To describe the practice of Pediatric Intensive Care in Latin America and compare it with two European countries.
DesignAnalysis of data presented by member countries of the Sociedad Latinoamericana de Cuidado Intensivo Pediátrico (SLACIP), Spain and Portugal, in the context of a Symposium of Spanish and Portuguese–speaking pediatric intensivists during the Fifth World Congress on Pediatric Intensive Care.
SettingPediatric Intensive Care Units (PICUs).
ParticipantsPediatric intensivists in representation of each member country of the SLACIP, Spain and Portugal.
InterventionsNone.
Variables of interestEach country presented its data on child health, medical facilities for children, Pediatric Intensive Care Units, pediatric intensivists, certification procedures, equipment, morbidity, mortality, and issues requiring intervention in each participating country.
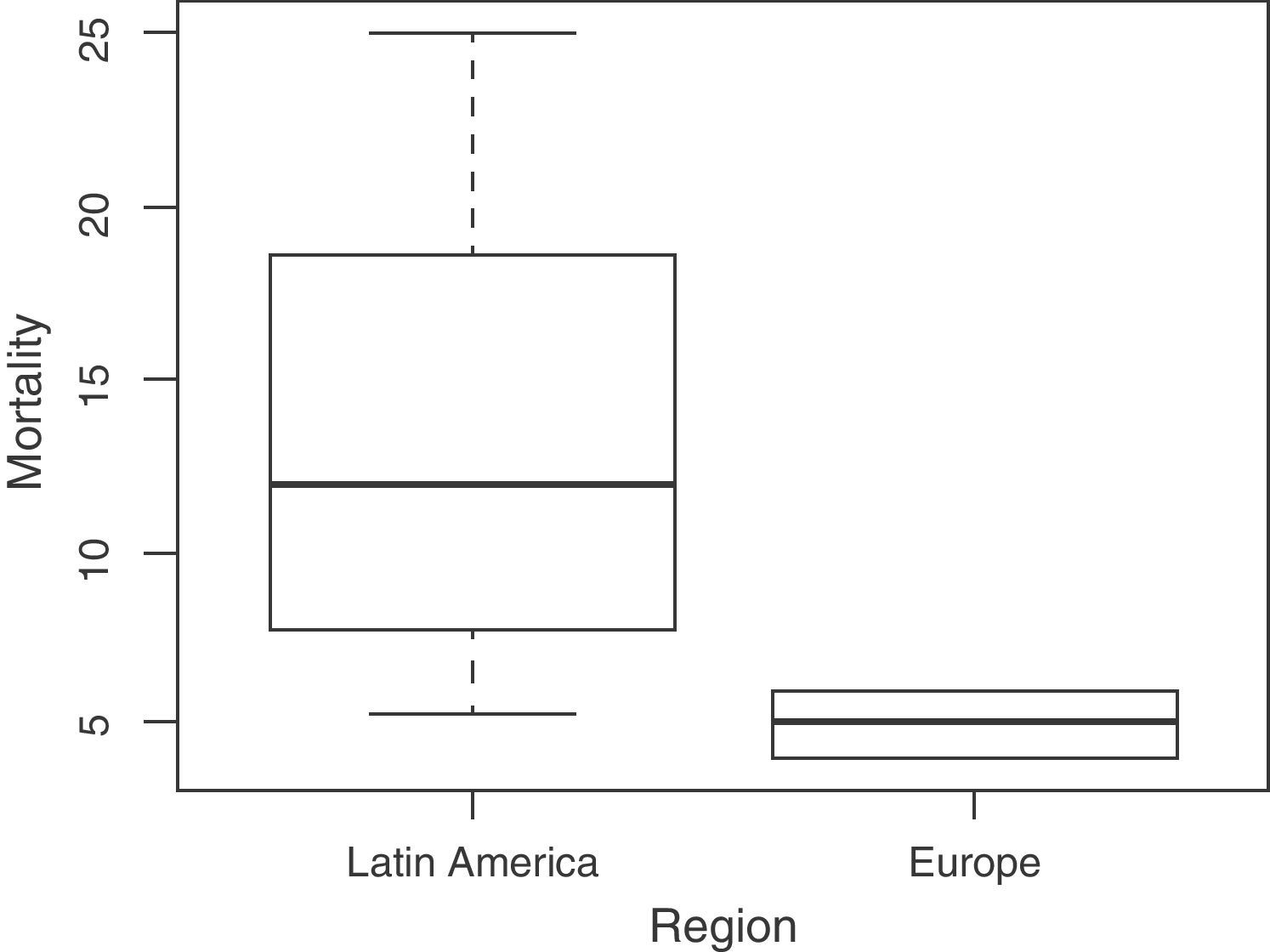
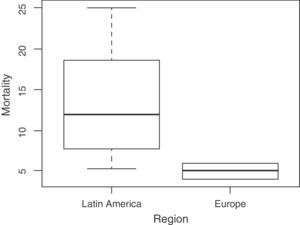
ResultsData from 11 countries were analyzed. Nine countries were from Latin America (Argentina, Colombia, Cuba, Chile, Ecuador, Honduras, Mexico, Dominican Republic and Uruguay), and two from Europe (Spain and Portugal). Data from Bolivia and Guatemala were partially considered. Populational, institutional, and operative differences were identified. Mean PICU mortality was 13.29% in Latin America and 5% in the European countries (p=0.005). There was an inverse relationship between mortality and availability of Pediatric Intensive Care Units, pediatric intensivists, number of beds, and number of pediatric specialty centers. Financial and logistic limitations, as well as deficiencies in support disciplines, severity of diseases, malnutrition, late admissions, and inadequate initial treatments could be important contributors to mortality at least in some of these countries.
ConclusionThere are important differences in population, morbidity, and mortality in critically ill children among the participating countries. Mortality shows an inverse correlation to the availability of Pediatric Intensive Care Units, intensive care beds, pediatric intensivists, and pediatric subspecialty centers.
Conocer cómo es la práctica de los cuidados intensivos pediátricos en Latinoamérica en comparación con 2 países europeos.
DiseñoRecopilación y análisis de los datos presentados por los países miembros de la Sociedad Latinoamericana de Cuidado Intensivo Pediátrico (SLACIP), España y Portugal, en el Simposio de Intensivistas Pediátricos de Habla Española y Portuguesa realizado durante el V Congreso Mundial de Cuidado Intensivo Pediátrico.
ÁmbitoUnidades de cuidado intensivo pediátrico.
ParticipantesIntensivistas pediátricos representantes de los países que conforman la SLACIP, España y Portugal.
IntervencionesNinguna.
Variables de interés generalSe recolectaron, de cada país, indicadores de salud infantil, características de las instituciones de salud dedicadas al cuidado de los niños, unidades de cuidados intensivos pediátricos (UCIP), intensivistas pediátricos, procesos de certificación dentro de la especialidad, equipamiento de las diferentes unidades, casuística, cifras de mortalidad y principales problemas que requieren solución en cada uno de los países participantes.
ResultadosSe analizaron los datos de 11 países, 9 latinoamericanos (Argentina, Colombia, Cuba, Chile, Ecuador, Honduras, México, República Dominicana y Uruguay) y 2 europeos (España y Portugal). Los datos de Bolivia y Guatemala fueron considerados solo parcialmente. Se identificaron diferencias poblacionales, institucionales y operativas entre los diferentes países. La mortalidad promedio fue 13,29% en las UCIP latinoamericanas y 5% en las UCIP europeas (p=0,005). La mortalidad se correlacionó de forma inversa con la disponibilidad de UCIP, número de intensivistas pediátricos, número de camas y número de centros pediátricos de especialidad. Limitaciones logísticas y financieras, deficiencias en las disciplinas de apoyo, estado general precario de los pacientes por desnutrición, retraso en su ingreso y tratamientos iniciales inadecuados, pueden ser contribuyentes significativos a la mortalidad al menos en algunos de estos países.
ConclusiónExisten diferencias significativas en términos poblacionales y de morbimortalidad entre los países estudiados. La mortalidad se correlaciona de forma inversa con la disponibilidad de UCIP, número de intensivistas pediátricos, número de camas y número de centros pediátricos de especialidad.
In the year 2000, the World Health Organization (WHO) established its “Goals for the Millennium”, with the purpose of improving human living conditions by the year 2015.1 The fourth goal is of particular interest for pediatricians: “To reduce mortality by two-thirds among children under 5 years of age by the year 2015”. Reaching this goal would mean avoiding over 6 million deaths every year.2
The strategy designed for reaching these “Goals for the Millennium” is mainly based on the adoption of preventive health measures, but it is unlikely for them to be reached in many countries, due to a series of problems.3,4 New alternative actions are moreover needed,5 such as those that depend on emergency services and Pediatric Intensive Care (PIC), which should be available to all children who need them.6 In this sense, it has been shown that the planned and careful implementation of such actions can easily reduce mortality by at least 50%.7
PIC is a relatively new discipline in Pediatrics. The first Pediatric Intensive Care Unit (PICU) was created in Gothenburg (Sweden) in 1955, and the first such Unit in the United States was established in the Children's Hospital of the District of Columbia in 1965.8 In Latin America, PICUs were created in the period between 1972 and 1990.9 Although these units have shown important advances, similar in many cases to those found in more developed countries, little is known of the general characteristics of their organization or development. The publications found on this subject in the international literature are few, and there are no reliable registries of the available PICU beds, their accessibility, or the quality of the care provided.10–13
The Latin American Society of Pediatric Intensive Care (Sociedad Latinoamericana de Cuidado Intensivo Pediátrico, SLACIP) was created in 1993 following a first meeting of Latin American pediatric intensivists on occasion of the First World Congress of the specialty held in Baltimore.14 Starting in 1996, the SLACIP has organized the Symposium of Spanish- and Portuguese-Speaking Pediatric Intensivists as an event prior to the world congresses in the field, creating a scenario aiming to favor professional development and the exchange of experiences among Latin American countries, Spain and Portugal. However, a genuine regional perspective of PIC in the member countries of the SLACIP is lacking. A comparison with European references such as Spain and Portugal could help identify strengths, weaknesses, and areas requiring further development through the adoption of policies and strategies specifically designed to the effect.6
With this idea in mind, in 2006 the SLACIP requested each country to supply its general health information and specific data on PIC practice. A preliminary analysis was made in 2007 on occasion of the World Congress of PIC held in Geneva (Switzerland),15 and this analysis is now expanded and described in the present article.
Patients and methodsSix months before the V World Congress of PIC, the Presidents of the national societies in the discipline in each Latin American country, as well as in Spain and Portugal, received an invitation to participate with a poster in the Symposium of Spanish- and Portuguese-Speaking Pediatric Intensivists. Where the official representative of each country was not known, contact was made with renowned experts in the field, as established from the registries of the SLACIP. The poster was required to offer the following information: country; name of the Society, Association, Branch or Chapter; total population of the country and population under 18 years of age; the five leading causes of infant and neonatal morbidity–mortality; infant and neonate mortality rates; general hospitals with Pediatric Departments; pediatric hospitals; pediatric hospital beds; pediatric traumatology or heart surgery centers; PICUs and their geographic distribution; PICU beds; PIC beds within adult Intensive Care Units (ICUs); and PICU beds per 30,000 children. Regarding PICU care activities, information was requested on the most frequent disorders and on the prevalence of denutrition among the children admitted due to critical disease. In relation to the technology available in the Units, data were compiled on the availability of conventional mechanical ventilation (MV), noninvasive MV, high-frequency MV, nitric oxide, heliox, invasive monitorization, the use of extracorporeal techniques (hemodialysis, peritoneal dialysis, plasmapheresis), and the use of enteral or parenteral nutrition. Information was also requested on the number of pediatric intensivists in the country, their formal professional certification process, the presence or absence of national clinical guides, and the existence or absence of inter-institutional collaborative projects. As general indicators, information was collected on mortality in the PICU and on the incidence of nosocomial infections. Lastly, data were requested on the main problems affecting the operation of the PICUs. One of the authors (SCM) compiled the data and analyzed them using the R version 2.12.2 statistical software (R Foundation for Statistical Computing, Vienna, Austria). Posteriorly, a data check and update was made referring to the vital and public health statistics according to the official information of the WHO.16,17
ResultsA total of 11 countries participated in the project: 9 Latin American nations (Argentina, Colombia, Cuba, Chile, Ecuador, Honduras, Mexico, the Dominican Republic and Uruguay) and two European countries (Spain and Portugal). Bolivia and Guatemala submitted incomplete data that were considered only in part.
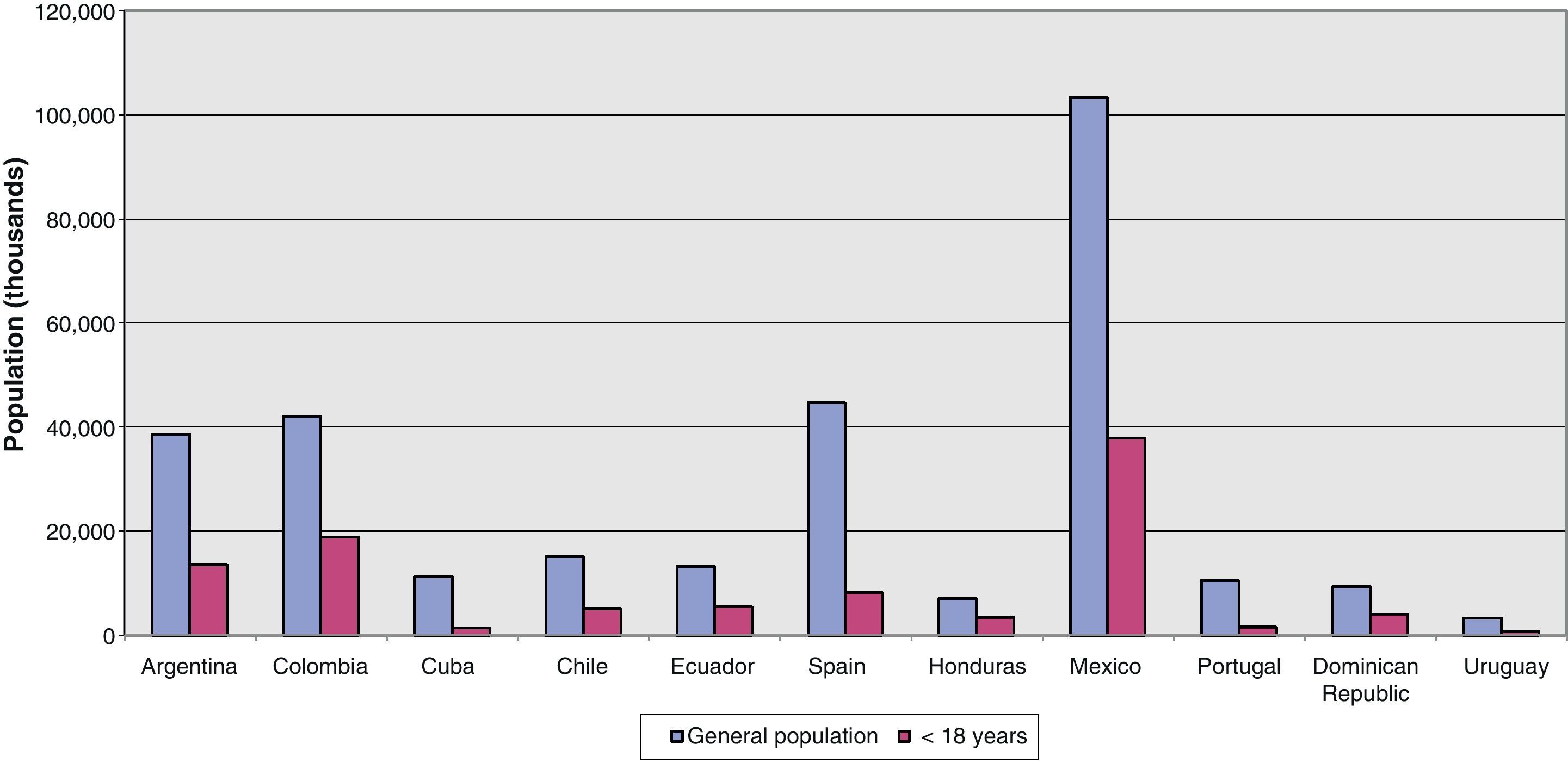
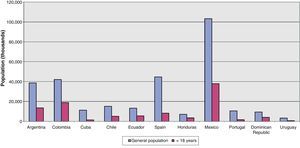
Population dataThe population of the participating countries totaled 298,503,361 inhabitants, ranging from 3,300,000 inhabitants in Uruguay to a little over 100,000,000 in Mexico. The population under 18 years of age totaled 100,574,490 inhabitants, though the figure contributed by Portugal corresponded to subjects under 14 years of age. On average, 33.7% of the population was underage. Fig. 1 shows the percentage distribution of the underage population versus the general population. The European countries and Cuba presented a low proportion of underage individuals, related to a drop in birth rate. The rest of the Latin American countries showed a significant proportion of children and young individuals in their populations, ranging from 27% in Uruguay to 50% in Honduras.
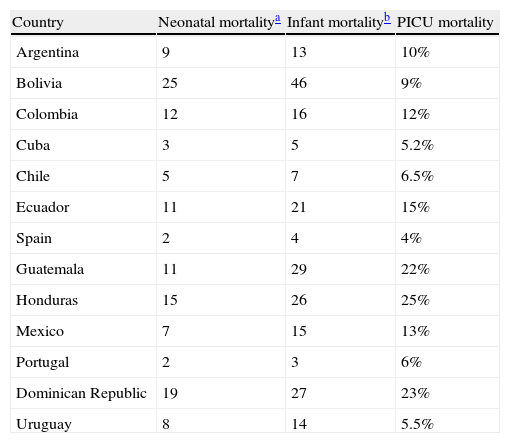
MortalityTable 1 shows the data supplied by the participating country, while Table 2 establishes a comparison between the Latin American and European countries. The most frequent causes of perinatal mortality were premature birth, congenital malformations, chromosomal alterations, congenital heart disease, asphyxia and intracranial bleeding. Honduras reported trauma as the first cause of perinatal mortality, while Uruguay cited hemorrhagic disorders and sudden death as significant problems associated to mortality.
Neonatal mortality, infant mortality and Pediatric Intensive Care Unit mortality in Latin American countries, Spain and Portugal.
| Country | Neonatal mortalitya | Infant mortalityb | PICU mortality |
| Argentina | 9 | 13 | 10% |
| Bolivia | 25 | 46 | 9% |
| Colombia | 12 | 16 | 12% |
| Cuba | 3 | 5 | 5.2% |
| Chile | 5 | 7 | 6.5% |
| Ecuador | 11 | 21 | 15% |
| Spain | 2 | 4 | 4% |
| Guatemala | 11 | 29 | 22% |
| Honduras | 15 | 26 | 25% |
| Mexico | 7 | 15 | 13% |
| Portugal | 2 | 3 | 6% |
| Dominican Republic | 19 | 27 | 23% |
| Uruguay | 8 | 14 | 5.5% |
Per 1000 live births, WHO 2008.
In children under 5 years of age, per 1000 live births, WHO 2008.
Comparison of mortality data by regions.
| Region | Latin America | Europe | p | 95%CI | ||
| x¯ | OF | x¯ | OF | |||
| Neonatal mortalitya | 11.36 | 6.36 | 2.0 | 0 | 0.0006 | 5.09–13.63 |
| Infant mortalityb | 19.90 | 11.67 | 3.5 | 0.7 | 0.0008 | 8.52–24.29 |
| PICU mortality | 13.29 | 7.16 | 5 | 1.41 | 0.005 | 2.99–13.58 |
Per 1000 live births, WHO 2008.
In children under 5 years of age, per 1000 live births, WHO 2008.
Mean infant mortality (affecting children under 5 years of age) was 17.4 per 1000 live births (Table 1). Spain reported 43.8 deaths per 100,000 inhabitants between one month and 18 years of age, though the WHO-based data cite 4 deaths per 1000 live births. Colombia and Mexico did not report this rate, though the WHO registered 16 and 15 deaths per 1000 live births in these countries. The described causes of infant mortality included perinatal disorders, congenital malformations, congenital heart diseases, pneumonia, acute diarrhea, sepsis, denutrition, accidents and traumatisms, diseases of the nervous system, and oncohematological diseases. In the countries with the highest infant mortality rates such as the Dominican Republic, Honduras and Ecuador, the predominant causes were infections (mainly of a respiratory and gastrointestinal nature) and denutrition. In the European countries there was a prevalence of non-infectious conditions such as traumatisms, tumors, nervous system disorders, congenital malformations and cardiorespiratory problems. The Dominican Republic was the only country citing infection with the human immunodeficiency virus (HIV) as a cause of infant mortality.
Hospital infrastructure for pediatric patientsAll countries had numerous general hospitals with Pediatric Departments, though the number of available beds was not reported. In comparison, the number of pediatric hospitals was limited, with the exception of Cuba, Argentina, Spain, and Mexico. Such hospitals are preferentially located in the major cities. Honduras has no pediatric hospital, Uruguay has only one, the Dominican Republic and Chile each have three, Portugal likewise has three, and Ecuador has four pediatric hospitals. Here again the number of available beds in each center was not specified. Pediatric centers specialized in trauma and heart surgery were found to be more numerous in Argentina and Mexico.
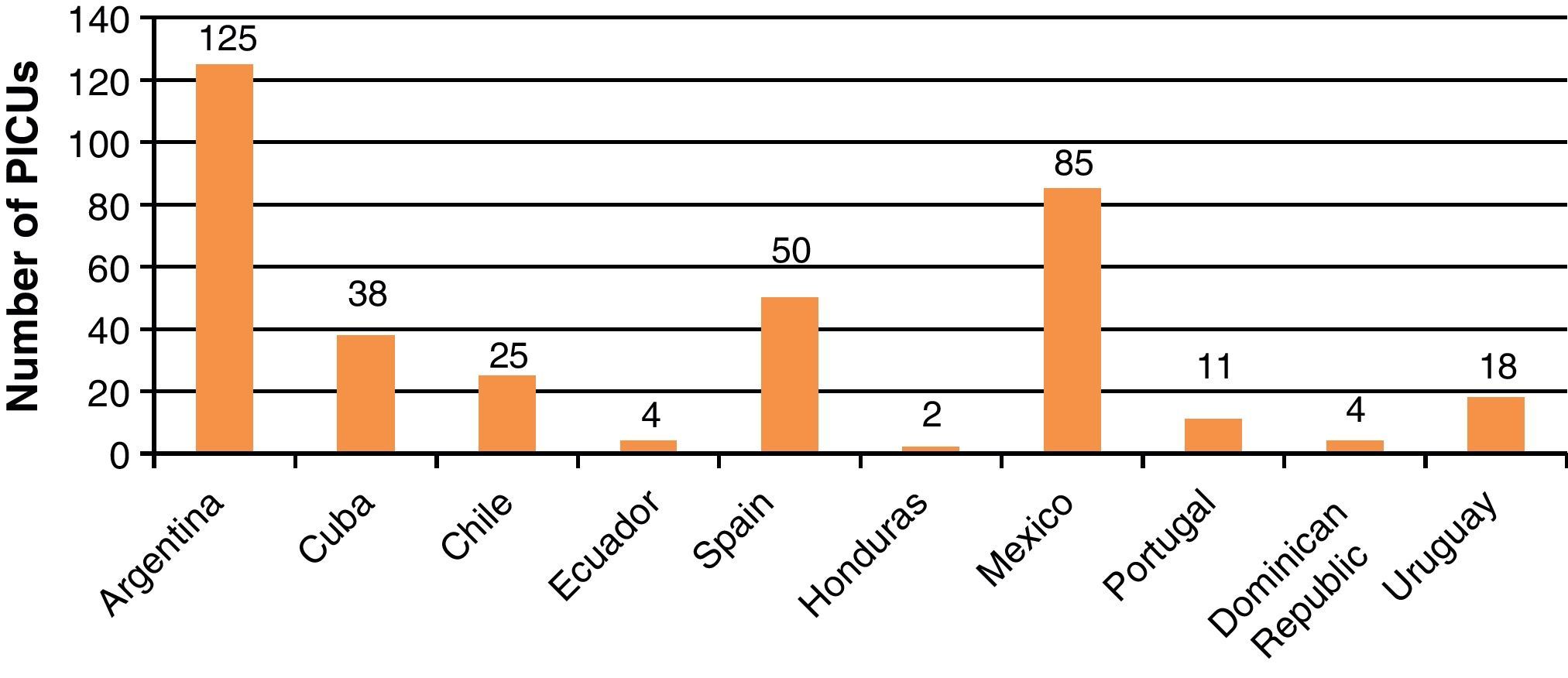
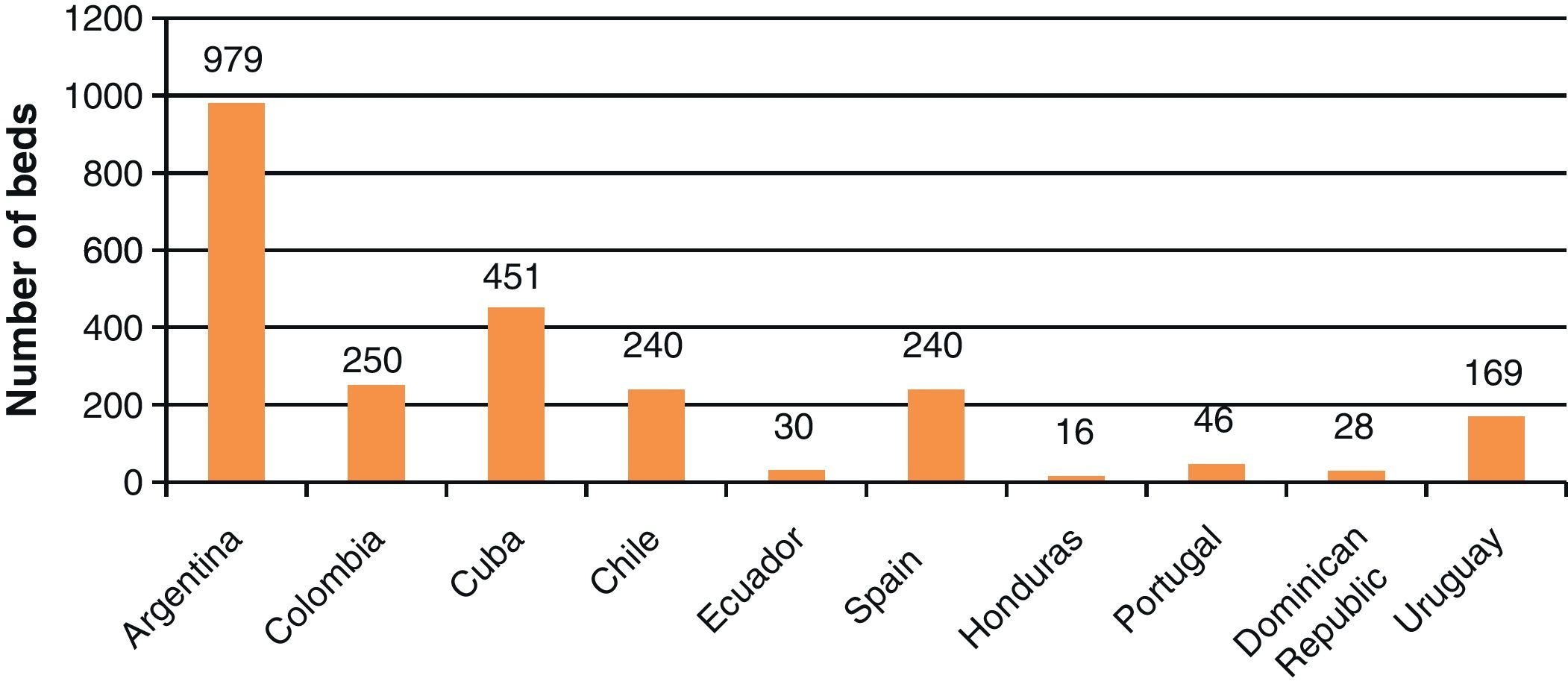
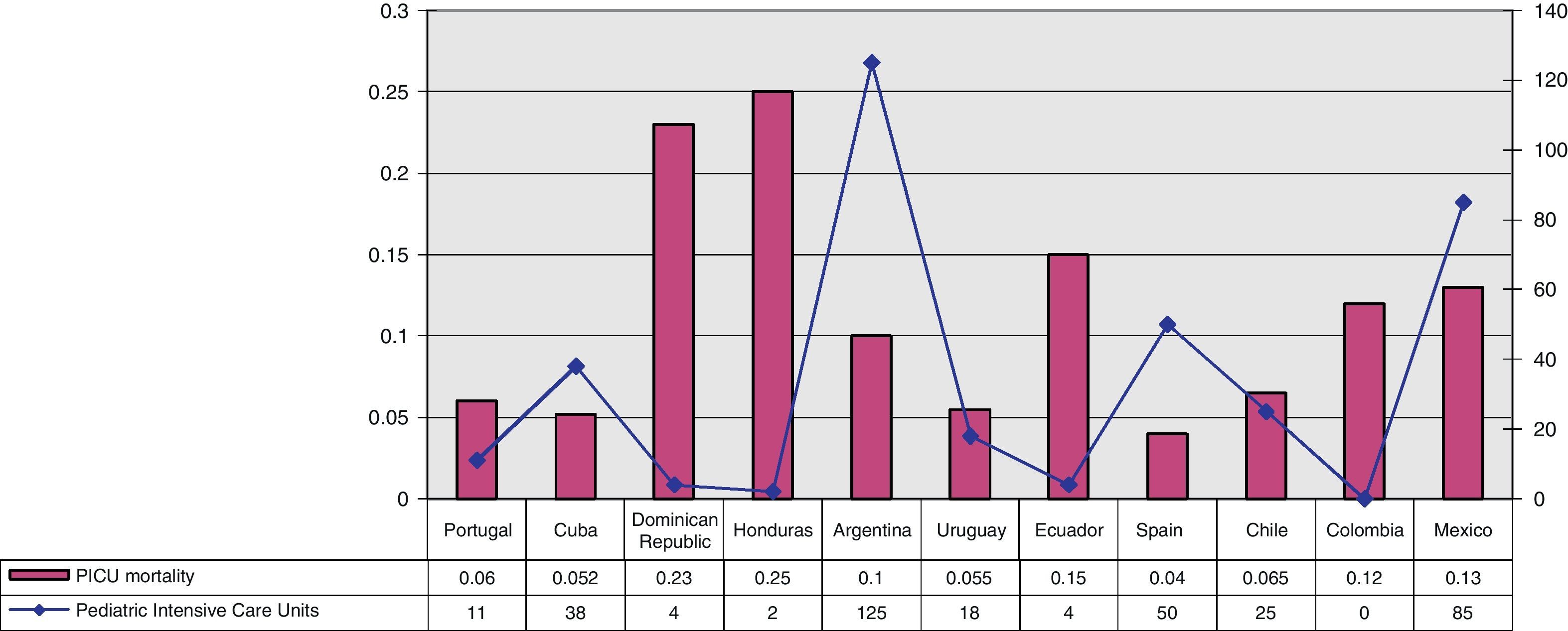
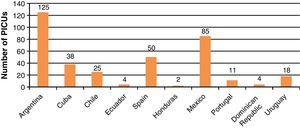
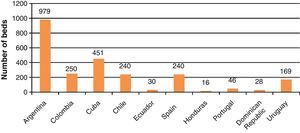
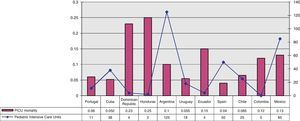
Fig. 2 reports the number of PICUs in the participating countries. The Dominican Republic, Honduras, Uruguay, and Ecuador have the fewest Units. In contrast, Spain, Argentina, and Mexico have the largest number of PICUs. The number of PICU beds was seen to range from 16 in Honduras to 979 in Argentina (Fig. 3). This information was not available in the case of the Mexican PICUs. Mention likewise was not made of the number of pediatric beds which some general hospital assign to children within adult ICUs. Globally, among the countries studied there was approximately one bed per 40,000 children.
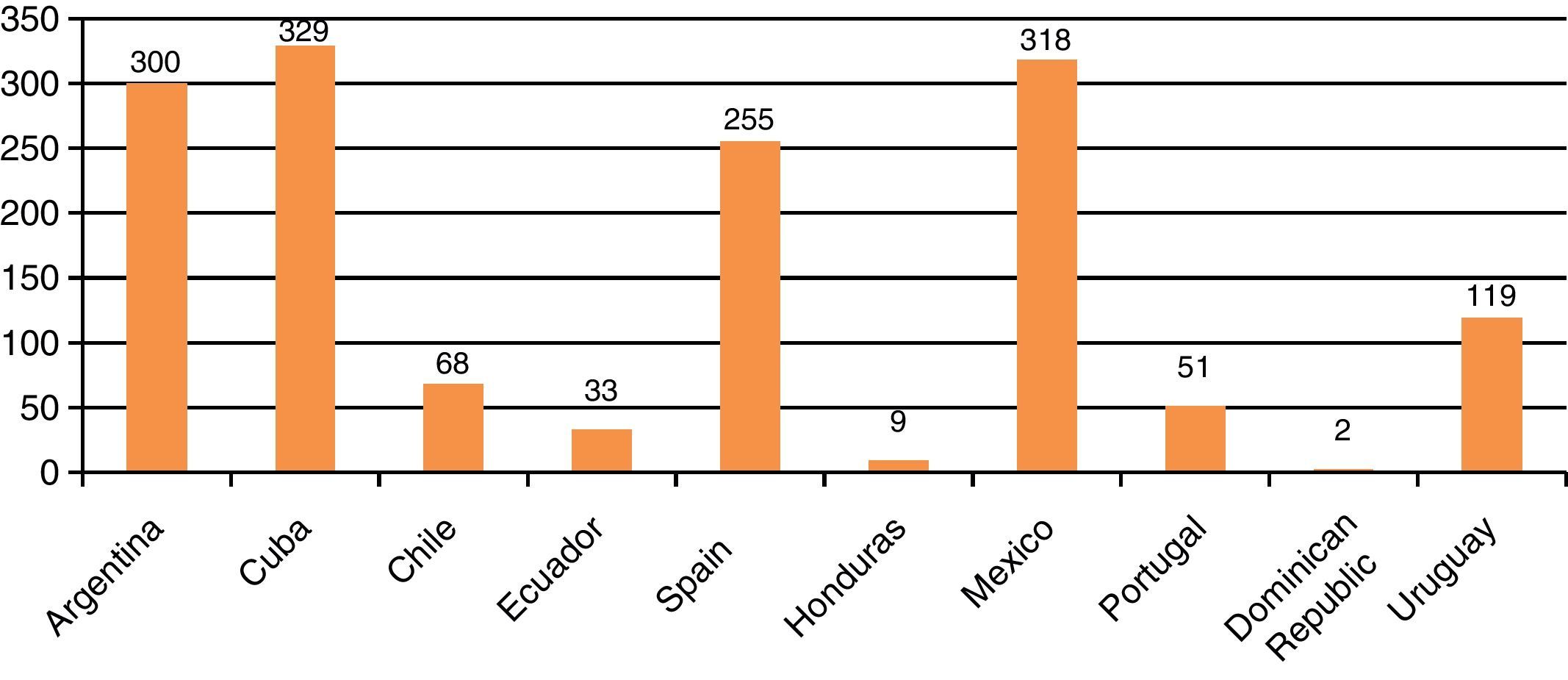
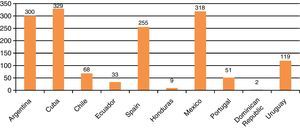
The number of pediatric intensivists was seen to be highly variable (Fig. 4). The countries with the greatest number of such specialists are Cuba, Argentina, Spain, and Mexico. In contrast, the Dominican Republic has two pediatric intensivists, Honduras has 9, and Ecuador has 33 (the number of members of the Ecuadorian Society of Pediatric Intensive Care was reported). Most of the countries, with the exception of these latter three, establish intensivist certification through University postgraduate training or formal recognition on the part of the respective professional societies or Medical Colleges.
The conditions most commonly dealt with in the PICUs of the Latin American countries were found to be postoperative support, infectious diseases, neurological disorders, respiratory processes, traumatisms, oncological diseases and immune depression, cardiovascular diseases, and intoxications. These conditions are related to the causes of infant mortality described above. Dengue was cited in one country (Dominican Republic), and intoxications in another (Ecuador).
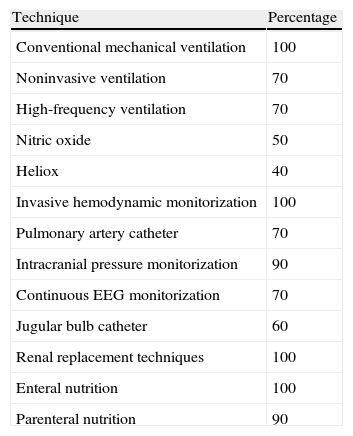
Table 3 reports the technological means available in the PICUs of the participating countries. Although almost all such Units are equipped with the basic technological means, certain forms of life support such as high-frequency ventilation, extracorporeal membrane oxygenation (ECMO), heliox, nitric oxide, continuous EEG monitorization, and jugular bulb catheterization are more limited. Significant differences were observed in PICU equipment within one same country, and even within one same city. As an example, access to noninvasive ventilation or high-frequency ventilation was seen to vary greatly.
Available technological resources in the Pediatric Intensive Care Units.
| Technique | Percentage |
| Conventional mechanical ventilation | 100 |
| Noninvasive ventilation | 70 |
| High-frequency ventilation | 70 |
| Nitric oxide | 50 |
| Heliox | 40 |
| Invasive hemodynamic monitorization | 100 |
| Pulmonary artery catheter | 70 |
| Intracranial pressure monitorization | 90 |
| Continuous EEG monitorization | 70 |
| Jugular bulb catheter | 60 |
| Renal replacement techniques | 100 |
| Enteral nutrition | 100 |
| Parenteral nutrition | 90 |
Mean PICU mortality in the studied countries was 12%, though this percentage ranged widely from 4% in Spain to 25% in Honduras (Table 1). The mean mortality in the Latin American PICUs was 13.29% versus 5% in the European Units–the difference between the two geographical settings being statistically significant (p=0.005) (Table 2, Fig. 5). Mortality in turn was inversely correlated to PICU availability, the number of pediatric intensivists, the number of beds, and the number of specialized pediatric centers. Lesser PICU accessibility was correlated to increased mortality. The cases of Honduras, the Dominican Republic and Ecuador illustrate this correlation (Fig. 6), which does not necessarily apply to all countries however. As an example, Mexico has a greater number of specialized pediatric centers, but mortality is comparable to that reported in Ecuador.
General organization of the specialtyOnly two countries, Cuba and Spain, have national clinical guides in the specialty. In 7 countries joint studies are made on a collaborative basis. Few countries have offered information on nosocomial infections.
Needs for the specialtyTen countries reported problems requiring immediate solutions. Most were referred to human resource and/or infrastructural shortcomings. In this context, mention is made of the need to increase the number of pediatric intensivists, nurses and residents. In addition, the need for intensivists with 24-h shifts or duties is cited, together with the need to reinforce the training programs targeted to all personnel, at either national level or through exchange programs with other countries. Regarding infrastructure, the need for more units, the creation of intermediate care units, or improvements in equipment has been cited. These concerns in turn are followed by the need for improved means for transporting critical children, and the need to introduce national norms referred to diagnosis and treatment. Other concerns refer to the lack of regionalization and equity, with a heterogeneous distribution of resources in which some geographical areas are well covered while others are completely devoid of adequate coverage. Likewise, some populations are cited as having easy access to the most modern care, while other populations lack practically everything. Less frequently cited (but equally important) concerns are the need for research activities, reliable registry methods for all intensive care variables, the need to develop home care and follow-up units, and the need to incorporate Ethics Committees.
DiscussionThe present report offers a regional perspective of the population and morbidity–mortality data of 9 Latin American and two European countries, related to a number of aspects such as hospital infrastructure, human and technological resources, and to PIC practice in each of them. One of the significant findings is the important presence of young individuals (population under 18 years of age) in the majority of the Latin American countries, and the fact that mortality in these countries is fundamentally associated to infections, respiratory failure, heart disease, traumatisms, neurological disorders, and oncohematological diseases.
The mortality figures differ significantly between the Latin American and European countries (Table 2). In Latin America, mortality is inversely correlated to PICU availability, the number of pediatric intensivists, the number of beds, and the number of specialized pediatric centers. The needs of the specialty as expressed by the participants in the study may help explain this situation, and include inequity and heterogeneity in the distribution of resources, and difficulties in accessing the existing services.
Access to emergency care in life-threatening situations constitutes a key health expectation for all communities. Medical care in general, and PIC in particular must contribute to satisfy these needs, with early and opportune interventions. This consideration in turn underscores the logical interaction that should exist between intensivists and the healthcare professionals that care for patients in life-threatening situations. The actions of the pediatric intensivist should not be confined or limited to the setting of the PICU.15
In some cases, deficiencies in first provided care and in the transport of critical children to specialized centers where PIC is available can explain the mortality figures reported in Latin American PICUs. In a study of 21 hospitals in 7 developing countries, initial screening or triage of 131 children was found to be inadequate or late in 8% of the cases; clinical evaluation was deficient in 41% of the children; and there were delays in the start of treatment in 19% of the patients.18 In another study, 50% of the in-hospital pediatric deaths occurred in the first 24h after admission.19 One of the factors that may explain this situation is that in general, the traditional training of healthcare professionals takes place in large urban hospital centers where emphasis is placed on diagnosis – leaving very little time for the teaching of the principles of emergency care. Accordingly, there is a marked difference between what is taught and what is really needed for resolving emergency situations. On the other hand, in many institutions there are very few professionals with formal training in intensive care, and those who are available are often poorly paid and frequently emigrate to other cities or countries.13
This report has a series of limitations that must be taken into account when interpreting the results obtained. Raw mortality data are presented, with no relation to severity scores–a fact that may partly explain the observed differences. The lack of reliable registries in most of the countries makes it difficult to present reliable and/or up to date information. As regards the needs of the specialty, those mentioned by the participants could be more related to their experience and the realities of their working environment than to the true situation of the country as a whole.
ConclusionThere are significant differences in population and morbidity–mortality among the studied countries. Mortality is inversely correlated to PICU availability, the number of pediatric intensivists, the number of beds, and the number of specialized pediatric centers. Logistic and financial limitations, deficiencies in the supporting disciplines (laboratory, imaging techniques, surgery, other sub-specialties), a precarious general patient condition secondary to advanced illness or denutrition, delays in admission and inadequate first provided treatments, a heterogeneous distribution of resources, and insufficient professional training in certain areas may all contribute significantly to mortality.
Financial supportNone.
Conflicts of interestThe authors declare no conflicts of interest.
Thanks are due to the professionals who contributed information for the preparation of this report: L. Albano, D. Rufach, S. Santos and L. Saligari (Argentina); C. de Villegas (Bolivia); L.C. Maya, B. Giraldo and G. Cassalett (Colombia); B.L. Castro, M. Machado and L. Ibargollen (Cuba); C. Valdevenito (Chile); L. Eguiguren, E. Quiñones, S. Morales, F. Aguinaga and D. Granda (Ecuador); A. Palomeque and C. Rey (Spain); L. Moya (Guatemala); W. Moncada and M. Matamoros (Honduras); M. Correa and A. Román (Mexico); A. Dinis, V. Alves, C. Duarte, A. Ribeiro, E. Santos, H. Almeida, L. Matos, J. Rosas and E. Costa (Portugal); P. Rosich (Dominican Republic); and O.R. Bello, L. Mátrai, B. Silva and A. Aguilar (Uruguay).
Please cite this article as: Campos-Miño S, et al. Los cuidados intensivos pediátricos en Latinoamérica. Med Intensiva. 2012;36:3–10.