To determine the incidence and characteristics of mental disorders (MD) in the Intensive Care Unit (ICU), and to define a classification system adapted to the ICU environment.
DesignA retrospective, descriptive analysis.
SettingIntensive Care Unit, Arnau de Vilanova Hospital in Lérida (Spain).
PatientsAll patients with MD admitted during 5-year period (January, 1 2004 to December 31, 2008).
Main variablesGeneral variables included clinical-demographic data, diagnostic variables, procedures, severity score, length of stay and mortality. Specific variables included psychiatric history, screening for substance abuse, psychiatric assessment, monitoring and transfer to a psychiatric center. Classification of the MD was as follows: (1) acute substance intoxication (SI); (2) suicide attempts (SA); and (3) MD associated with the main diagnosis (AMD).
ResultsA total of 146 patients had MD (7.8%); they were predominantly male (74%) and were younger than the general ICU population (43.9 years vs 55.3 years, p<0.001). The ICU stays of the patients with MDs were shorter (4 days vs 7 days, p<0.001), and there was less hospital mortality (17.1% vs 25%, p<0.05). They also showed a higher incidence of pneumonia (19.9% vs 13.8%, p<0.05), but no differences in the level of severity were observed. The SI group (24.7%) contained the highest number of young people; the SA group (36.3%) showed a predominance of women; and the AMD (39%) group had the longest stays and the highest mortality. Psychiatric consultation was carried out mainly in the SA group (62.3%).
ConclusionsMD is a relatively common problem in the ICU. Collaboration with the Psychiatry Department seldom occurs, but must be encouraged to develop fully integrated management of critical patients with MD.
Conocer la incidencia y características del trastorno mental (TM) en la UCI y definir una clasificación adaptada al entorno de UCI.
DiseñoEstudio descriptivo y retrospectivo.
ÁmbitoUnidad de Cuidados Intensivos polivalente del Hospital Universitario Arnau de Vilanova de Lérida.
PacientesSe incluyó 146 pacientes que ingresaron con TM durante un periodo de 5 años (1 de enero de 2004 a 31 de diciembre de 2008).
Variables de interésVariables generales: clínico-demográficas, diagnóstico, procedimientos, gravedad, estancia y mortalidad. Variables específicas: antecedentes psiquiátricos, screening de tóxicos, valoración psiquiátrica, seguimiento y traslado a centro psiquiátrico. Clasificación del TM: 1) intoxicación aguda por sustancias (IS), 2) intento autolítico (IA) y 3) trastorno mental asociado al diagnóstico principal (TA).
ResultadosUn total de 146 pacientes con TM (7,8%). Predominio de varones (74%) y más jóvenes (43,9 vs. 55,3 años, p<0,001). La estancia en la UCI fue más corta (4 días vs. 7 días, p<0,001) y hubo menor mortalidad hospitalaria (17,1 vs. 25%, p<0,05). Sin diferencias en nivel de gravedad pero más incidencia de neumonía (19,9 vs. 13,8%, p<0,05). El grupo IS (24,7%), más jóvenes, el grupo IA (36,3%) con predominio de mujeres y TA (39%) con estancia y mortalidad más altas. La consulta a Psiquiatría se realizó prioritariamente en IA (62,3%).
ConclusionesEl TM es un problema relativamente frecuente en UCI. La colaboración con Psiquiatría es minoritaria y debe ser potenciada para conseguir un manejo integral del paciente crítico con TM.
Mental disorders (MDs) are a common problem in western society, and cause important disability. MDs are defined as any generic alteration of mental health, related or not to some known underlying somatic condition. The term MD includes psychotic and/or affective disorders, as well as problems resulting from substance abuse or dependency. The prevalence of these diseases has been well defined in the general population, though few studies have evaluated MDs in critically ill patients.1 While there has been an increase in the number of psychiatric Intensive Care Units (ICUs) specialized in the management of acute MD decompensation, the indicated specific care of such patients when admitted to a polyvalent ICU remains unclear.2 One of the main problems in this context is the difficulty for intensivists to define the different MDs, since specific biomarkers are lacking, and non-psychiatric physicians—including intensivists—are scantly familiarized with the management and diagnosis of these disorders.3 MDs are present in ICUs, where three different scenarios can be found: admission due to acute substance abuse,4 attempted suicide,5 and MD as a comorbidity factor.6
The incidence of the different MDs in the critical patient has not been well established, and little is known of their influence upon the prognosis of the critical condition, or of the need for specific care from the psychiatric perspective.7
In addition, the aforementioned three scenarios do not always manifest independently. The association between substance abuse and other MDs has been well established, and there have been descriptions of combined depression, substance abuse and attempted suicide.8 All this complicates adequate evaluation by the non-psychiatric physician, and requires coordination with the Psychiatry Department to ensure adequate analysis and treatment of the psychopathological condition of the patient.9
Few studies to date have investigated MDs in the Intensive Care setting. The present observational study has been designed to describe the frequency of MDs, their differential characteristics, and impact upon critical patient prognosis and mortality.
Patients and methodsA retrospective study was made of all the patients admitted to our ICU (Arnau de Vilanova University Hospital in Lérida, Spain) between January 2004 and December 2008. We excluded patients under 14 years of age, subjects with incomplete information, and stays of less than 24h. Demographic data were collected, together with the APACHE II severity score, the Glasgow score upon admission, ICU procedures (mechanical ventilation [MV], use of noradrenalin, total parenteral nutrition [TPN] and sedation), stay, in-hospital mortality and infectious complications defined as the presence of pneumonia (PN) according to the criteria published by the CDC.10
The patients were classified into 7 diagnostic categories (adapting the classification to the sample size and characteristics of our case-mix): head injuries (HIs), polytraumatism without HIs, neurological, respiratory, surgical, sepsis, and others.
The patients with MDs were divided into three groups: (1) acute substance intoxication (SI) (alcohol, cannabis, cocaine, opioids, methadone, ecstasy, and amphetamines); (2) attempted suicide (AS) (involving drugs or otherwise); and (3) MDs associated with the main diagnosis (AMD) — which included patients admitted for any reason, with a history of MD accompanied by a typified diagnosis and monitored by a specialist in psychiatry. Four AMD subgroups were established: AMD related to substances (AMDS), AMD with a diagnosis of schizophrenia and other psychotic disorders (including bipolar disorder with psychotic symptoms) (AMDP), AMD with mood disorders (AMDM), and MDs with anxiety disorders (MDA).
Substance intoxication, alcohol abuse, and the different types of MDs were defined following the category-based diagnostic classification of the Disease and Statistical Manual of Mental Disorders edition 4 (DSM-IV-TR). Suicide attempt is not typified as a diagnostic group in the DSM-IV-TR.3
In the patients with MDs we added specific variables referred to the existence of previous psychiatric disease, previous suicide attempts, the determination of toxic substances, the conduction of psychiatric evaluations, follow-up and transfer to the Psychiatry Department (which in our case requires moving the patient to another hospital). For the determination of toxic substances in urine, use was made of a rapid qualitative immunochromatographic multidrug detection test (INSTANT-VIEW®, Alfa Scientific Designs (INC, Poway, CA 92064-USA). This test yields a positive result when the drug concentration exceeds 125% of the established cutoff value.
The study was approved by the Clinical Research Ethics Committee of our center.
Statistical analysisContinuous variables are reported as the mean±standard deviation (SD), median (interquartile range), or as a percentage. The comparison of categorical variables was based on the chi-squared test, the nonparametric Mann–Whitney U-test, or the Kruskal–Wallis test for continuous variables.
The SPSS version 16.0 statistical package was used. Statistically significant differences were considered for p<0.05.
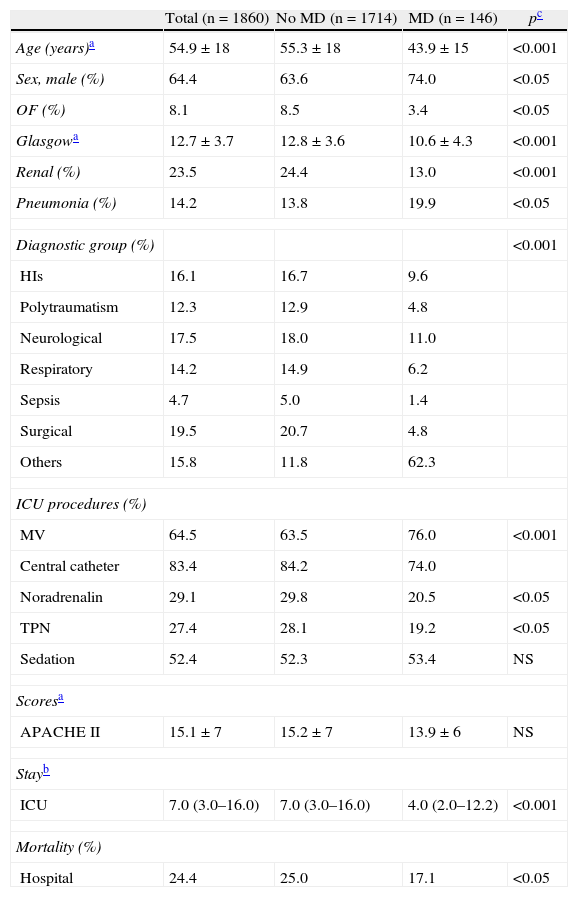
ResultsDuring the study period, a total of 1860 patients were admitted to the ICU. Of these, 146 (7.8%) patients presented MDs. Table 1 describes the clinical-demographic characteristics of the study group. The patients with MD were significantly younger, predominantly males, and had fewer antecedents of prior organic disease (3.4% vs 8.5%; p<0.05). Significant differences were also observed with regard to the typical procedures carried out in the ICU, with a greater use of mechanical ventilation and a lesser need for vasoactive medication and TPN – though no differences were observed in terms of the need for sedation. No differences were established as regards the APACHE II severity score (13.9±7 vs 15.4±8), though in-hospital mortality was significantly lower (17.1% vs 25%; p<0.05), and both ICU and hospital stay were shorter.
Clinical-demographic characteristics of the patients admitted to the ICU.
| Total (n=1860) | No MD (n=1714) | MD (n=146) | pc | |
| Age (years)a | 54.9±18 | 55.3±18 | 43.9±15 | <0.001 |
| Sex, male (%) | 64.4 | 63.6 | 74.0 | <0.05 |
| OF (%) | 8.1 | 8.5 | 3.4 | <0.05 |
| Glasgowa | 12.7±3.7 | 12.8±3.6 | 10.6±4.3 | <0.001 |
| Renal (%) | 23.5 | 24.4 | 13.0 | <0.001 |
| Pneumonia (%) | 14.2 | 13.8 | 19.9 | <0.05 |
| Diagnostic group (%) | <0.001 | |||
| HIs | 16.1 | 16.7 | 9.6 | |
| Polytraumatism | 12.3 | 12.9 | 4.8 | |
| Neurological | 17.5 | 18.0 | 11.0 | |
| Respiratory | 14.2 | 14.9 | 6.2 | |
| Sepsis | 4.7 | 5.0 | 1.4 | |
| Surgical | 19.5 | 20.7 | 4.8 | |
| Others | 15.8 | 11.8 | 62.3 | |
| ICU procedures (%) | ||||
| MV | 64.5 | 63.5 | 76.0 | <0.001 |
| Central catheter | 83.4 | 84.2 | 74.0 | |
| Noradrenalin | 29.1 | 29.8 | 20.5 | <0.05 |
| TPN | 27.4 | 28.1 | 19.2 | <0.05 |
| Sedation | 52.4 | 52.3 | 53.4 | NS |
| Scoresa | ||||
| APACHE II | 15.1±7 | 15.2±7 | 13.9±6 | NS |
| Stayb | ||||
| ICU | 7.0 (3.0–16.0) | 7.0 (3.0–16.0) | 4.0 (2.0–12.2) | <0.001 |
| Mortality (%) | ||||
| Hospital | 24.4 | 25.0 | 17.1 | <0.05 |
Glasgow: Glasgow Coma Score; OF: chronic organic failure; TPN: total parenteral nutrition; Renal: acute renal failure; HIs: head injuries; MD: mental disorder; MV: mechanical ventilation.
Mean±standard deviation.
Median (interquartile range).
Comparison between groups; p-value determined by the χ2 test, for the comparison of proportions, or the Mann–Whitney U-test for continuous variables.
Renal failure was less frequent in the patients with MD (13% vs 24.4%; p<0.001), though the incidence of pneumonia was comparatively higher (19.9% vs 13.8%; p<0.05).
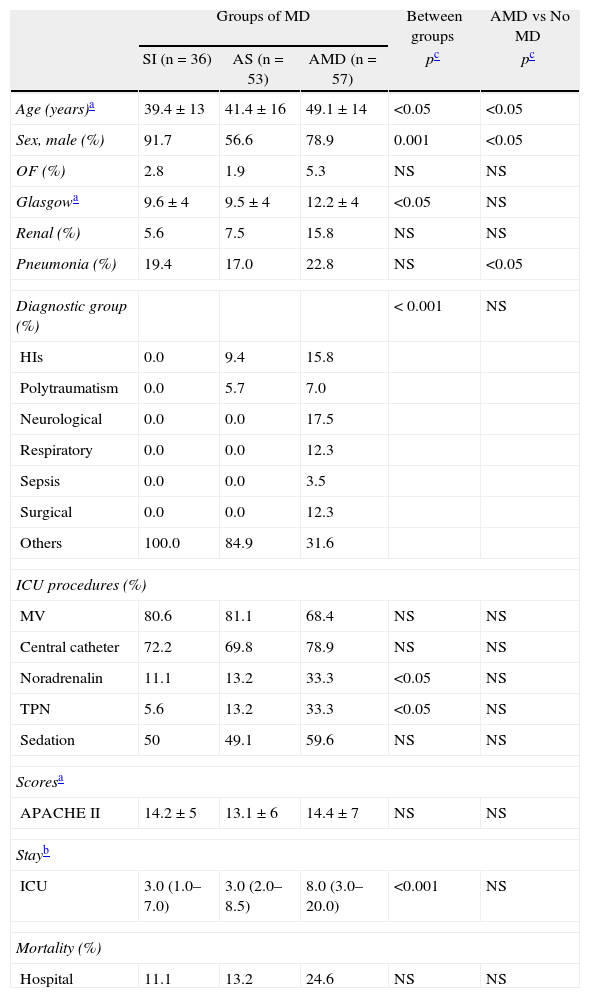
On stratifying the patients with MDs according to the main reason for admission, the characteristics were seen to differ (Table 2).
Clinical-demographic characteristics according to diagnostic group.
| Groups of MD | Between groups | AMD vs No MD | |||
| SI (n=36) | AS (n=53) | AMD (n=57) | pc | pc | |
| Age (years)a | 39.4±13 | 41.4±16 | 49.1±14 | <0.05 | <0.05 |
| Sex, male (%) | 91.7 | 56.6 | 78.9 | 0.001 | <0.05 |
| OF (%) | 2.8 | 1.9 | 5.3 | NS | NS |
| Glasgowa | 9.6±4 | 9.5±4 | 12.2±4 | <0.05 | NS |
| Renal (%) | 5.6 | 7.5 | 15.8 | NS | NS |
| Pneumonia (%) | 19.4 | 17.0 | 22.8 | NS | <0.05 |
| Diagnostic group (%) | < 0.001 | NS | |||
| HIs | 0.0 | 9.4 | 15.8 | ||
| Polytraumatism | 0.0 | 5.7 | 7.0 | ||
| Neurological | 0.0 | 0.0 | 17.5 | ||
| Respiratory | 0.0 | 0.0 | 12.3 | ||
| Sepsis | 0.0 | 0.0 | 3.5 | ||
| Surgical | 0.0 | 0.0 | 12.3 | ||
| Others | 100.0 | 84.9 | 31.6 | ||
| ICU procedures (%) | |||||
| MV | 80.6 | 81.1 | 68.4 | NS | NS |
| Central catheter | 72.2 | 69.8 | 78.9 | NS | NS |
| Noradrenalin | 11.1 | 13.2 | 33.3 | <0.05 | NS |
| TPN | 5.6 | 13.2 | 33.3 | <0.05 | NS |
| Sedation | 50 | 49.1 | 59.6 | NS | NS |
| Scoresa | |||||
| APACHE II | 14.2±5 | 13.1±6 | 14.4±7 | NS | NS |
| Stayb | |||||
| ICU | 3.0 (1.0–7.0) | 3.0 (2.0–8.5) | 8.0 (3.0–20.0) | <0.001 | NS |
| Mortality (%) | |||||
| Hospital | 11.1 | 13.2 | 24.6 | NS | NS |
Glasgow: Glasgow Coma Score; AS: attempted suicide; SI: acute substance intoxication; TPN: total parenteral nutrition; Renal: acute renal failure; AMD: mental disorder associated to main diagnosis; HIs: head injuries; MD: mental disorder; MV: mechanical ventilation.
Mean±standard deviation.
Median (interquartile range).
Comparison between groups; p-value determined by the χ2-test, for the comparison of proportions, or the Mann–Whitney U-test for continuous variables.
Thirty-six patients were admitted due to SI. Alcohol abuse was present in 22 of these 36 cases, and the detection of toxic substances in urine proved positive in 26 of the 28 individuals in which such testing was performed. The most commonly consumed illegal substance was cocaine (11 cases), followed by cannabis (5 cases), ecstasy (2 cases), and amphetamines (2 cases). Opioid detection proved positive in 8 cases, and 5 of these patients had a history of heroin abuse. Methadone positivity in turn was recorded in 10 cases. In 62% of the cases intoxication was due to two or more substances. The SI group was younger, with a mean age of 39.4±13 years, a clear male predominance (91.7%), and a scant need for inotropic drugs or TPN. Of note was their low Glasgow score and a severity score similar to that of the other groups, but with short stay and low mortality.
The AS group in turn comprised 53 individuals, with a greater presence of women in this case (43.4%), and low sedation requirements. Most AS were related to drug overdose (37 patients) – fundamentally psychoactive medication. The remaining 16 suicide attempts involved different mechanisms: hanging (4 cases), falls (4 cases), firearm (2 cases), the ingestion of organophosphorus compounds (3 cases), and the ingestion of caustic agents (2 cases).
In the AMD group (57 patients), and considering the four subgroups, there were 31 subjects with AMDS, 13 with AMDP, 9 with AMDM and 4 with MDA. This was the oldest group, with a mean age of 49±14 years, and again showed a clear male predominance (78.9%).
Table 2 also shows the results of the comparison between the AMD group and the non-mental disease patients (data reported in Table 1).
Differences were found in the AMD group, with a greater percentage of males, a younger age and a higher pneumonia rate. In the diagnostic groups, and although statistical significance was not reached because of the small sample sizes involved, the percentage of other disorders was greater in AMD (31.6% vs 11.8%). The most frequent diagnoses in this group were: 5 cases of gastroenteritis (8.7% of the AMD) with important dehydration, 4 cases of pancreatitis (7.0%) and 3 cases of diabetic ketoacidosis (5.3%).
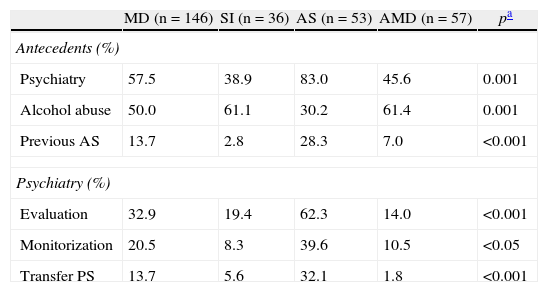
In the SI and AS groups, as expected, associations to other psychiatric conditions were observed. Specifically, 39% of the patients with SI had a history of previous psychiatric disease, while in the AS group this percentage reached 83% - with a predominance of major depression (19 patients). Alcohol abuse was present in 50% of the cases. A request for psychiatric assessment was made in 32.9% of the patients, and approximately 60% of the consulted cases required specialized monitorization. Such interconsultation fundamentally occurred in the AS group, where 32.1% of the subjects required transfer to a psychiatric center (Table 3).
Clinical characteristics specific of the study group.
| MD (n=146) | SI (n=36) | AS (n=53) | AMD (n=57) | pa | |
| Antecedents (%) | |||||
| Psychiatry | 57.5 | 38.9 | 83.0 | 45.6 | 0.001 |
| Alcohol abuse | 50.0 | 61.1 | 30.2 | 61.4 | 0.001 |
| Previous AS | 13.7 | 2.8 | 28.3 | 7.0 | <0.001 |
| Psychiatry (%) | |||||
| Evaluation | 32.9 | 19.4 | 62.3 | 14.0 | <0.001 |
| Monitorization | 20.5 | 8.3 | 39.6 | 10.5 | <0.05 |
| Transfer PS | 13.7 | 5.6 | 32.1 | 1.8 | <0.001 |
AS: attempted suicide; Previous AS: previous attempted suicide; SI: acute substance intoxication; AMD: mental disorder associated to main diagnosis; MD: mental disorder; Transfer PS: transfer to a psychiatric center.
Comparison between groups; p-value determined by the χ2-test.
Urine testing for toxic agents was performed in 62 patients (42.5%), particularly in individuals admitted due to SI—where the test was performed in 77.8% of the cases. Of note is the fact that 90.3% of the determinations proved positive—this showing that urine testing was only carried out when there was a strong suspicion of intoxication.
DiscussionAlmost 8% of all patients admitted to an ICU suffer some mental disorder (MD) as either the main reason for admission, or as an antecedent accompanying the critical disease process. The recorded incidence is clearly lower than that published for patients admitted to hospital wards, where the figure can reach 30% according to some series.7 The mentioned lesser incidence could be due to limitations in healthcare resources that make it necessary to rationalize the ICU beds—as a result of which the admission of patients with severe MDs may be rejected.11 The availability of beds—very restricted for our reference area—influences the decision to admit patients with previous limiting comorbidity such as serious psychiatric problems, and in certain cases also makes it necessary to attend some patients in other non-critical hospital areas.
Our results show that patients with MDs are young and predominantly of the male sex, with few antecedents of chronic organic disease, a low Glasgow score, lesser mortality, and shorter stays. These characteristics are similar to those published in other series,12,13 and could be explained by a greater presence of rapidly reverting neurological disease, no serious lung damage, and the absence of previous organic disease.
We recorded a high incidence of pneumonia in the study group, attributable in part to the increased need for mechanical ventilation and the low initial Glasgow score.14 The association of psychiatric comorbidity to pneumonia has already been observed in earlier studies, and has been attributed to factors such as malnutrition, poor dental hygiene, altered neutrophil function, bacterial translocation, or alveolar surfactant dysfunction.15–17
There are controversial findings on the influence of psychiatric comorbidity upon patient mortality. In our series, the critical patients with associated psychiatric problems did not have a greater mortality rate than the general population admitted to ICUs.12,18,19 An important part of our study group consisted of patients with drug-induced attempted suicide (AS) and substance intoxication (SI) in which the fundamental problem is a consequence of respiratory depression—with low mortality provided early medical care is provided. Obviously, these data refer to those patients who reach the ICU. In contrast, other published studies have reported increased mortality in the general population addicted to drug substances.20
Those patients admitted for reasons directly related to MDs such as SI and AS present characteristics that are different from those of the general population in ICUs. The patients admitted due to SI were the youngest group, with a clear male predominance, and usually presented antecedents of abuse of more than one drug substance. Substance abuse remains one of the most important public health problems in modern society, and although the mortality rate of subjects admitted to the ICU due to SI is low, bias is generated as a result of the deaths that occur before the patient reaches the hospital.21,22 Within the SI group, and in coincidence with earlier studies, medicinal overdose was the most frequent presentation, with a greater presence of women and of previous psychiatric antecedents.8 Of note was the low mortality corresponding to drug-induced AS (8%), while in contrast the mortality rate of non-drug-induced AS was 18%. This is to be expected, since more violent methods such as hanging or falls tend to indicate a strong suicidal intent.23
The group with MDs associated to the main diagnosis (AMD) generally behaved similarly to those critical patients without psychiatric comorbidity, though they also showed a higher incidence of pneumonia that cannot be attributed to the Glasgow score or to the need for mechanical ventilation, which was comparable to that of the general population in the ICU. Alcohol abuse and the predisposition to respiratory alterations in certain psychiatric illnesses such as schizophrenia could help explain this increased incidence.16,24
The combination of medical and mental disease makes it necessary to incorporate mental health care to the management of critical patients. To this effect it is essential to establish collaboration with the Psychiatry Department, in order to coordinate medical care with the analysis and treatment of the psychiatric comorbidity.9 Liaison psychiatry, defined as those activities of the Psychiatry Department in non-psychiatric areas of the general hospital, serves to afford early management of patient psychiatric problems in the different medical departments, and thus improve the quality of patient care.25
In our study, psychiatric assessment and monitorization or follow-up was requested mainly in the case of patients with attempted suicide—one-third of which were moved to the Psychiatry Department once their medical problem was stabilized.
Clearly, AS alerts the intensivist to the possibility of a new suicide attempt after discharge from the ICU, particularly if the patient is to continue recovery in a hospital ward lacking due safety measures.26
The results of our study underscore the low incidence of psychiatric care in the subgroup of patients admitted with associated MDs and in the case of substance abuse.6
The present study has a number of limitations. A first limitation is the retrospective analysis of the data, the limited sample size, and the fact that the study has been carried out in a single ICU with its own specific sociodemographic characteristics. Another limitation is referred to the difficulty of diagnosing toxic substance abuse in the critical patient, since the screening of such substances has not been standardized in our ICU, and as has been reported above, testing in urine was only carried out when there was a strong suspicion of abuse. In our experience, intensivists do not routinely determine the presence of substance abuse, and the patients in turn are usually unable to provide information because of their diminished level of consciousness at the time of admission to the ICU. Blood alcohol testing was likewise not performed on a routine basis (only when legally demanded). In the case of rest of the psychiatric disorders, the limited training of intensivists in MDs does not allow the necessary precision in diagnosing the severity of the mental condition, and such information is therefore not entered in the case history. The same shortcomings apply to the correct identification of attempted suicide masked behind an apparently casual fall or traffic accident.27
Our findings, which could be generalized to other ICUs, show that psychiatric care should be reinforced in patients with MDs, with improved training of our personnel (including residents) in this field.25 According to our data, the existence of a history of MD does not imply a poorer prognosis, and this criterion should be re-evaluated when deciding admission to the ICU of patients of this kind.
The contribution of psychiatry in the ICU should cover aspects of the three groups which we have defined in this study. Improvement in the management of patients of this kind includes reinforcement of the role of the psychiatrist in the integral care of the patient once the acute phase of the critical condition has been passed. In acute substance intoxication, the psychiatrist can help assess the disintoxication treatment needs and start follow-up; in cases of attempted suicide the psychiatrist can help by assessing the risk of repeated attempts and advising institutionalized care if needed; and in the case of associated disorders, advice can be provided on the improved management of specific medication that can be prescribed on a chronic basis, with posterior follow-up.28,29 Psychiatrist contact with the family of the patient (which may feel more motivated in a critical phase of the background problem) in turn may represent an advantage in terms of integral care.
The described classification aims to address the most frequent psychiatric problems seen in the ICU from a practical perspective, differentiating between those conditions which are the main reasons for admission and those that accompany the critical disorder. Prospective studies are needed to investigate the admission of patients with MDs to the ICU and to further assess their impact upon the critical illness—opening the field to new therapeutic strategies and favoring increased psychiatrist participation in the ICU.30
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Badia M, et al. Clasificación de los trastornos mentales en la Unidad de Cuidados Intensivos. Med Intensiva. 2011;35:539–45.