Edited by: Federico Gordo. Intensive Care Service of Hospital of Henares, Madrid, Spain
Last update: April 2025
More infoHealthcare professionals working in the Intensive Care Unit (ICU) care for patients suffering from a critical illness and their relatives. Working within a team of people with different personalities, competencies, and specialties, with constraints and demands might contribute to a working environment that is prone to conflicts and disagreements. This highlights that the ICU is a stressful place that can threaten healthcare professionals’ wellbeing. This article aims to address the concept of wellbeing by describing how the stressful ICU work-environment threatens the wellbeing of health professionals and discussing how this situation jeopardizes patient safety. To promote wellbeing, it is imperative to explore actionable interventions such as improve communication skills, educational sessions on stress management, or mindfulness. Promoting ICU healthcare professionals’ wellbeing through evidence-based strategies will not only increase their personal resilience but might contribute to a safer and more efficient patient care.
Los profesionales sanitarios que trabajan en la Unidad de Cuidados Intensivos (UCI) cuidan de pacientes que sufren una enfermedad grave y de sus familiares. Trabajar en un equipo de personas con diferentes personalidades, competencias y especialidades, con limitaciones y exigencias, puede contribuir a crear un entorno de trabajo propenso a conflictos y desacuerdos. Esto pone de manifiesto que la UCI es un lugar estresante que puede amenazar el bienestar de los profesionales sanitarios. Este artículo pretende abordar el concepto de bienestar describiendo cómo el estresante entorno laboral de las UCI amenaza el bienestar de los profesionales sanitarios y debatiendo cómo esta situación pone en peligro la seguridad de los pacientes. Para promover el bienestar, es imperativo explorar intervenciones viables como mejorar las habilidades de comunicación, sesiones educativas sobre gestión del estrés o mindfulness. Promover el bienestar de los profesionales sanitarios de la UCI mediante estrategias basadas en la evidencia no sólo aumentará su resiliencia personal, sino que podría contribuir a una atención al paciente más segura y eficiente.
An Intensive Care Unit (ICU) is a demanding and stressful work environment for healthcare professionals. Long working hours, challenging workload with life-threatening conditions of patients, and managing conflicts with co-workers and patients’ relatives might result in work-related stress among ICU professionals.1,2 There is a growing interest in promoting healthcare professionals’ wellbeing. Resilient, healthy, and engaged healthcare professionals are more productive and less likely to leave their job or be off sick.3 However, what does ‘wellbeing’ mean and how is this linked to work-related stress in an ICU and influence patient safety? Therefore, the focus of this paper is to address the concept of wellbeing, to described how the stressful ICU working environment influence the wellbeing of health professionals, and to discuss how this situation jeopardizes patient safety.
Wellbeing of healthcare professionalsWellbeing is the keyword in the World Health Organization’s (WHO) definition of health: “a state of complete physical, mental and social wellbeing and not merely the absence of disease or infirmity”.4 In particular, the WHO identifies mental health as “state of wellbeing in which an individual realizes his or her own abilities, can cope with the normal stresses of life, can work productively and is able to make a contribution to his or her community”.4
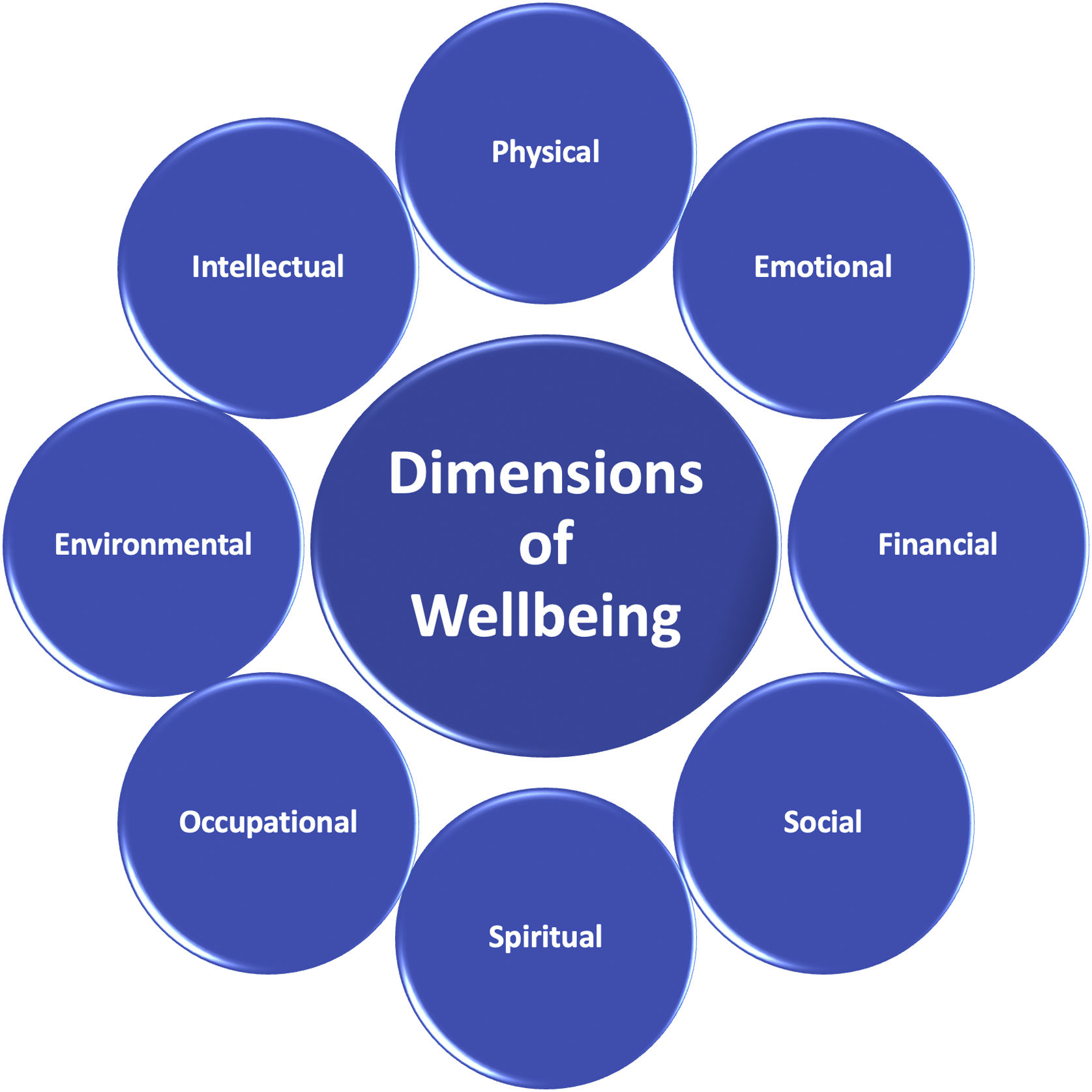
Wellbeing is a complex concept, which varies according to the context and the individual.5 It relates to a wide range of dimensions (Fig. 1). More than twenty years ago, Ryff et al.5–7 started to study wellbeing. They developed a six-factor model of psychological wellbeing which determines six factors that contribute to an individual’s psychological wellbeing, contentment, and happiness. This model of psychological wellbeing differs from past models in one important way: wellbeing is multidimensional, and not merely about happiness, or positive emotions. According to this model, psychological wellbeing consists of:5
- •
Self-acceptance: a persisting positive and acceptant attitude toward oneself.
- •
Personal growth: the insight into one’s own potential for self-actualization.
- •
Purpose in life: goals and beliefs directing one’s meaning in life.
- •
Positive relationships with others: having satisfactory personal relationships.
- •
Autonomy: self-determination as guided by one’s internal standards.
- •
Environmental mastery: ability to manage or create a suitable environment to accommodate personal needs and values.
Wellbeing should include a social dimension since our personal (psychological) wellbeing depends on the social context and our social connections.8 Coexistence in our work and life, traditions and beliefs are important for our social wellbeing (Fig. 2).9 Both psychological and social well-being are essential conditions for optimal functioning. Together they determine how we feel about ourselves and life in general, our emotional wellbeing. Emotional wellbeing means using strengths rather than focusing on solving problems or weaknesses.8–10
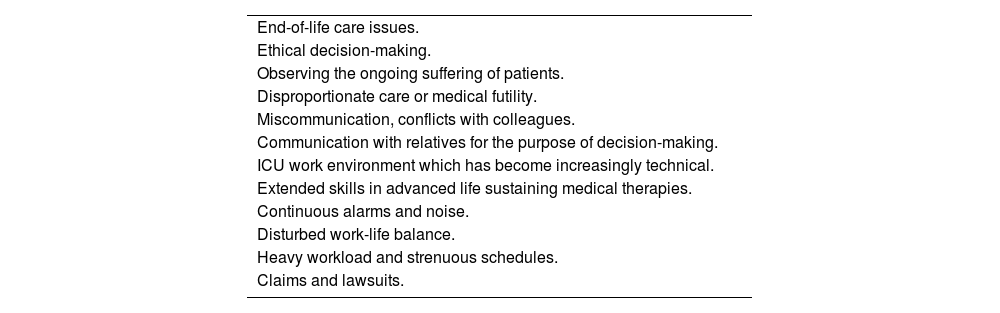
Stress-related factors in the ICUHealthcare professionals working in the ICU often deal with patients suffering from life threatening illness and their relatives struggling between hope and loss. Consequently, the role of healthcare professionals, during the patient’s illness can be challenging for themselves.11,12 In addition, working within a team of people with different personalities, competencies, and specialties, with constraints and demands, can contribute to a working environment that is prone to conflicts and disagreements.13 All this, emphasizes the ICU as a stressful work environment. It has been described that ICU healthcare professionals could be emotionally affected by several factors14–17 (Table 1). Thus, working in the ICU threaten the wellbeing of ICU nurses, intensivists, and allied healthcare professionals.
Causes of work-related stress in the ICU.
| End-of-life care issues. |
| Ethical decision-making. |
| Observing the ongoing suffering of patients. |
| Disproportionate care or medical futility. |
| Miscommunication, conflicts with colleagues. |
| Communication with relatives for the purpose of decision-making. |
| ICU work environment which has become increasingly technical. |
| Extended skills in advanced life sustaining medical therapies. |
| Continuous alarms and noise. |
| Disturbed work-life balance. |
| Heavy workload and strenuous schedules. |
| Claims and lawsuits. |
Individual responses to stress may be manifested as physical symptoms such as headaches, sleep disorders, low back pain and stomach problems or as mental responses such as being irritability or hostility, loss of concentration, low self-esteem, emotional instability.18 However, these are non-specific symptoms that do not enable the identification of the source of stress and therefore limit effective coping mechanisms or the development of preventive strategies for this ongoing process.19,20 In short, the stressful environment of the ICU has negative consequences on health professionals’ wellbeing.
Consequences of work-related stressConsequences of work-related stress for healthcare professionalsWork-related stress in ICU can lead to different situations that threaten the professionals' wellbeing:
- •
Burnout: it has been defined as a combination of three factors (emotional exhaustion, depersonalization, and reduced self-fulfillment).21 There is growing evidence that burnout among healthcare professionals working in an ICU is the result of a demanding and continuously high-stress work environment.20,22–24
- •
Compassion fatigue: it has been described as a loss of compassion due to repeated exposure to suffering during work.25 Compassion fatigue consists of two parts. The first part contains aspects such as exhaustion, frustration, and depression, typically associated with burnout. The second part is the negative feeling driven by concerns such as hypervigilance, avoidance, fear, and intrusion, which are also characteristic of traumatic stress symptoms.26–29
- •
Secondary traumatic stress: it has been defined as the destructive emotional distress resulting from an encounter with a patient who has suffered primary or direct trauma. It includes persistent and deliberate avoidance of distressing trauma-related stimuli.30
- •
Moral distress: it has been described as a challenge that arises when healthcare professionals know the right thing to do, medically or ethically, but institutional and/or external constraints make it nearly impossible to pursue the right course of action.31,32 This serious problem threats the integrity not only of healthcare professionals but of healthcare organizations as well. Moral distress has been associated with risk of burnout, employee attrition, propensity to leave a position and decreased quality of care.33–38
- •
Alarm fatigue: it occurs when healthcare professionals are over-stimulated by a high number of alarms, leading to a blunting of these warning signals, causing alarm desensitization, and leading to missed alarms or delayed response. As the frequency of alarms used in healthcare rises, alarm fatigue has been increasingly recognized as an important patient safety issue.39–42
All these concepts in the health impairment process underscore the same consequences of work-related stress. In a systematic literature review on emotional distress among ICU professionals, Hays et al.20 suggested that the true magnitude of work-related stress remains unclear and open to discussion due to a lack of unity in concepts, related measuring instruments, and cut-off points.
Work-related stress and poor wellbeing as well as high levels of burnout were found to be significantly associated with more self-reported errors.43 Healthcare professionals involved in adverse events may experience a range of emotions, including guilt, shame, anxiety, and depression. They may question their clinical skills and judgment, leading to a significant emotional toll. This has been described as the “second victim phenomenon”.44 Identifying and supporting second victims is important to maintain their mental health.45 This includes training aimed at raising awareness of these challenges, as well as measures to promote open communication and a culture of support.46
Consequences of work-related stress and patient safetyAll situations that negatively affect the wellbeing of health professionals jeopardize patient safety by compromising the ability of healthcare professionals to respond appropriately to medical alarms and provide compassionate, high-quality care.47 Studies in which both burnout and poor wellbeing were independently associated with poorer patient safety indicate how important both variables are. For example, burnout and depression can manifest themselves in the form of fatigue, irritability and reduced cognitive performance. All of this puts a strain on relationships within the team, leading to a poorer safety climate, as well as the individual’s own work performance, which in turn leads to greater distance between staff, poorer quality-of-care and ultimately a higher risk of errors. Work-related stress in healthcare professionals, especially among nurses, is a key factor in lowering patient safety culture and quality-of-care.48 To enhance patient safety, task distribution and support should account for variations in stress perceptions based on age, gender, marital status, and grade. It is important to take steps to recognize, prevent and manage these phenomena to ensure effective and safe patient care.49,50
Alarm fatigue can lead to a negligent or delayed response to actual medical emergencies. The constant presence of alarms, even if they are not critical, can lead to ICU staff underestimating the seriousness of alarms or even ignoring them.46 This increases the risk of misinterpretation or errors in handling vital situations, which ultimately jeopardizes patient safety.51
On the other hand, compassion fatigue also refers to the emotional, physical, and mental exhaustion that healthcare professionals may experience when continuously providing intense emotional support to patients. This can cause medical staff to be less attentive, make mistakes or even neglect the quality of patient care.
Impact of the COVID-19 pandemic on wellbeingApart from the large amount of literature on mental health and wellbeing within ICU settings published in recent years, the impact of the COVID-19 pandemic on healthcare professionals working in ICUs is also reflected in accentuated staff shortages and job leaving intentions.52,53 The prevalence of impaired psychological wellbeing, as well as symptoms of burnout and job dissatisfaction, was already high before the surge of COVID-1954,55 and was understandably exacerbated by the pandemic and its subsequent waves.55–57 In any case, COVID-19 warrants a separate chapter on wellbeing. The COVID-19 period has very specific factors of ICU working conditions from the scarcity of resources58,59 to the fear to get infected and to infect their loved ones, or the isolation between patients and relatives60 among others.
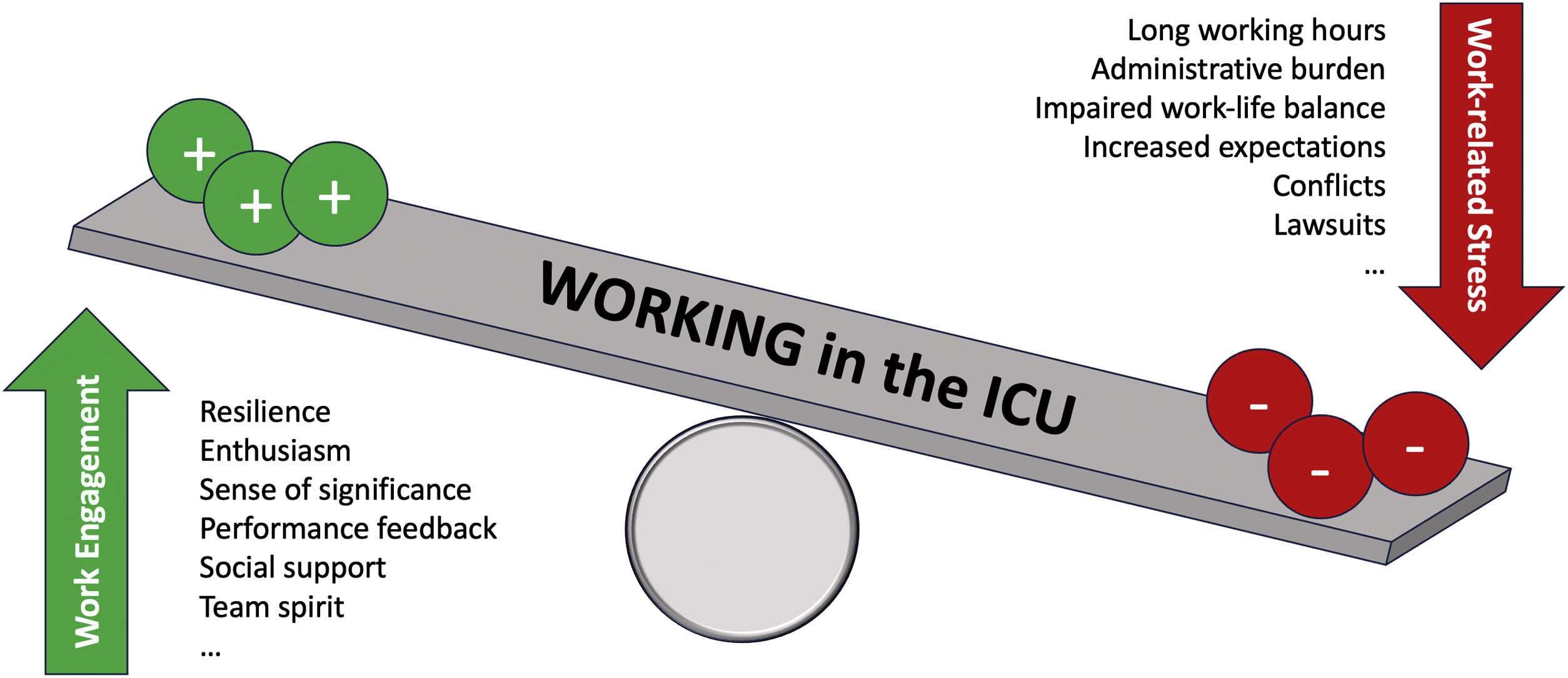
The role of resilience in wellbeingIn a work context, resilience is the ability of workers to adapt when faced with difficulties (work-related stress). It is a necessary quality to promote wellbeing when facing the challenges of life and work.61 Resilience is a learned skill, which encourages investment in resilience training. Resilience training helps to bounce, and not break.62 According to the Mayo Clinic, the most effective method to enlarge personal resilience is training attention and awareness. Becoming more intentional and purposeful will decrease negative thoughts and draw attention to what is most meaningful.63 Similar resilience training could be useful for ICU healthcare professionals to adaptively cope with work-related adverse conditions and stress, although research is still lacking to support this idea (Fig. 3).
Interventions to support wellbeing among ICU professionalsTo prevent migration of specialist staff from the ICU, it is of utmost importance to promote a proactive approach to wellbeing at work. This should be fostered by providing supportive organizational structures.64,65
In this respect, it is useful to differentiate between preventive approaches:
- -
Primary prevention aims to prevent health impairment and sick leave before they occur. This is achieved by avoiding exposure to (chronic) stressors and increasing resilience to work-related stress. Examples include enforcing safe and healthy practices (i.e., reasonable work schedules), enhancing interdisciplinary communication (regular moral counseling, team huddles and day starts),66 and educating about healthy and safe habits (i.e., regular exercise, relaxation techniques). A positive team culture and collegial support are needed to be open on the stressful situations and work environment of the ICU.67 In addition, the use of new tools to promote teamwork, communication, and patient safety such as real-time randomized safety audits could improve quality and safety in critically ill patients.68 Above that, addressing autonomy in work or supporting positive relationships among team members are important aspects.
- -
Secondary prevention seeks early detection of (dis)stress symptoms. Examples include training employees to better handle their work situation while providing them with resources to optimize their coping abilities and to enhance their resiliency to stress, using apps monitoring stress and vital signs 24/7, or self-report screening instruments.
- -
Tertiary prevention is defined as the treatment of individuals who are already highly stressed. It consists of providing ICU healthcare professionals with opportunities for treatment and recovery and the necessary services and resources to ensure their effectiveness.
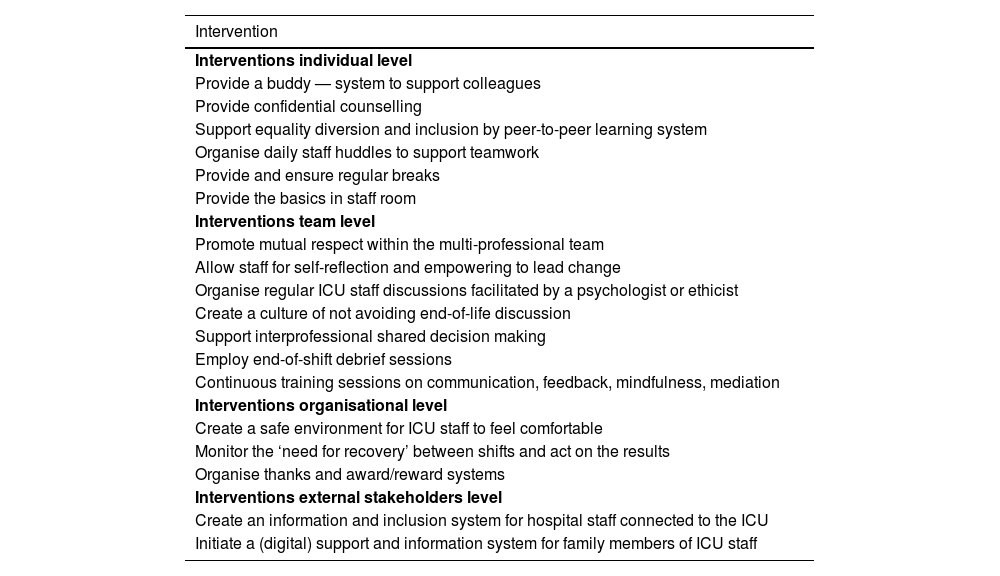
Recommendations on preventive strategies on how to relate to these aspects are often missing. Some studies measured the effect of interventions such as different working schedules of intensivists, educational programs on emotional distress, improvement of elements of family-centered care and communication skills.68–72 Other studies suggested preventive strategies, ranging from improving the working environment, changing the composition of teams to include more women, developing teamwork and regular job rotation.73–77 However, most interventions showed only a trend toward improvement and few programs resulted in statistically significant change. The implementation of a number of strategies, such as an active and intensive communication strategy regarding end-of-life care in the ICU, was associated with significantly lower rates of burnout and depression after some of these interventions.78 Further examples of interventions to support wellbeing of ICU health professionals are presented in Table 2.79
Interventions to support wellbeing among ICU professionals (Adapted from Latour et al. Crit Care. 2022;26(1):218.80).
| Intervention |
|---|
| Interventions individual level |
| Provide a buddy — system to support colleagues |
| Provide confidential counselling |
| Support equality diversion and inclusion by peer-to-peer learning system |
| Organise daily staff huddles to support teamwork |
| Provide and ensure regular breaks |
| Provide the basics in staff room |
| Interventions team level |
| Promote mutual respect within the multi-professional team |
| Allow staff for self-reflection and empowering to lead change |
| Organise regular ICU staff discussions facilitated by a psychologist or ethicist |
| Create a culture of not avoiding end-of-life discussion |
| Support interprofessional shared decision making |
| Employ end-of-shift debrief sessions |
| Continuous training sessions on communication, feedback, mindfulness, mediation |
| Interventions organisational level |
| Create a safe environment for ICU staff to feel comfortable |
| Monitor the ‘need for recovery’ between shifts and act on the results |
| Organise thanks and award/reward systems |
| Interventions external stakeholders level |
| Create an information and inclusion system for hospital staff connected to the ICU |
| Initiate a (digital) support and information system for family members of ICU staff |
To improve wellbeing of healthcare professionals working in ICU, it is not enough to help only those who are perceived to be under too much stress. Stress reactions are early indicators of an imbalance in the physical or emotional load and in the individual's ability to adapt to challenging situations. Positive and flourishing individual conditions are not only related to personal wellbeing but are also helpful for improving work performance and team spirit. This will ultimately improve quality-of-care and patient safety. However, changing the wellbeing of ICU healthcare professionals also requires addressing organizational wellbeing. Even if the consequences for healthcare professionals and patients can be well described and there is currently solid evidence, the solution for day-to-day work remains unclear. In any case, organizational strategies, such as structural changes, stress debriefings and ethical support in the ICU, can positively influence wellbeing at work as well as patient safety. This will ultimately improve quality-of-care and resilience of the team.
Authors’ contributionsERR and KF wrote and prepared the manuscript. MMCVM and JL supervised and approved the final version of the manuscript.
Conflict of interestThe authors have no conflict of interest to declare regarding this article.
FundingThis research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
None.