Prone positioning (PP) in patients with severe oxygenation impairment is one of the adjuvant strategies that has demonstrated to improve survival in acute respiratory distress syndrome (ARDS).1
During the coronavirus-19 (COVID-19) pandemic, a huge proportion of patients developed ARDS under mechanical ventilation (MV). In this context, epidemiological studies informed higher rates of PP use; nonetheless, the number of PP sessions reported has been similar to previous studies.2,3
The inability to sustain the oxygenation improvement when back to supine position, the heavy workload imposed by proning and the potential adverse effects associated with PP might lead to discussions about the usefulness of successive PP sessions in advanced phases of late ARDS.
In this retrospective, case-series study, we describe the results of patients older than 18 years old under MV that developed moderate-severe ARDS induced by COVID-19 and required 8 or more PP sessions. The number of sessions considered for inclusion was based on the number of cycles above the first standard deviation of the PROSEVA trial (4±4) and the amount of sessions commonly used in previous studies.1–3 The implementation and detention protocol of PP was based on PROSEVA trial recommendations.1
Data are expressed as mean (SD), median (IQR) and number (percentage), as appropriated. The Shapiro–Wilk test was used to test normality. The analysis of data was performed using Prism version 8.4 for Mac OS (GraphPad Software, San Diego, CA, USA) and Statical Software R. All reported P values are two-sided, and have not been adjusted for multiple comparisons. A p value of less than 0.05 was considered to indicate statistical significance. The study was approved by the local review board (approbation code: 10-2021). All the patients signed the informed consent.
Between 1 March 2020 and 31 July 2021, one-hundred fifty one patients were admitted with diagnosis of COVID 19 and required MV. One-hundred and six (70%) required PP and twenty three (17.6%) of them needed ≥8 PP sessions. Demographic characteristics and outcomes of the overall sample and those who died and survived are shown in Table 1. Demographic characteristics did not significantly differ between survivors and non-survivors.
Patient's characteristics and outcomes.
| All patients (n=23) | Survivors (n=13) | Non-survivors (n=10) | P value | |
|---|---|---|---|---|
| Demographic and laboratory | ||||
| Male gender, n (%) | 12 (52.2) | 8 (61.5) | 4 (40) | 0.546 |
| Age, mean (SD) | 58.2 (13.5) | 55.4 (13.9) | 61.8 (17.9) | 0.266 |
| SAPS II, median [IQR] | 31.5 [26.5–36.5] | 31 [27–38] | 33 [25–35.5] | 0.968 |
| APACHE II, mean (SD) | 12.6 (5.2) | 12.8 (4.9) | 12.1 (35.8) | 0.805 |
| Days of symptoms onset to intubation, median IQR | 8 [6–11.5] | 9 [8–13] | 7.5 [6–8.7] | 0.152 |
| Prone positioning | ||||
| PaO2/FiO2 before 1st PP session, mean (SD) | 120.1 (25.1) | 119.1 (27.3) | 121.6 (23.3) | 0.830 |
| Crs before 1st PP, mean (SD) | 29.4 (12) | 29.3 (13.3) | 30.5 (10.4) | 0.831 |
| Ventilatory Ratio before 1st PP, mean (SD) | 2.2 (0.6) | 2.2 (0.6) | 2.2 (0.6) | 0.928 |
| PP sessions, median [IQR] | 11 (9-14) | 10 (9-14) | 11 (9-14) | 0.570 |
| Days from last PP to end of MV, mean (SD) | 7 [2–15] | 13 [10–15] | 1.5 [0–2] | <0.001 |
| Outcomes | ||||
| MV days, median [IQR] | 30 [23–34] | 31 [30–41] | 22 [18.5–27.7] | 0.003 |
| Extubation, n (%) | 3 (13) | 1 (7.7) | 2 (20) | 0.807 |
| Reintubation, n (%) | 2 (66) | 1 (100) | 1 (50) | 1.000 |
| Tracheostomy, n (%) | 14 (60) | 12 (92.3) | 2 (20) | 0.002 |
References. SAPS II: Simplified Acute Physiology Score II, APACHE II: Acute Physiology and Chronic Health Evaluation II, PaO2/FiO2: ratio of the partial pressure of oxygen in arterial blood (PaO2) to the inspired oxygen fraction (FiO2), MV: mechanical ventilation, Crs: Respiratory system compliance, PP: prone position; SD: standard deviation; IQR: interquartile range. Values are expressed in mean (SD), median [IQR] and number (percentage), as appropriate.
All patients met moderate to severe ARDS criteria at the time of the first PP session. A total of 273 PP sessions were performed, with a median (IQR) of 11 (9–14) sessions per patient, reaching a maximum of 21 in 1 patient. The median (IQR) duration of invasive ventilation was 30 (23–34) days. Survivors had significantly more days of MV than non-survivors [median: 31 (IQR 30–41) vs 22 (IQR18.5-27) p<0.003]. Only 26% of the patients were weaned from MV and 60% (n=14) of them underwent tracheostomy. These outcomes are representative of a subgroup of patients with infrequent characteristics in relation to the number of prone sessions reported by Estenssoro et al. and COVID-ICU Group.2,3 ICU mortality was 43.5%, lower than reported in mechanically ventilated patients with COVID-19 in Argentina (57%).3
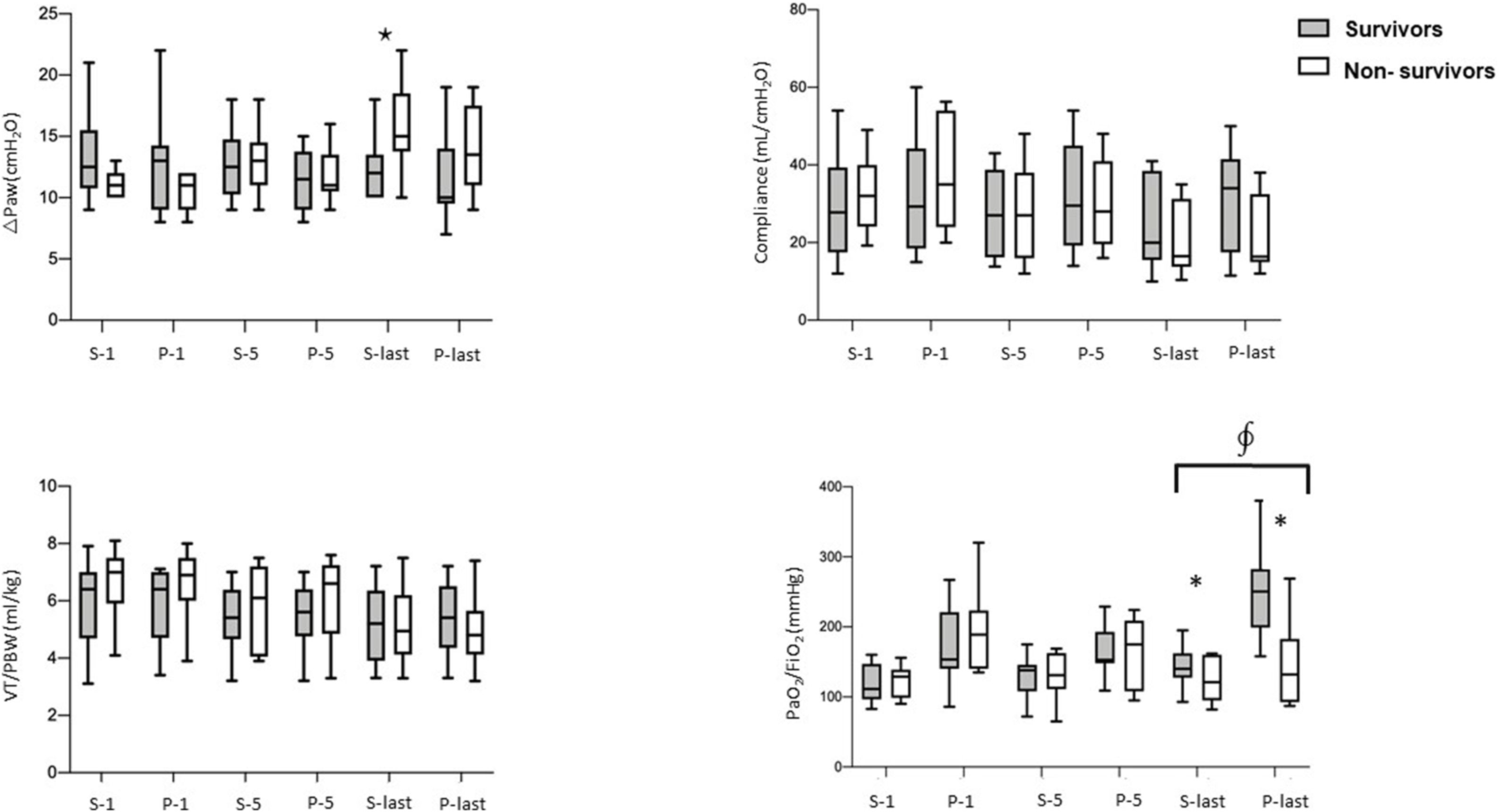
Fig. 1 shows the behavior of tidal volume adjusted by predicted body weight (VT/PBW), respiratory system mechanics and oxygenation before and after the first, fifth and last PP cycle. The decision to show the fifth PP session was based on the half our PP sessions in the overall sample. All the patients presented a trend to improve the respiratory system compliance, airway driving pressure and oxygenation in the first and fifth session. This behavior was homogeneous, preventing the identification of patterns of response between survivors and non-survivors. Shelhamer et al. and Weiss et al. reports similar oxygenation outcomes in the first PP cycle.4,5
PaO2/FiO ratio, respiratory system compliance, DPaw and VT/PBW before and after the first, fifth and last prone position cycle. PaO2/FiO2: ratio of the partial pressure of oxygen in arterial blood (PaO2) to the inspiren oxygen fraction (FiO2); Crs: Respiratory system compliance; DPaw: airway driving pressure; VT/PBW: tidal volume to predicted body weight; S-1: Supine before first session; P-1: after first prone session; S-5: Supine before fifth prone session; P-5: After fifth prone session; S-last: Supine before last prone session; P-last: after last prone session. Circles and squares correspond to the mean and mustaches to the standard deviations. ☆p=0.01: comparison of DPaw between survivors and non-survivors in S-last. ∮p=0.0001: comparison of the magnitude of change in PaO2/FiO2: between survivors and non-survivors in supine vs prone position. *p=0.001: comparison of PaO2/FiO2: between survivors and non-survivors in S-last and P-last.
Although we did not find differences in VT/PBW between groups, patients who did not survive presented higher DPaw and worst oxygenation before the last prone cycle (p<0.05).
The ratio of the partial pressure of oxygen in arterial blood to the inspired oxygen fraction (PaO2/FiO2) value after the last prone session was significantly higher in survivors compared to non-survivors (p=0.001). Also, the magnitude of change in PaO2/FiO2 after the last cycle was significantly different between groups (p=0.0001).
In the last proning session, oxygenation only increased in patients that survived. Such finding should not be considered as a distinctive feature between groups or a predictor of results but probably reflects a clinical improvement in survivors that took us to stop proning them while an unfavorable evolution of non-survivors. We believe that the lack of improvement in gas exchange should not be considered as a stop-proning criteria.6 Regarding oxygenation criteria, the PROSEVA trial proposed to stop prone treatment only when PaO2/FiO2 decreased>20% in two consecutive sessions, a situation that was not achieved by none of non-survivors. This is supported by the brief period of time from the last prone session to the end of mechanical ventilation in non-survivors (1.5 [IQR 0–2]), reinforcing that prone treatment was maintained until the last days (Table 1). In contrast to our results, Gleissman et al. found a significant increase in oxygenation only during the first three PP cycles, explaining that the lack of improvement could be due to progression of ARDS to a more proliferative phase after several days of MV. According to this observation and the high rates of complications reported during PP maneuvers, the authors suggest that assuming PP at this time point implies more risks than benefits.7 In our cohort, only four potentially serious complications were registered during 273 maneuvers (hipotension, oxygen desaturation and ventilator circuit disconnection) and none of the cycles had to be interrupted due to severe complications. Pressure sores (PS) were registered in 13/23 patients (56%), which were localized in the facial (10/23) and thoracic region (3/23) with a median of 2.3 (IQR 2–3) per patient. The median (IQR) grade of PS was 2 (1–2).8
Our findings support the proposed detention criteria of PROSEVA trial.1 The favorable response even after multiple PP sessions, the low rate of severe adverse effects, the favorable results in terms of mortality and the lack of predictors associated with degree of response to the intervention suggest that interrupting the implementation of PP should not be considered even beyond the number of cycles commonly reported in the literature.
Funding sourcesThis research did not receive any specific grant.
Conflict of interestNone.
Lic. Daniela Gilgado (Physical and Respiratory Therapy Service Sanatorio Anchorena San Martin)
Dr. Diego Halac (Chief of Medical Clinic Sanatorio Anchorena San Martín).