The management of critically ill cancer patients at the ICU setting is a complex challenge that requires a solid evidence base to optimize clinical decision-making. One of the main obstacles in this context is the lack of mortality predictive models specific to this population, which compromises the objectivity of prognosis and fosters the influence of cognitive biases in clinical practice.1 Traditionally used ICU prognostic models, such as APACHE II and SOFA, do not incorporate functional parameters, thus limiting their applicability and accuracy in critically ill cancer patients.2,3 In this regard, integrating variables related to functional status, such as the ECOG scale, could improve predictive capacity and offer a more personalized approach to patient care.4
Despite efforts to develop effective prognostic tools, none of the existing models have yet achieved the necessary accuracy for validation specifically in critically ill cancer patients.5 To address this gap, we conducted a prospective cohort study from August 24th, 2018 through November 19th 2021, at a tertiary teaching hospital. A total of 215 patients with solid tumors who experienced acute episodes and were evaluated for ICU admission—whether they were ultimately admitted or denied access—were included. The primary endpoint of the study was to develop mortality predictive models at 6 months for this specific population. The study was approved by the Cantabria Ethics Committee.
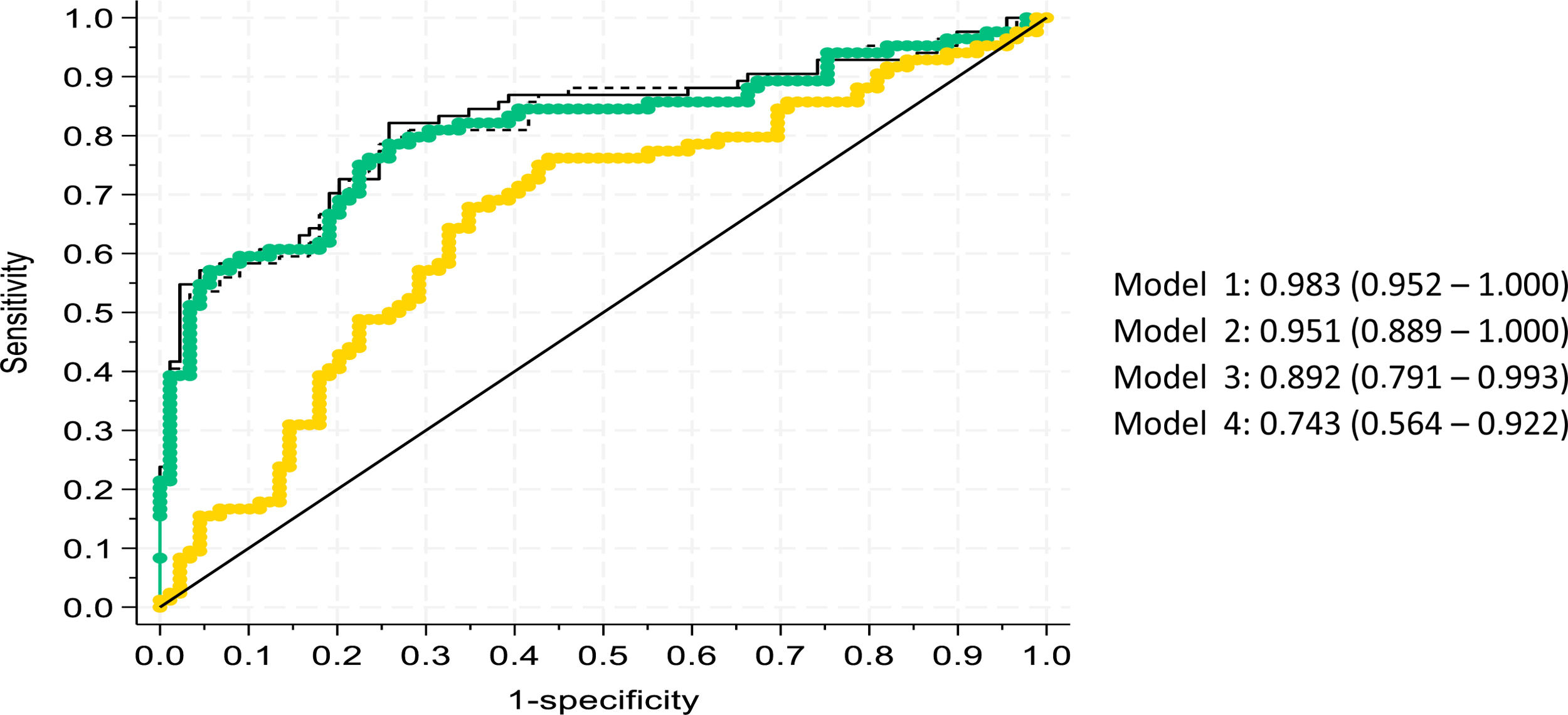
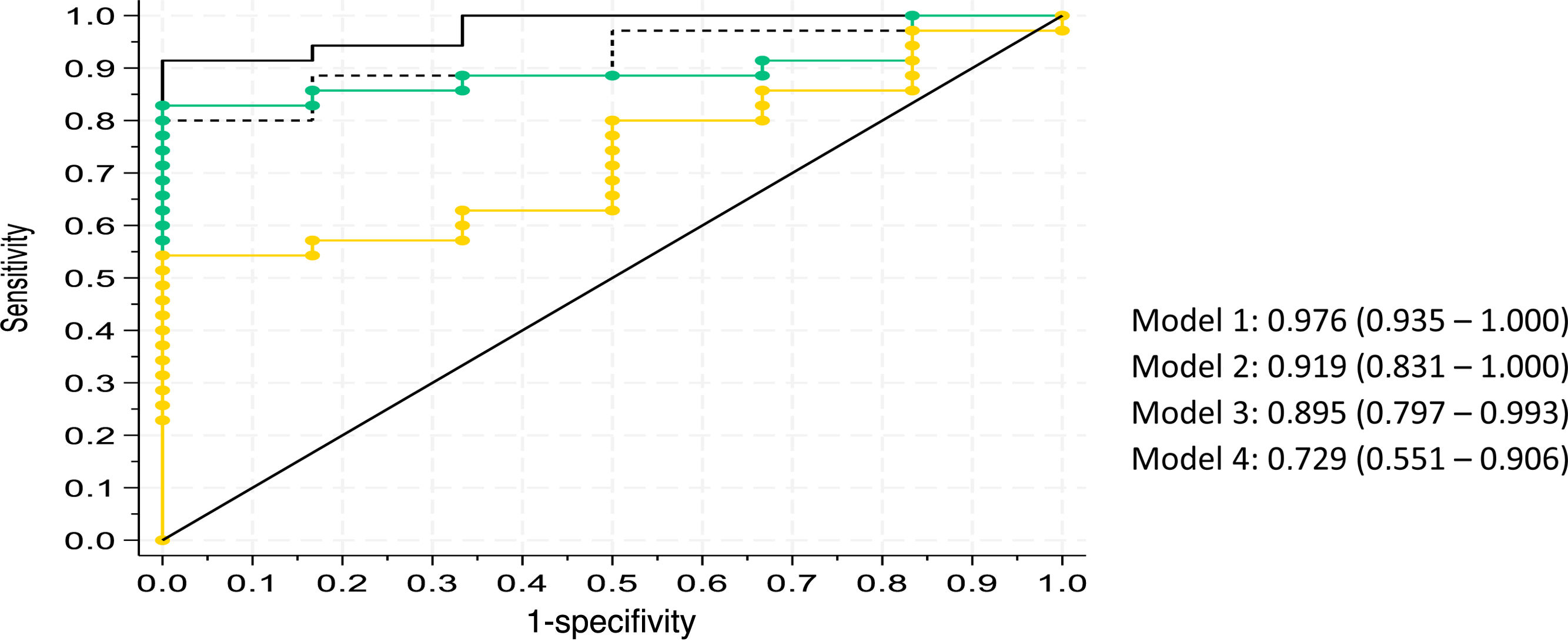
The process of constructing the predictive models involved a thorough selection of variables using logistic regression. Initially, models incorporating a single term were created, and additional variables were gradually added until a comprehensive model including all relevant terms was obtained. To assess model fit quality and complexity, Mallows’ Cp index and Akaike’s Information Criterion (AIC) were used. Models with the lowest values in both indices were selected, and results were presented using ROC curves. The 4 best-performing models were highlighted.
Model #1, considered the most comprehensive, included key variables such as patient functional status measured by the ECOG scale, tumor status, life expectancy estimated by the oncologist, tumor extent, age, smoking habits, and renal failure. The subsequent models (Models #2, #3, and #4) represented variations of the comprehensive model, each excluding 1 or more variables: Model #2 excluded the ECOG variable; Model #3 excluded both ECOG and tumor status; and Model #4 removed ECOG, tumor status, and life expectancy estimation.
Results showed that, in both ICU-admitted (Fig. 1) and non-admitted patients (Fig. 2), Model #1 had the best predictive capacity, with an area under the curve (AUC) of 0.983 (95%CI, 0.952–1.000) and 0.976 (95%CI, 0.935–1.000), respectively. This model, which incorporated all variables, including the ECOG score, proved to be the most robust in terms of predictive capability.
The APACHE II and SOFA scales are widely used at the ICU setting to predict mortality and patient severity. However, their predictive performance in this population varies. Azoulay et al. described that, in the hematologic population, the number of organ dysfunctions measured using the SOFA scale was significantly associated with mortality from day 1 onward.6 Later studies found no significant differences between scores on both scales and mortality at 3 and 6 months in patients with solid organ tumors.7
In fact, a recent study analyzing various prognostic models, including APACHE II, APACHE IV, SOFA, SAPS-II, SAPS-III, and MPM II, demonstrated that most tend to underestimate mortality in critically ill cancer patients.8 As previously mentioned, one limitation of these models is the lack of variables related to the patient’s functional status. Evidence suggests that critically ill cancer patients with greater frailty (defined as those with ECOG scores ≥) have a significantly higher mortality risk.9 Consequently, we believe that the models proposed in our study could serve as a foundation for future multicenter studies aimed at validating more specific mortality estimators for this population.
In conclusion, our findings underscore the importance of developing mortality predictive tools individualized to the specific characteristics of critically ill cancer patients. In particular, incorporating parameters related to patient functional status, such as the ECOG score, is of paramount importance.
CRediT authorship contribution statementElena Cuenca Fito: Conceptualization of the study, data collection, and manuscript drafting.
Inés Gómez-Acebo: Statistical and methodological support.
Alejandro González Castro: Manuscript drafting and review.
Declaration of Generative AI and AI-assisted technologies in the writing processNo artificial intelligence was used in the preparation of this manuscript.
FundingNone declared.