The current pandemic of SARS-CoV-2 has brought all healthcare systems to the point of collapse. This has brought more pressure to the intensive care units (ICU) mainly due to hypoxemic acute respiratory failure (ARF) requiring ventilatory support.1 The most commonly used ventilatory support technique is invasive mechanical ventilation (88%) vs non-invasive mechanical ventilation (NIV) (11%).1 Based on previous epidemics (SARS, influenza A-H1N1), the clinical practice guidelines have suggested the possibility of trying NIV in experienced centers as long as the necessary measures are taken to prevent transmitting the infection to the healthcare personnel involved.2 The current recommendations, based on the benefits provided by high-flow nasal oxygen therapy (HFNOT),3 and the high rate of failed NIV reported during the recent epidemic of Middle East respiratory syndrome coronavirus (MERS-CoV),4 have come up with a recommendation to use HFNOT to the detriment of NIV. Also, if NIV is eventually used, close monitoring should be performed to detect failed NIV.5
Following these recommendations and based on the experience gained with the use of NIV during the outbreaks of influenza,6,7 we used NIV as first-line therapy in our patients with hypoxemic ARF. BiPAP V60 ventilators (RespironicsInc.®, Pennsylvania, United States) into CPAP mode were used (15 cmH20 to 20 cmH20 of positive end-expiratory pressure or PEEP) with moisture-free tubing (antibacterial and antiviral respiratory filter), as well as the PerforMax® facial mask (RespironicsInc.®, Murrysville, PA, United States). Procedure: after the patient’s admission to the ICU and after confirming the need for NIV, hemodynamic and respiratory monitorization were performed. Afterwards, the NIV mode was changed into non-stop CPAP mode (15 cmH20 to 20 cmH20) except for hydration or hygiene purposes. In the presence of clinical improvement and better arterial blood gas test results, the FiO2/CPAP ratio was reduced with gradual disconnections with HFNC (with an oxygen level/air flow capable of keeping the same level of oxygenation compared to the previous one).
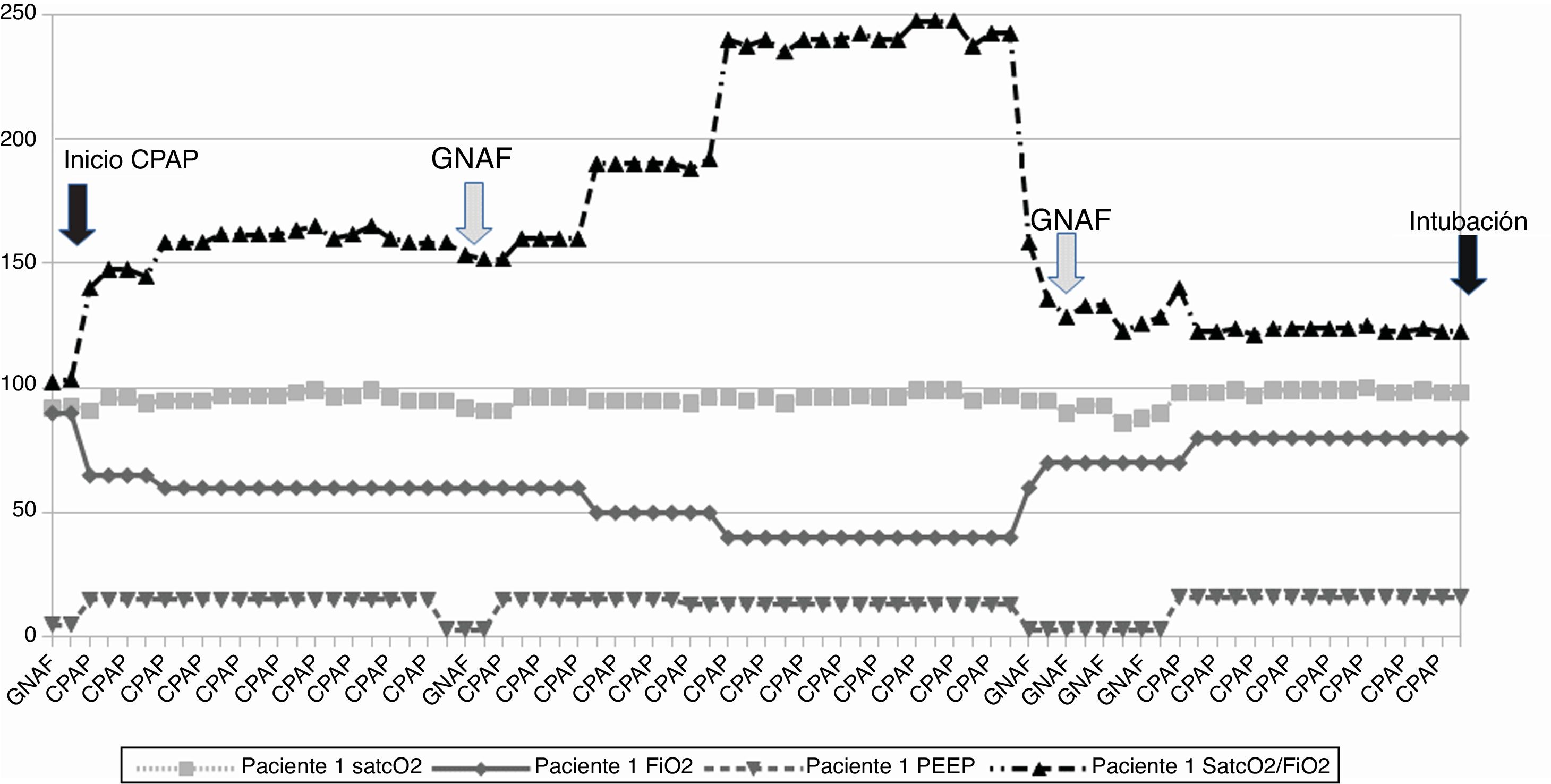
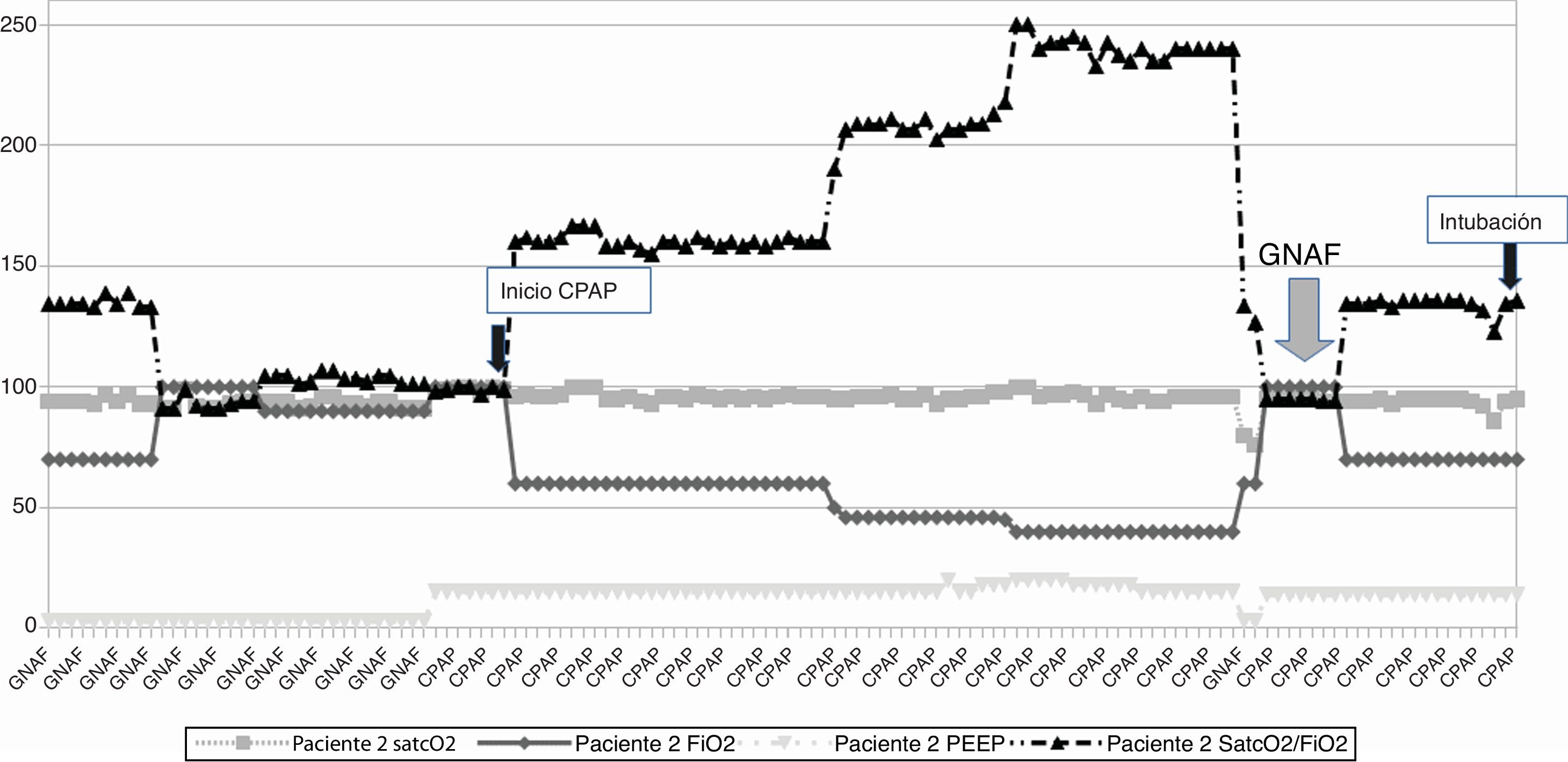
This is the case of 2 patients (Figs. 1 and 2) with pneumonia admitted to the ICU and treated with oxygen therapy through HFNC (air flow, 60 L/min; fraction of inspired oxygen [FiO2, 0.7 and 1.0, respectively]). After putting NIV into CPAP mode the patients’ clinical signs and arterial blood gas test values improved significantly (estimated by the percutaneous arterial oxygen saturation/fraction of inspired oxygen ratio [SpO2/FiO2 ratio]). The FiO2 dropped constantly with the passing of time until it reached FiO2 levels of 0.4−0.5. Given this situation, the disconnection of the HFNC was decided using software from the ventilator through Optiflow® nasal cannulae (Fischer & Payckel Healthcare Ltd., Auckland, New Zealand), and the MR850 active humidification system (Fischer & Payckel, Auckland, New Zealand). Once initiated (same FiO2 and air flow of 50 L/min to 60 L/min), the SpO2/FiO2 ratio dropped in both cases (gray arrow) probably due to lung de-recruitment. Both patients got worse and had to be reconnected to NIV requiring higher FiO2 levels. Fifteen hours after reinstating NIV the patients had to be intubated and connected to mechanical ventilation due to worse levels reported in the arterial blood gas test (black arrow).
Patient #1: Evolution of oxygen saturation (%), level of PEEP (cmH20), and oxygen concentration (FiO2) along non-invasive ventilation. CPAP, continuous positive airway pressure; FiO2, fraction of inspired oxygen; HFNC, high-flow nasal cannula; PEEP, positive end-expiratory pressure; SpO2, percutaneous arterial oxygen saturation.
Patient #2: Evolution of oxygen saturation de (%), level of PEEP (cmH20), and oxygen concentration (FiO2) along non-invasive ventilation. CPAP, continuous positive airway pressure; FiO2, fraction of inspired oxygen; HFNC, high-flow nasal cannula; PEEP, positive end-expiratory pressure; SpO2, percutaneous arterial oxygen saturation.
Initially, patients received HFNC that later proved insufficient from the oxygenation point of view. The study on which the use of HFNC to treat this condition is based is a multicenter clinical trial that compared 3 ways of oxygen therapy: conventional oxygen therapy, HFNC, and NIV. In the subgroup of patients with a partial pressure arterial oxygen/fraction of inspired oxygen ratio (PaO2/FiO2) ≤ 200 mmHg, both the rate of intubation (53%, 35%, and 58%, P = .009), and the mortality rate (16%, 10%, and 23%, P = .03) were significantly lower in the HFNC group.3 The fact of the early improvement with CPAC vs HFNC may be due to our patients’ increased hypoxemia (although we used the SpO2/FiO2 ratio); on the other hand, it may be due to the higher level of PEEP used since the estimated level provided by HFNC goes from 3 cmH20 to 5 cmH20. The preeminence of HFNC over NIV in the latest recommendations published,5 based on the results of the FLORALI3 trial, have been recently put into question.8 The authors use methodological aspects to question this indication by suggesting that both non-invasive support systems may be adequate to treat these patients’ hypoxemia.8 This conclusion was backed by a meta-analysis that proved that all non-invasive oxygen therapy strategies (NIV, HFNC) reduce mortality compared to conventional oxygen therapy.9
The British guidelines support the use of CPAP modes with elevated levels of PEEP (12 cmH20 to 15 cmH20) in patients with hypoxemic ARF. However, the use of HFNC10 is ill-advised. Based on our own experience, we totally agree with these guidelines since it was evident that the CPAP mode improved oxygenation significantly. However, the withdrawal of CPAP and further administration of HFNC made respiration worse, and eventually triggered intubation. The role of HFNC in the management of SARS-CoV-2-induced pneumonia may be effective during the early stages of ARF as a back-up therapy while NIV is off or as the back-up when weaning from NIV until progression to conventional oxygen therapy. In light of all this, its use while NIV is off will not possible as long as clinical stability has not been achieved, which translates into acceptable PEEP levels (<10 cmH20). Otherwise, it can lead to lung de-recruitment and, eventually to the patient’s intubation. Therefore, we recommend using HFNC wisely giving it the value it really has at each moment. At the same time, we recommend the correct use of NIV optimizing all aspects that can lead to failed NIV. This is what would be required: first talk to the patient on the technique that should be used to reduce the levels of uncertainty and anxiety; secondly, use comfortable interfaces without too many leaks (helmets or face masks); thirdly, use high pressure levels (CPAP above all) to keep the lung as recruited as possible; fourth, use clinical-arterial blood gas test parameters, not just the PaO2/FiO2 ratio, as a guidance to assess the response to NIV.
Please cite this article as: Belenguer-Muncharaz A, Hernández-Garcés H. Fracaso de la ventilación no invasiva tras empleo de oxigenoterapia de alto flujo en pacientes con neumonía por SARS-CoV-2. Med Intensiva. 2021;45:e37–e39.