Ultrasound has become an essential tool in assisting critically ill patients. Its knowledge, use and instruction require a statement by scientific societies involved in its development and implementation.
Our aim is to determine the use of the technique in intensive care medicine, clinical situations where its application is recommended, levels of knowledge, associated responsibility and learning process also implement the ultrasound technique as a common tool in all intensive care units, similar to the rest of European countries.
The SEMICYUC's Working Group Cardiac Intensive Care and CPR establishes after literature review and scientific evidence, a consensus document which sets out the requirements for accreditation in ultrasound applied to the critically ill patient and how to acquire the necessary skills.
Training and learning module requires a structured process within the specialty. The SEMICYUC must agree to disclose this document, build relationships with other scientific societies and give legal cover through accreditation of the training units, training courses and different levels of training.
La ecografía se ha convertido en un instrumento imprescindible en la asistencia a los pacientes críticos. Su conocimiento, uso e instrucción requiere un posicionamiento por parte de las sociedades científicas implicadas en su desarrollo y aplicación.
Nuestros objetivos son determinar el uso de la técnica dentro de Medicina Intensiva, las situaciones clínicas donde su aplicación es recomendable, los niveles de conocimiento, la responsabilidad asociada y el proceso de aprendizaje, así como convertir la técnica ecográfica en una herramienta de uso habitual en todas las unidades de cuidados intensivos, en concordancia con el ámbito europeo que nos rodea, para su integración y homologación.
El Grupo de Trabajo de Cuidados Intensivos Cardiológicos y RCP de la SEMICYUC establece, tras revisión bibliográfica y evidencia científica, un documento de consenso donde se establecen los requisitos necesarios para la acreditación en ecografía aplicada al paciente crítico y adquirir las competencias necesarias.
El aprendizaje exige un proceso estructurado dentro de la especialidad. La SEMICYUC debe comprometerse a divulgar este documento, establecer relaciones con otras sociedades científicas y dar cobertura legal mediante acreditación de las unidades formativas, cursos y niveles de capacitación.
Ultrasound (US) is a noninvasive technique that offers an image of body organs and vessels for diagnostic and/or therapeutic purposes. It presents limitations depending on the indication, the technical capacity of the operator, the quality of the data obtained, and the decisions made.
The actions taken as a result of poor interpretation of the exploration can have adverse consequences for the patient. Likewise, failure to use the technique for diagnoses or invasive procedures may imply an unnecessary risk for the patient that can have legal consequences for the physician. Use of the technique implies adequate training.
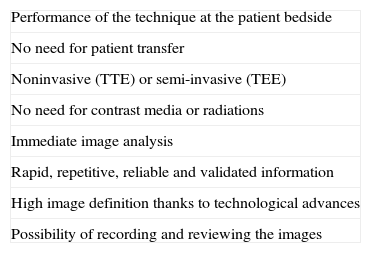
Critical patients generally present a series of clinical particularities in which morphological and functional ultrasound evaluation proves essential due to its noninvasiveness, reliability, validity and applicability at the patient bedside (Table 1).There is extensive literature supporting the use of the technique in critically ill patients.1–5
Advantages of ultrasound in critical patients.
| Performance of the technique at the patient bedside |
| No need for patient transfer |
| Noninvasive (TTE) or semi-invasive (TEE) |
| No need for contrast media or radiations |
| Immediate image analysis |
| Rapid, repetitive, reliable and validated information |
| High image definition thanks to technological advances |
| Possibility of recording and reviewing the images |
TEE: transesophageal echocardiography; TTE: transthoracic echocardiography.
The Spanish Society of Intensive and Critical Care Medicine and Coronary Units (Sociedad Española de Medicina Intensiva, Crítica y Unidades Coronarias, SEMICYUC) has the responsibility, duty and obligation to ensure that the procedures used in critical patients are carried out safely and correctly as regards their indication, quality and the technical knowledge of the operators, based on the implementation of an accredited training program.
In this context, the SEMICYUC should promote the use of ultrasound, facilitating its adoption as a routine tool, as well as correct training in the technique, with a view to ensuring that most Units have access to these procedures and that critical patients are treated and monitored effectively, adequately and safely. However, no widely recognized guidelines have been established to date, and only a few isolated national initiatives have developed rules for training in ultrasound among non-cardiologists who perform explorations in different settings,6–9 and particularly in Intensive Care.9
Of the possible clinical situations in which echocardiography may be indicated10 (about 200), over 50% are found in the Emergency Care area and in Intensive Care Units (ICUs).
MethodsThe Cardiological Intensive Care and Cardiopulmonary Resuscitation Work Group of the SEMICYUC (GTCIC y RCP), on occasion of its XXVII meeting held in 2010 in Sabadell (Spain), decided to draft a consensus document supported by the most recent scientific evidence based on a search of the United States National Institute of Health, National Library of Medicine – MEDLINE, and recruiting the broadest national representation of intensivists with extensive experience and knowledge of ultrasound. During this period, it proved possible to increase the number of authors collaborating in the initial draft, which in turn was presented in the scientific meetings of Segovia in 2011, Santander and Madrid in 2012, and Tenerife in 2013, until its definitive presentation for publication.
This consensus document describes the characteristics of ultrasound in general and of echocardiography in particular, in reference to the management of critical patients. The ultrasonographic studies are delimited according to levels and the recordings included, with consideration of the training needed by non-cardiological specialists in order to acquire the necessary skills.
One of the aspects in which maximum consensus was gained in our group was the notion that general ultrasound training in Critical Care Medicine and training in basic echocardiography should start during residency training. Furthermore, it should range from “first sight” exploration and the concept of discarding life-threatening disease (“rule-in versus rule-out”) to more precise and specific evaluations. The topics addressed in general ultrasound training in Critical Care Medicine are pleuropulmonary ultrasound, vascular ultrasound, transcranial duplex imaging and ultrasound in the context of different protocols: focused assessment with sonography in trauma (FAST), focused cardiac ultrasound (FOCUS), focused ultrasound and echocardiography (FUSE), focused assessment with transthoracic echocardiography (FATE), and focused echocardiography evaluation in life support (FEEL).
On an independent basis, advanced echocardiography allows detailed evaluation of the anatomy of the heart and of patient hemodynamics, using transthoracic echocardiography (TTE) and transesophageal echocardiography (TEE). Training in this area requires the necessary skills in ultrasound, Doppler-color and Doppler-tissue imaging, and the capacity to establish clinicopathological correlations with a view to adequately interpreting the more complex clinical conditions.
General ultrasound and basic echocardiographyTwo concepts have recently been developed that are of help in learning the application and usefulness of these techniques in the management of critical patients, specifically in the context of Intensive Care Medicine.
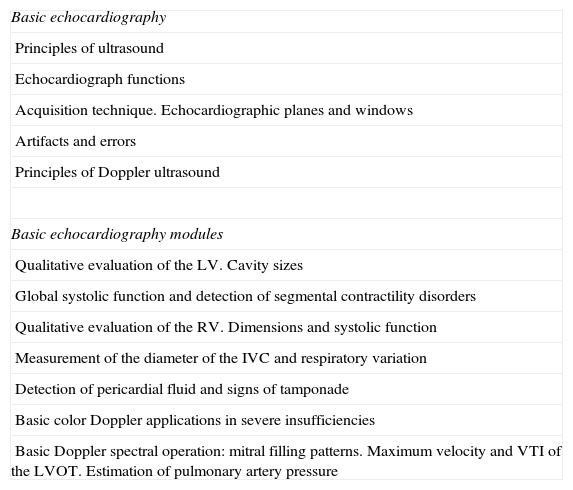
One of the concepts is so-called point-of-care ultrasonography, corresponding to real-time ultrasound used to obtain dynamic recordings that can be immediately correlated to the clinical condition of the patient and to the findings of the physical examination, and which moreover can be repeated in the event of any change in the patient condition or in the treatment provided.11 The characteristics of our medical specialty offer multiple applications for ultrasonography. Some of them are already well established, such as transcranial duplex ultrasound in neurocritical care, though the field of application has been extended to many other areas ranging from diagnostic or screening uses such as abdominal11 or pleuropulmonary ultrasound,12,13 to guidance in procedures such as central catheter placement,14,15 pericardial drainage, or the drainage of pleural collections. The modality with the greatest clinical application is the anatomical and functional study of the heart and major vessels using basic echocardiography techniques (Tables 2 and 3).
Basic echocardiography training program.
| Basic echocardiography |
| Principles of ultrasound |
| Echocardiograph functions |
| Acquisition technique. Echocardiographic planes and windows |
| Artifacts and errors |
| Principles of Doppler ultrasound |
| Basic echocardiography modules |
| Qualitative evaluation of the LV. Cavity sizes |
| Global systolic function and detection of segmental contractility disorders |
| Qualitative evaluation of the RV. Dimensions and systolic function |
| Measurement of the diameter of the IVC and respiratory variation |
| Detection of pericardial fluid and signs of tamponade |
| Basic color Doppler applications in severe insufficiencies |
| Basic Doppler spectral operation: mitral filling patterns. Maximum velocity and VTI of the LVOT. Estimation of pulmonary artery pressure |
VTI: velocity–time integral; LVOT: left ventricular outflow tract; IVC: inferior vena cava; RV: right ventricle; LV: left ventricle.
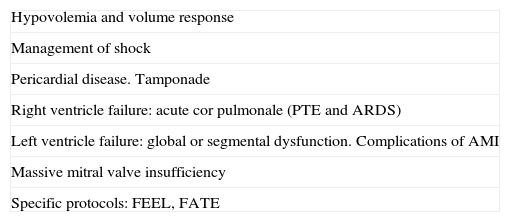
Clinical applications.
| Hypovolemia and volume response |
| Management of shock |
| Pericardial disease. Tamponade |
| Right ventricle failure: acute cor pulmonale (PTE and ARDS) |
| Left ventricle failure: global or segmental dysfunction. Complications of AMI |
| Massive mitral valve insufficiency |
| Specific protocols: FEEL, FATE |
FATE: focused assessment with transthoracic echocardiography; FEEL: focused echocardiography evaluation in life support; AMI: acute myocardial infarction; ARDS: adult respiratory distress syndrome; PTE: pulmonary thromboembolism.
Based on the recommendations of Mayron et al.,16 protocols such as FUSE and FOCUS have been developed,17,18 defined as anatomical of physiological echocardiography aimed at answering a specific question and/or guiding a procedure, and performed by a competent physician with knowledge of the technique.
Focused echocardiography evaluation in life supportFocused echocardiography evaluation in life support (FEEL)19 is a diagnostic tool used during cardiopulmonary resuscitation (CPR).20 It is recommended in the 2010 guides of the American Heart Association/European Resuscitation Council/International Committee on Resuscitation, focusing on high-quality CPR with minimum interruption in order to reduce the no-flow episodes.21
The aim of the FEEL protocol is to diagnose or discard potentially treatable causes of cardiac arrest, including tamponade, massive pulmonary embolism, severe ventricular dysfunction and hypovolemia, as well as fine ventricular fibrillation not diagnosed by surface electrocardiography (ECG)–thereby optimizing peri-CPR patient resuscitation.
Focused assessment with transthoracic echocardiographyThe FATE protocol, developed in the last 15 years, allows us to make decisions in a fast and easy manner, in patient life-threatening situations. The learning process is simple. FAST fundamentally involves thoracic exploration, including three cardiac images (subcostal, apical and parasternal) and an image of the pleura, in a rapid sequence, with the following objectives:
- 1.
Confirming the absence of evident disease.
- 2.
Evaluating wall thickness and cavity dimensions.
- 3.
Evaluating contractility.
- 4.
Visualizing the pleura on both sides.
- 5.
Correlating the information to the clinical context.
The general objective is to detect life-threatening conditions and obtain information on heart volumes and contractility.
Focused assessment with sonography in traumaThe FAST protocol was developed for the exploration of trauma patients, and forms part of the Advanced Trauma Life Support protocol developed by the American College of Surgeons.22 It initially centers on the abdomen. Although ultrasound does not offer 100% sensitivity in identifying all cases of bleeding, it is very useful for identifying intraperitoneal bleeding in hypotensive patients requiring urgent laparotomy, and for the diagnosis of cardiac damage in penetrating traumatisms. Recent studies have shown the FAST protocol to be equivalent to or even better (in experienced hands) than chest X-rays in identifying pneumothorax or hemothorax in trauma patients.
The objectives of FAST are:
- 1.
Identification of free fluid (intraperitoneal, pericardial).
- 2.
Guiding of decisions in the resuscitation of trauma patients, based on the ultrasound findings and hemodynamic condition of the patient.
General ultrasound and basic echocardiography also includes other explorations, such as pleuropulmonary ultrasound, vascular ultrasound and duplex cranial sonography, which are dealt with below.
Pleuropulmonary ultrasoundUltrasound is extraordinarily useful for the daily management of pleuropulmonary disease. It is the best technique for the detection of pleural effusion, but is also superior to X-rays in discarding pneumothorax,23 which may be radiologically occult, and in the evolutive follow-up of condensations due to pneumonia and atelectasis.24,25 Ultrasound complements the hemodynamic information supplied by echocardiography, with the assessment of the extravascular lung water, and informs of lung aeration in multiple diseases.26–28
The approach to thoracic ultrasound is different from that of abdominal ultrasound or echocardiography. The images do not correspond to any recognizable structure; rather, the tissue echoes generate artifacts. In pulmonary ultrasound we visualize horizontal or vertical lines, and due training is required to recognize what they represent, and to distinguish among them in order to avoid mistakes.
Vascular ultrasoundThe main applications of vascular ultrasound in the critical patient are guidance in arterial or venous vascular catheter puncture and insertion, and in the diagnosis of venous thromboses.
Whenever possible, ultrasound-guided puncture is advised, since it allows us to determine the position of the vein and its anatomical relations, and to discard complications associated to venous thrombosis.29,30 In this sense, direct visualization with ultrasonography allows easy, rapid and safe catheterization.
Many studies offer sufficient evidence for recommending central venous catheter (CVC) insertion under ultrasound guidance, and the technique has been incorporated to many clinical practice and patient safety guides.31,32 Under these circumstances, arterial insertion guided by ultrasound is fully recommended.33,34
Cranial duplex ultrasoundThe morphological and functional analysis of the cranium using low-frequency ultrasound was introduced as a diagnostic technique in patients with acute neurological disease.35,36 This procedure, known as transcranial color-coded duplex ultrasonography, has recently been introduced in ICUs. It allows structural evaluation of the brain parenchyma, and the location and study of vessels pertaining to the circle of Willis. The new generation systems even allow a semiquantitative analysis of brain perfusion.37
Advanced echocardiographyWithout neglecting the contribution of other procedures, advanced echocardiography in the ICU aims to address several key issues in clinically unstable patients–assessing the underlying etiology, determining the hemodynamic profile and identifying the principal elements causing instability, with the selection of adequate initial treatment, and evaluation of the degree of response to the decision made.
Acquiring the necessary skills requires mastery of the morphological and functional analysis of the transthoracic exploration (TTE), including Doppler ultrasound. Such skills must be summed to knowledge of the possible cardiac functional repercussions of extrinsic factors including mechanical ventilation, inotropic drug support, extrarenal filtration techniques, etc. (Tables 4 and 5).
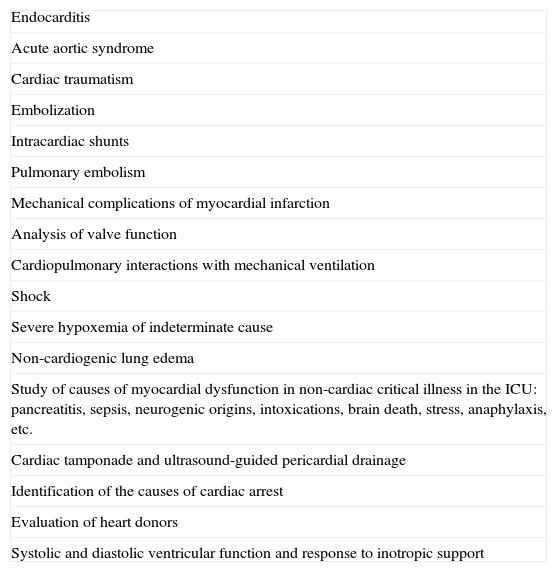
Indications of advanced echocardiography.
| Endocarditis |
| Acute aortic syndrome |
| Cardiac traumatism |
| Embolization |
| Intracardiac shunts |
| Pulmonary embolism |
| Mechanical complications of myocardial infarction |
| Analysis of valve function |
| Cardiopulmonary interactions with mechanical ventilation |
| Shock |
| Severe hypoxemia of indeterminate cause |
| Non-cardiogenic lung edema |
| Study of causes of myocardial dysfunction in non-cardiac critical illness in the ICU: pancreatitis, sepsis, neurogenic origins, intoxications, brain death, stress, anaphylaxis, etc. |
| Cardiac tamponade and ultrasound-guided pericardial drainage |
| Identification of the causes of cardiac arrest |
| Evaluation of heart donors |
| Systolic and diastolic ventricular function and response to inotropic support |
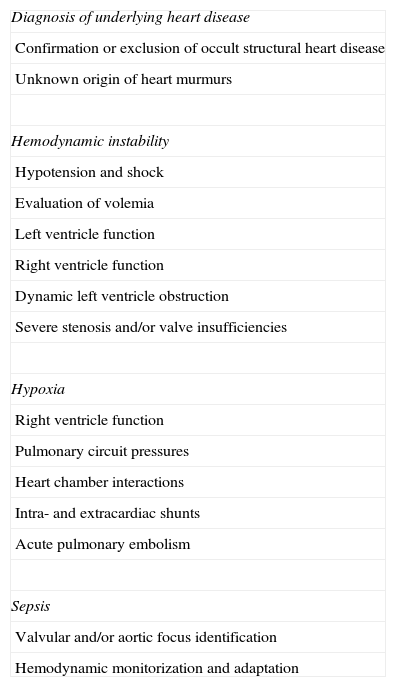
Common uses of echocardiography in the Intensive Care Unit.
| Diagnosis of underlying heart disease |
| Confirmation or exclusion of occult structural heart disease |
| Unknown origin of heart murmurs |
| Hemodynamic instability |
| Hypotension and shock |
| Evaluation of volemia |
| Left ventricle function |
| Right ventricle function |
| Dynamic left ventricle obstruction |
| Severe stenosis and/or valve insufficiencies |
| Hypoxia |
| Right ventricle function |
| Pulmonary circuit pressures |
| Heart chamber interactions |
| Intra- and extracardiac shunts |
| Acute pulmonary embolism |
| Sepsis |
| Valvular and/or aortic focus identification |
| Hemodynamic monitorization and adaptation |
One of the main inconveniences of echocardiography in the ICU is the difficulty of securing an adequate acoustic window (due to interference by invasive and noninvasive mechanical ventilation, mobilization difficulties, bandages and thoracic drain devices, etc.), as well as its dependence upon operator experience. TEE largely resolves the difficulties of securing an adequate acoustic window. This is a semi-invasive technique in which the proximity of the esophagus to the cardiac structures allows the use of high-frequency probes affording high resolution, and offers a window in which images of the heart and major vessels can be obtained with a great increase in resolution with respect to TTE (Table 6). Likewise, TEE allows us to visualize areas of the heart that are not accessible to conventional ultrasound. The explorations made yield a high percentage of adequate images in critical patients, and the usefulness of the technique justifies the need for intensivists to acquire skills in the use of TEE.38
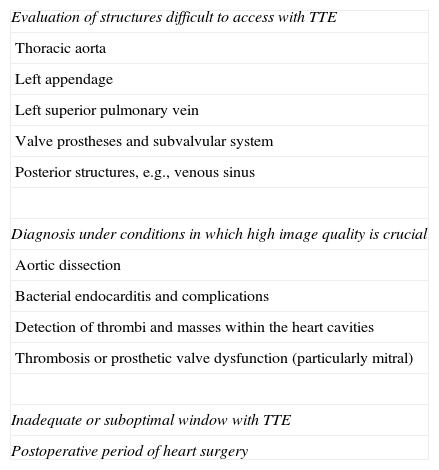
Advantages and indications of transesophageal echocardiography in the Intensive Care Unit.
| Evaluation of structures difficult to access with TTE |
| Thoracic aorta |
| Left appendage |
| Left superior pulmonary vein |
| Valve prostheses and subvalvular system |
| Posterior structures, e.g., venous sinus |
| Diagnosis under conditions in which high image quality is crucial |
| Aortic dissection |
| Bacterial endocarditis and complications |
| Detection of thrombi and masses within the heart cavities |
| Thrombosis or prosthetic valve dysfunction (particularly mitral) |
| Inadequate or suboptimal window with TTE |
| Postoperative period of heart surgery |
TTE: transthoracic echocardiography.
To date, few countries have developed specific training programs in critical patients. However, recently a full list has been published of the ultrasound skills required of intensivists, embodied in a “Declaration of Competencies” developed by two critical care societies.39 These skills or competencies encompass abdominal, thoracic and vascular ultrasound (General Critical Care Ultrasound), as well as echocardiography in critical care (Critical Care Echocardiography).
Likewise, the objective of the European CoBaTrICE (Competency-Based Training in Intensive Care) project, headed by the European Society of Intensive Care Medicine, with the participation of the SEMICYUC, is to develop an internationally accepted training program based on the development of competencies and with the principal purpose of harmonizing training.40
In Domain 2 (diagnosis, evaluation, investigation, monitorization and data interpretation), the CoBaTrICE describes the knowledge and indications for performing TTE and TEE as assessment, monitorization and investigation tools in the critical patient.
The competencies of intensivists in ultrasound are considered to include not only knowledge of the indications of echocardiography in the critical patient, but also the ability to perform and interpret echocardiographic studies,41,42 and consensus has been established regarding the training needed to reach different levels or grades of competency.43
Training in ultrasound should be protocolized and supervised according to the guidelines of the training programs referred to each of the specialties, and concordant with the European setting. In this context it is reasonable to follow the recommendations established on occasion of the congress of the European Society of Intensive Care Medicine in Vienna, in 2009, within the setting of a meeting held among different national associations (International Expert Statement on Training Standards for Critical Care Ultrasonography).44
A structured certification program is probably the best approach for standardizing professionals with the required skills and knowledge. Although from a medical-legal aspect competence is more relevant than certification, the latter is of great help in establishing a minimum and correct standard of practice.
Levels of training in ultrasoundIn discussing the training levels, the work group considered that capacitation in ultrasound should contemplate different levels, each with concrete objectives acquired on a progressive basis, as detailed below.
Basic level proposal (Level I)Level I comprises theoretical and practical training, including awareness of the diagnostic options available in different clinical situations; technical aspects of the ultrasound system; the physics of ultrasound; cardiovascular anatomy and the acquisition of echocardiographic planes through different acoustic windows; knowledge of the different echocardiography modes, including the theoretical basis of TEE and the different disease conditions that can modify cardiac anatomy and function; recognition of the most frequent disease conditions; and final drafting of a report. The aim is to qualitatively evaluate a limited number of frequent problems allowing a rapid tentative diagnosis, followed by confirmation using computed axial tomography (CAT) or advanced TEE or TTE. This level includes basic training in pleuropulmonary ultrasound, vascular accesses, abdominal ultrasound, and transcranial duplex imaging. The theoretical program has a minimum duration of 20hours, including 14hours of theoretical training in general ultrasound and basic echocardiography (divided among clinical cases and sessions), and 6hours of practice with echographic systems.
The minimum number of explorations or studies made in order to ensure the required training in basic echocardiography has been established as approximately 30 supervised studies. These studies are to be made in an accredited unit, and should contain teaching aspects applied to routine clinical practice. Each “candidate” is to present a study log reflecting the activities carried out, including the reports that have been drafted, interpreted, notified and validated by an accredited supervisor. Training in this phase can be performed both in the echocardiography unit and in the ICU. A final examination is carried out, and the diploma awards a number of training credits.
Concrete objectives:
- 1.
Knowledge of ultrasound systems and probes.
- 2.
Two-dimensional echocardiography and the M-mode. Knowledge and correct plane acquisition. Recognition of normal dimensions.
- 3.
Cardiac Doppler ultrasound.
- 4.
Semiquantitative evaluation of left and right ventricular functions. Assessment of volemia.
- 5.
Identification of acute pericardial and pleural disease. Puncture guide.
- 6.
Semiquantitative evaluation of severe valve dysfunction.
- 7.
Venous catheterization guide and FAST abdominal ultrasound and pleuropulmonary ultrasound.
Level II (advanced echocardiography) is characterized by knowledge and control of all aspects related to TTE, not only image acquisition and quantitative measurements, but also the application of Doppler techniques, knowledge of the transesophageal technique (TEE), and the specific indications in the critical patient. This level in turn is subdivided into Levels IIa and IIb.
Level IIa implies knowledge and the diagnosis of most of the cardiovascular alterations found in the ICU. The aim is to be able to establish a firm diagnosis, interpret the findings and correlate them to the clinical picture, and to make decisions allowing posterior adoption of a therapeutic strategy. Level IIb in turn is dedicated to the study of specific conditions in ICUs, the use of ultrasound as a monitoring tool, furthering of the knowledge gained, and the use of TEE. The Level IIb studies are to be carried out in Critical Care Units.
The theoretical training should be as interactive as possible, using illustrative cases with recorded typical images. The minimum duration of these courses should be 40hours, distributed between theoretical sessions and didactic cases. The training is acquired by rotation through an accredited ICU, and under qualified supervision for the acquisition of skills in TTE and TEE. The literature reflects a minimum number of 150 supervised TTE studies at each level, with between 30 and 50 TEE studies. However, the current tendency is to evaluate the acquisition of competencies, rather than to simply count of how many explorations or procedures have been carried out.
It is advisable to base training not only on a number of studies but also on the existence of sufficient diversity of the clinical cases in order to ensure more complete and thorough learning. The studies should include the clinical scenario for correct interpretation.
Each “candidate” is to present a study log reflecting the activities carried out, including the reports that have been drafted and notified, together with the interpretation of images, to be validated by the supervisor.
The advanced level requires due certification or accreditation. Levels IIa and IIb can be reached simultaneously, and allow the conduction of studies and reports on an autonomous basis. The accredited centers will supply all the audiovisual and theoretical materials needed. The studies should be recorded, with a final practical–theoretical examination.
Level III proposalLevel III does not imply a higher level of training, but does mean that skill is demanded in developing research protocols in specific disease in the ICU, in cardiovascular physiology and, in general, in developing the previous level with a view to subsequently allowing the training of others. This level includes the performance of special echocardiographic techniques in the critical patient.
ConclusionsThe SEMICYUC should be committed to diffusing this document, establishing relations with other scientific societies, and affording legal coverage through accreditation of the training units, courses, and levels of competency.
It is the hope of the authors for the document to have national as well as international projection (through American societies which have the SEMICYUC as reference), and to position the SEMICYUC for subsequent agreements with the work groups other societies such as the Spanish Society of Cardiology, the Spanish Society of Internal Medicine (SEMI), the Spanish society of Anesthesia, Resuscitation and Pain Management, and the Spanish Society of Emergency Care Medicine.
An expanded version is available on the SEMICYUC website.
Conflicts of interestThe authors declare that they have no conflicts of interest.
Please cite this article as: Ayuela Azcárate JM, Clau-Terré F, Vicho Pereira R, Guerrero de Mier M, Carrillo López A, Ochagavia A, et al. Documento de consenso para la formación en ecografía en Medicina Intensiva. Proceso asistencial, uso de la técnica y adquisición de competencias profesionales. Med Intensiva. 2014;38:33–40.