Comparar la prevalencia y características del síndrome post-cuidados intensivos paciente (SPCI-P) y familiar/cuidador (SPCI-F) en dos cohortes (COVID y no COVID) y analizar factores riesgo de SPCI-P.
DiseñoProspectivo, observacional cohortes (marzo 2018-2023), seguimiento a tres meses y al año.
ÁmbitoUnidad de Cuidados Intensivos (UCI) polivalente, 14 camas, hospital nivel II.
Pacientes o participantesPacientes: 265, familiares: 209. Criterios de inclusión pacientes: edad>18 años, ventilación mecánica>48 horas, estancia UCI>5 días, delirium, shock séptico, síndrome de distrés respiratorio agudo, parada cardiaca. Criterios de inclusión familiares: acudir a consulta.
IntervencionesSeguimiento a tres meses y al año del alta hospitalaria.
Variables de interés principalesPacientes: sociodemográficas, clínicas, evolutivas, alteraciones físicas, psíquicas y cognitivas, dependencia y calidad de vida. Familiares: estado mental y sobrecarga física.
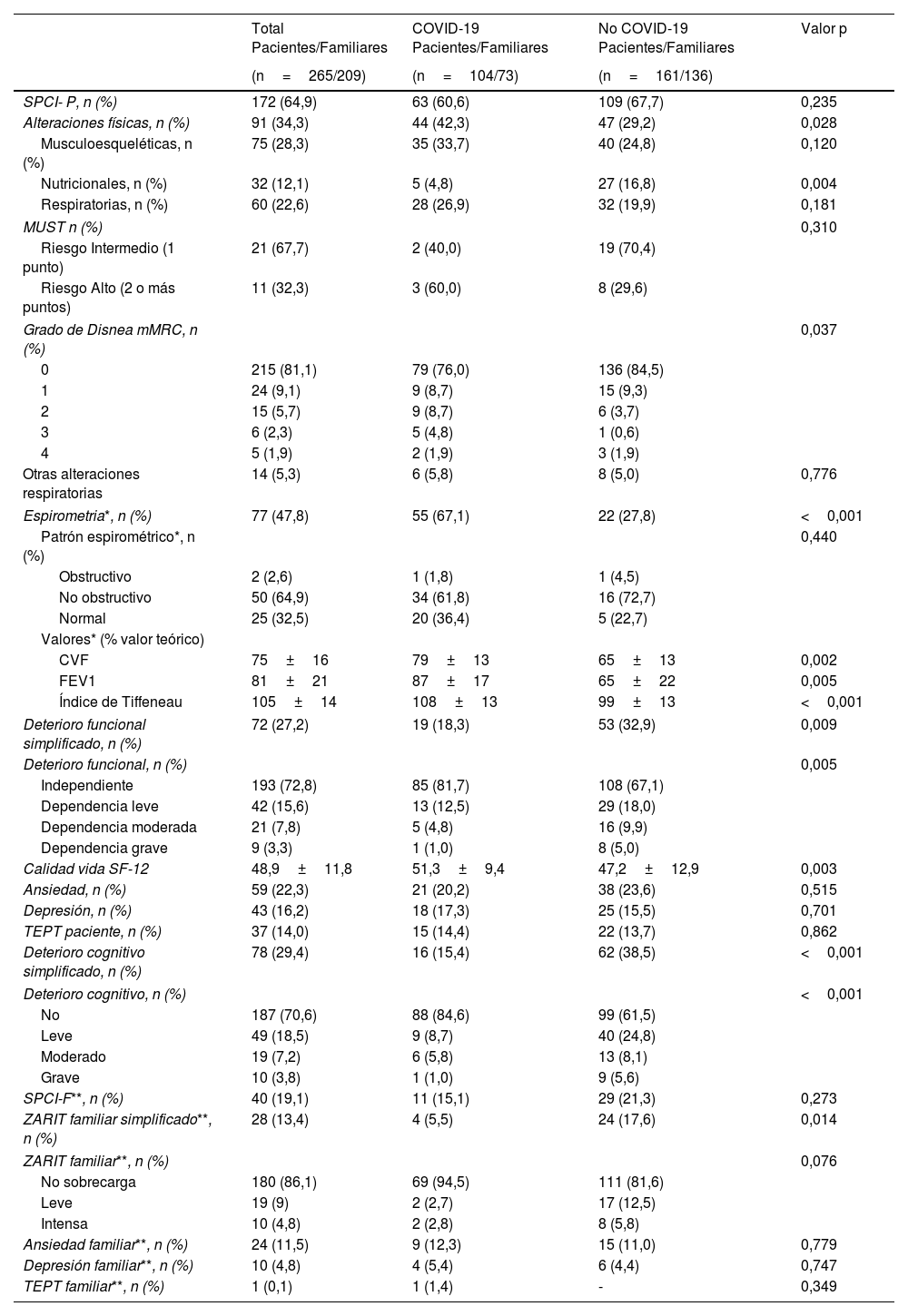
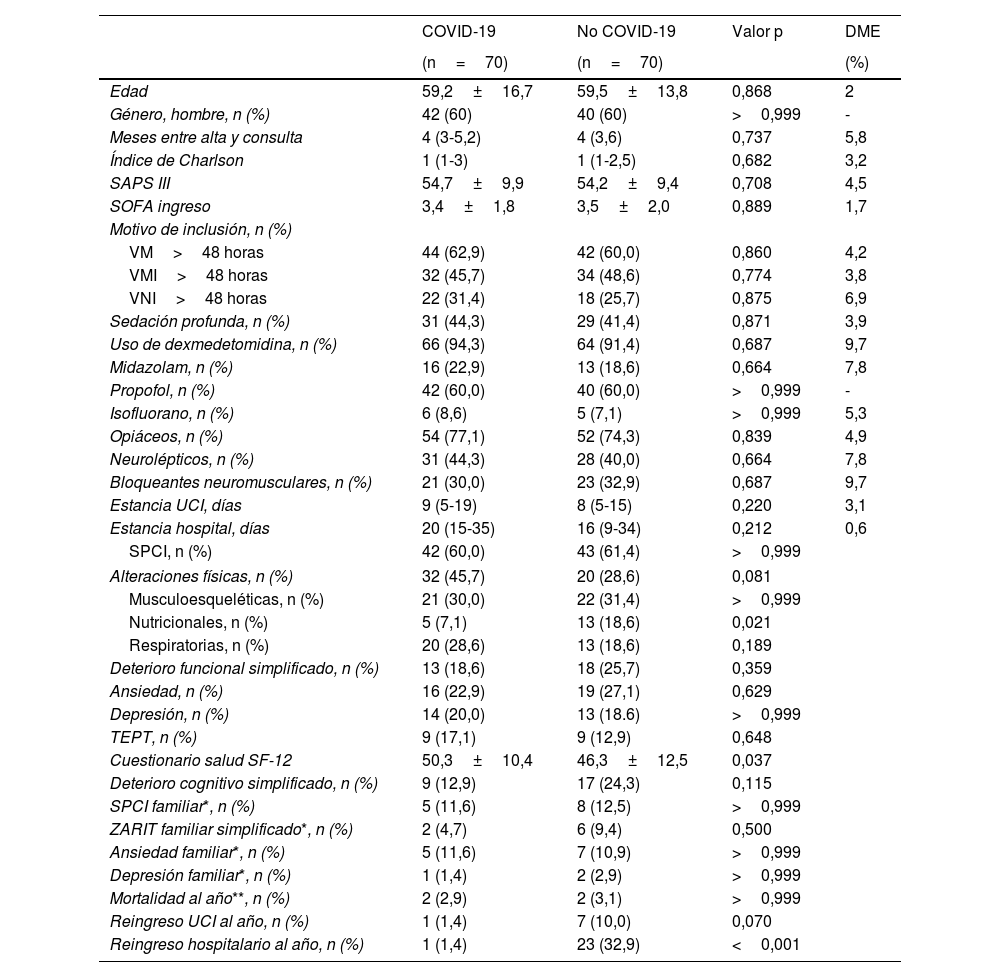
ResultadosSPCI-P 64,9%, sin diferencias entre grupos. Pacientes COVID más alteraciones físicas que los no-COVID (p=0,028). Estos últimos mayor deterioro funcional (p=0,005), peor calidad de vida (p=0,003), más alteraciones nutricionales (p=0,004) y deterioro cognitivo (p<0,001). SPCI-F 19,1%, más frecuente en familiares de pacientes no-COVID (17,6% vs. 5,5%; p=0,013). Factores predictivos independientes de SPCI-P: primeros años estudio (OR: 0,484), mayor comorbilidad (OR: 1,158), delirium (OR: 2,935), varios motivos de inclusión consulta (OR: 3,171) y midazolam (OR: 4,265).
ConclusionesPrevalencia de SPCI-P y SPCI-F similar en ambas cohortes. Principales factores asociados a SPCI-P: mayor comorbilidad, delirium, midazolam, haber sido incluido en la consulta por más de un motivo y primeros años del estudio.
Compare prevalence and profile of post-intensive care patient (P-PICS) and family/caregiver (F-PICS) syndrome in two cohorts (COVID and non-COVID) and analyse risk factors for P-PICS.
DesignProspective, observational cohort (March 2018- 2023), follow-up at three months and one year.
Setting14-bed polyvalent Intensive Care Unit (ICU), Level II Hospital.
Patients or participants265 patients and 209 relatives. Inclusion criteria patients: age> 18 years, mechanical ventilation> 48hours, ICU stay> 5 days, delirium, septic shock, acute respiratory distress syndrome, cardiac arrest. Inclusion criteria family: those who attended.
InterventionsFollow-up 3 months and 1 year after hospital discharge.
Main variables of interestPatients; sociodemographic, clinical, evolutive, physical, psychological and cognitive alterations, dependency degree and quality of life. Main caregivers: mental state and physical overload.
Results64.9% PICS-P, no differences between groups. COVID patients more physical alterations than non-COVID (p=0.028). These more functional deterioration (p=0.005), poorer quality of life (p=0.003), higher nutritional alterations (p=0.004) and cognitive deterioration (p<0.001). 19.1% PICS-F, more frequent in relatives of non-COVID patients (17.6% vs. 5.5%; p=0.013). Independent predictors of PICS-P: first years of the study (OR: 0.484), higher comorbidity (OR: 1.158), delirium (OR: 2.935), several reasons for being included (OR: 3.171) and midazolam (OR: 4.265).
ConclusionsPrevalence PICS-P and PICS-F between both cohorts was similar. Main factors associated with the development of SPCI-P were: higher comorbidity, delirium, midazolam, inclusion for more than one reason and during the first years.
Article
Go to the members area of the website of the SEMICYUC (www.semicyuc.org )and click the link to the magazine.