failure due to need for OTI | 7 (5.6) | 3 (5.0) | 4 (6.2) | 1.000 |
| Failure due to death | 7 (5.6) | 5 (8.3) | 2 (3.1) | .259 |
| LSTL | 55 (45.5) | 28 (46.7) | 27 (44.3) | .791 |
| Type of ARF [N (%)] | ||||
| ARF with hypercapnia | 96 (8.0) | 43 (74.1) | 53 (85.5) | .120 |
| ARF with hypoxemia | 62 (53.0) | 27 (48.2) | 35 (57.4) | .321 |
| ARF with respiratory acidosis | 71 (59.2) | 32 (55.2) | 39 (62.9) | .389 |
| Evolutionary data [N (%)] | ||||
| Hospital admission | 105 (84.0) | 48 (8.0) | 57 (87.7) | .241 |
| Hospital stay (days), median (IQR) | 7.5 (4-13) | 6 (3-13) | 8.5 (5-13) | .178 |
| Mortality at the emergency setting | 12 (9.6) | 8 (13.3) | 4 (6.2) | .173 |
| In-hospital mortality | 27 (21.6) | 15 (25) | 12 (18.5) | .375 |
ARF, acute respiratory failure; COPD, chronic obstructive pulmonary disease; CPAP, continuous positive airway pressure; IQR, interquartile range; LSTL, life-sustaining treatment limitation; NIV-HES: noninvasive ventilation at the hospital emergency services; NIV, noninvasive ventilation; OTI, orotracheal intubation; PEEP, positive end-expiratory pressure, SD, standard deviation.
Adjusted odds ratio of the variables associated with prolonged NIV-HES including the efficacy of the technique.
| Variables | Adjusted OR (95%CI) |
|---|---|
| Past medical history | |
| Smoking | 1.04 (0.43-2.52) |
| Diabetes | 4.09 (1.52-11.01) |
| Stroke | 0.47 (0.11-2.06) |
| Indication for NIV | |
| Acute respiratory failure | 0.19 (0.07-0.57) |
| Other clinical scenarios | 1.33 (0.43-4.14) |
| Efficacy of NIV-HES | |
| Success due to clinical improvement | 1.49 (0.61-3.60) |
| Failure due to intolerance to the technique | 0.70 (0.25-2.02) |
| Failure due to need for OTI | 1.11 (0.22-5.57) |
| Failure due to death | 0.49 (0.08-2.97) |
95%CI, 95% confidence interval; NIV-HES: noninvasive ventilation at the hospital emergency services; NIV, noninvasive ventilation; OR, odds ratio; OTI, orotracheal intubation.
The variables in bald were statistically significant.
In half of the cases included in our study, NIV-HES was prolonged for >12 hours. This is not associated with worse efficacy results since it was not associated with a lower success rate of NIV due to improvement of clinical signs. Although no significant differences in comorbidities were reported except for diabetes, we should mention that in non-prolonged NIV-HES, the presence of patients with previous heart failure was more common while in prolonged NIV-HES, the presence of previous COPD was more frequent. This is consistent with the results obtained from the indications for NIV, AHF, and COPD respectively.1 We should mention that in our study, AHF was associated with non-prolonged NIV-HES times. In this clinical scenario we basically have a problem of oxygenation due to pulmonary congestion. Through the application of continuous positive airway pressure or positive end-expiratory pressure, we can achieve alveolar recruitment, thus improving oxygen saturation rapidly; the hemodynamic effects following positive airway pressure, the reduced venous return, right ventricular preload, and left ventricular postload should be added to this mechanism, thus improving cardiac output and myocardial contractility.14,15 Also, medical therapy, usually vasodilators and diuretics, is administered concomitantly to NIV. These agents can solve the AHF. This means that within a few hours the patient’s clinical condition gets better, allowing us to remove NIV very early in time.16 The percentage of patients with COPD is higher in the prolonged NIV-HES group. However, it was surprising to see that no statistically significant association was found since these patients have ventilatory failure and, therefore, require longer times on NIV. The reason for this can be found in the high percentage of patients with COPD in the non-prolonged NIV-HES group. This group patients with decompensated COPD had less ARF with hypoxemia, hypercapnia, and acidosis. This makes us think that this group patients with COPD have gasometric criteria of less severity and, therefore, faster responses, allowing us to remove NIV early.
The closest association of the past medical history of diabetes in patients with prolonged NIV-HES seems irrelevant. However, hyperglycemia is independently associated with worse outcomes in critically ill patients with late failed NIV, and with worse results in patients with ARF with hypercapnia.17–19 Even in patients with acute COPD who do not require NIV, the presence of hyperglycemia has been associated with longer hospital stays and higher in-hospital mortality rates, which may be associated with more respiratory infecctions.20 However, all these associations were not found with the past medical history of diabetes. Unfortunately, in our registry, the glycemia levels at admission were not registered, which is why we cannot put an end to this controversy. However, it seems logical to think that diabetic patients probably had some sort of hyperglycemia at admission.
LSTL was not associated with prolonged NIV-HES, which is surprising in the sense that in this group of patients the palliative and, therefore, prolonged use of NIV should have occurred more often.3 The management of NIV in patients with LSTL depends on the experience of treating physicians and on how the use of NIV is planned. If the patient does not respond properly to NIV and this technique is continued to control dyspnea, then NIV can be prolonged. And on the contrary, if the patient does not improve within the first few hours and this technique is not used palliatively, early weaning from NIV prior to sedation should be expected.
The high percentage of patients with prolonged NIV-HES is challenging. The healthcare personnel rotate significantly at the HES setting. Their training is heterogeneous and requires continuous update to increase significantly the amount of personnel trained to perform this technique and face this prolonged demand in time.21 Also, there is this need to have enough ventilators to perform NIV simultaneously in different patients and, especially, in the winter season and during the seasonal flu epidemic too. NIV means that the healthcare and nursing systems alike will end up overloaded with inadequate or insufficient ratios of NIV most of the times. Poor information disclosure on disease progression and prognosis, and confusing information can occur. In these conditions it is difficult to avoid the uncertainty surrounding the patient and his family.22 For all these reasons, it can be said that prolonged NIV-HES is associated with a lack of efficacy managing this technique, which eventually impacts the final prognosis. However, in our study, we did not find such an association. It seems that the HES that participated in this study really tried from the organizational and training points of view to stop this from happening.
We do not have information on the reasons why there is such a high rate of prolonged NIV-HES. It has been suggested that one of the determinant factors can be the lack of drainage in these patients from the emergency department to other hospital units.3 In some cases, these patients can be eligible for admission at the intensive care unit (ICU) being respiratory problems and the presence of COPD an associated comorbidity common in patients admitted to the ICU setting.23,24 Currently, these units have a high levels of hospital bed occupancy and cannot meet the existing demand all the time.25 We should mention the high number of patients in whom the treating physician identified the presence of LSTL, a situation that eventually leads to fewer admissions to the ICU setting.26 Hospitals can come up with different solutions to solve this problem. Part of the structure of HES can be used as an intermediate care unit or a brand new intermediate care unit structure can be created or even support through resources like extended ICUs can be given.27,28 The use of intermediate care units has been studied extensively. These units allow continuous monitoring, as well as the safe administration of vasoactive drugs and NIV.29 Also, more specialized units like intermediate respiratory care units have become available these days being the need for NIV the main justification for the existence of these units. They not only stop ICU admissions from happening, but also promote drainage in these units, thus becoming an efficient alternative.30–32 One of the purposes of extended ICUs is to detect patients who can get worse, initially at the hospital floors. However, we believe that this can be an interesting resource that should be implemented at the HES setting since it facilitates the shared and agreed decision-making process. This, in turn, allows us to make better transitions if the patient finally needs to be admitted to the ICU. HES have the capacity to initiate NIV early and properly. Hospitals have the capacity to facilitate the drainage and transition of these patients outside the HES setting. The best thing to do would be to integrate the different actors involved in the administration of NIV.
Our study has limitations. The sample size was small, and the group of hospitals included had different structures and resources available. However, this heterogeneity reflects the actual situation of HES where the care provided to patients with ARF who require NIV can take place in hospitals of different characteristics and regardless of their complexity and resources available. This variability also affects drainage from the HES to the hospital floor since not all hospitals withstand the same emergency pressure. There is no such thing as standardization in the referral or drainage circuits of patients from the HES setting to hospital units. That is why in certain hospitals it can be easier to admit patients to the ICU or intermediate care settings, when available. However, the high percentage of patients who finish their NIV at the HES setting seems to respond to a generalized and homogeneous behavior regardless of the treating hospital. An important limitation of our study is that neither clinical nor gasometric evolutionary data were included. These data can identify groups of patients with poor disease progression who have more chances of failed technique or prolonged NIV-HES. The fact that efficacy was similar in both groups of patients is not indicative that evolutionary data were very different between both groups since these data are the ones that better identify failed techniques.
As a conclusion to our study, we can say that prolonged NIV-HES is something common. However, it is associated with a low rate of efficacy regarding the technique. The flows of these patients need to be standardized based on the resources available to guarantee proper referrals from the HES.
Authors’ contributionsAuthors have contributed the follow way:
María Arranz: study design, data mining from the center, outcome assessment, and manuscript preparation.
Javier Jacob: study design, data mining from the center, outcome assessment, data statistical analysis, and manuscript preparation.
Mariona Sancho-Ramoneda: study design, data mining from the center, outcome assessment, and manuscript preparation.
Àngels Lopez: study design, data mining from the center, outcome assessment, data statistical analysis, and manuscript preparation.
M. Carmen Navarro-Sáez: study design, data mining from the center, outcome assessment, data statistical analysis, and manuscript preparation.
Jose Ramon Cousiño-Chaoa: study design, data mining from the center, outcome assessment, data statistical analysis, and manuscript preparation.
Xavier López-AltimARFs: study design, data mining from the center, outcome assessment, data statistical analysis, and manuscript preparation.
Francesc López i Vengut: study design, data mining from the center, outcome assessment, data statistical analysis, and manuscript preparation.
Olivia García-Trallero: study design, data mining from the center, outcome assessment, data statistical analysis, and manuscript preparation.
Antonio German: study design, data mining from the center, outcome assessment, data statistical analysis, and manuscript preparation.
Jaume Farré-Cerdà: study design, data mining from the center, outcome assessment, data statistical analysis, and manuscript preparation.
Jose Zorrilla: study design, data mining from the center, outcome assessment, data statistical analysis, and manuscript preparation.
Conflicts of interestNone reported.
Please cite this article as: Arranz M, Jacob J, Sancho-Ramoneda M, Lopez À, Navarro-Sáez MC, Cousiño-Chao JR, et al. Características de la ventilación no invasiva prolongada en los servicios de urgencias hospitalarios y su impacto en la eficacia. Análisis del registro VNICat. Med Intensiva. 2021;45:477–484.