Noninvasive ventilation (NIV) constitutes first-line treatment for the exacerbation of obstructive pulmonary disease and cardiogenic lung edema. Several studies suggest that NIV failure could increase the risk of mortality, mainly due to the delay in tracheal intubation. We aimed to evaluate the negative impact of NIV failure in routine practice among Spanish ICUs.
PatientsA subanalysis was made of the multicenter validation of the Sabadell Score study, extracting patients with acute respiratory failure requiring either invasive or noninvasive mechanical ventilation, with the exclusion of patients presenting “do not resuscitate and/or do not intubate” orders.
VariablesWe recorded demographic parameters, ICU-specific treatments and the development of acute renal failure or infections during ICU stay. Patients were followed-up on until hospital discharge or death. The statistic analysis included Cox multiple logistic regression.
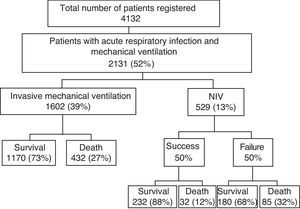
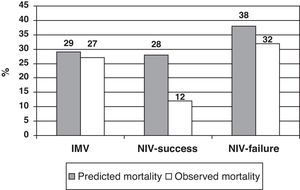
ResultsWe analyzed 4132 patients, of whom 1602 (39%) received only invasive mechanical ventilation (IMV), while 529 (13%) received NIV. The latter succeeded in 50% of the patients, but the other 50% required intubation. NIV failure was more common in neurological and postsurgical patients. Mortality was lower than predicted in NIV patients (22% vs 33%) and similar to predicted in IMV patients (27% vs 29%). Mortality was lower than predicted in patients in whom NIV proved successful (12% vs 28%), and in those in whom NIV failed (32% vs 38%).
ConclusionNIV failure and the need of intubation as routinely used do not seem to imply a poorer patient prognosis.
La ventilación no invasiva (VNI) constituye la primera línea de tratamiento en las exacerbaciones de la enfermedad pulmonar obstructiva crónica y el edema cardiogénico. Algunos estudios sugieren que el fracaso de la VNI incrementaría el riesgo de mortalidad, principalmente debido al retraso en la intubación. Pretendemos analizar si el fracaso de la VNI se asocia con un peor pronóstico en condiciones de práctica clínica diaria.
PacientesSubanálisis del estudio de validación multicéntrico Sabadell Score, analizando los pacientes con insuficiencia respiratoria aguda que requieren ventilación mecánica invasiva (VMI) o VNI, tras excluir los pacientes con limitación terapéutica.
VariablesEstudio de cohortes prospectivo. Recogimos datos demográficos, tratamientos específicos y complicaciones (fracaso renal agudo e infecciones adquiridas en UCI). Los pacientes se siguieron hasta el alta hospitalaria o muerte. El análisis estadístico incluyó regresión logística múltiple de Cox.
ResultadosAnalizamos 4.132 pacientes, de los cuales 1.602 (39%) recibieron solo VMI y 529 (13%) VNI. La VNI fue exitosa en el 50%, y el otro 50% requirió intubación, siendo más frecuente en pacientes neurológicos y postoperados. La mortalidad real fue similar a la predicha en los pacientes tratados solo con VMI (27% vs 29%, p=NS), pero inferior en los pacientes tratados con VNI (22% vs 33%, p<0.001), siendo muy inferior a la predicha en el grupo VNI-éxito (12% vs 28%, p<0.001), y solo ligeramente inferior en el grupo VNI-fracaso (32% vs 38%, p=NS).
ConclusionesEl fracaso de la VNI y la necesidad de intubación no parecen empeorar el pronóstico de los pacientes.
Noninvasive ventilation (NIV) is presently a routine procedure in the management of patients with acute respiratory failure (ARF) secondary to decompensated chronic obstructive pulmonary disease (COPD), hypoxia or decompensated congestive heart failure (CHF). Theoretically, NIV is safe and effective in correcting gas exchange and in reducing ventilatory muscle effort–thereby avoiding the need for invasive mechanical ventilation (IMV)1 and its consequences, such as ventilation associated pneumonia (VAP).
Many studies have demonstrated benefits of NIV in exacerbated COPD and decompensated CHF, as reflected by blood gas correction and a decrease in intubation, mechanical ventilation and mortality.1–3 In cases of hypoxemic ARF (pneumonia, adult respiratory distress syndrome, etc.), controversy remains regarding the indications, benefits and results of NIV. However, some studies recommend its utilization in view of the satisfactory results obtained in terms of patient prognosis and a decrease in intubation.1,4–6 Nevertheless, these studies are very heterogeneous in terms of the population groups and number of patients analyzed. This situation points to the need for broader studies in order to draw firm conclusions regarding the possible benefits of the technique, as underscored by the International Consensus Conference in Intensive Care Medicine.7
In general, studies on the application of NIV focus on determination of the components needed to ensure effective utilization of the technique (type of interface, ventilator programming, working equipment, etc.).1 In contrast, other studies, attempting to predict the results, center on the evaluation of factors capable of predicting success or failure of the technique (underlying disease, patient age, severity scales, PaO2/FiO2, PaCO2, etc.).6,8,9 Attempts to predict the effectiveness of NIV are based on the suspicion that a delay in intubation can worsen the patient prognosis in terms of mortality and/or stay in the Intensive Care Unit (ICU) and in hospital, as has been suggested by some studies.10
At present, and under true life clinical conditions outside the strict protocols of clinical trials, the prognosis of patients requiring NIV in Spanish ICUs is not clear. Based on the data obtained from the multicenter Sabadell Score validation study,11 we have attempted to determine whether failure in applying NIV would worsen the patient prognosis or not.
The primary study objective was to determine whether the success or failure of NIV (avoidance or failure to avoid intubation and IMV) modifies patient survival.
As a secondary objective, we examined whether the success or failure of NIV can be influenced by demographic or pharmacological factors, the development of infections in the ICU or acute renal failure (ARF), and whether it affects ICU and/or hospital stay.
Patients and methodsThe multicenter Sabadell Score validation study was carried out in 31 Spanish ICUs over a period of three months (March–May 2008). A total of 4132 patients were analyzed (Fig. 1). On the basis of the original study–the primary objective of which was to validate the Sabadell Score as a predictor of the prognosis of patients discharged from the ICU–in our subanalysis we used the existing data to assess the effect of the routine use of NIV in daily clinical practice in Spanish hospitals. We selected the patients presenting criteria of acute respiratory failure of any origin, and with a need for mechanical ventilation, whether invasive or otherwise. We excluded all cases involving a limitation of therapeutic effort or with a defined “therapeutic ceiling”. Different variables were analyzed: patient age, reason for admission, specific ICU treatments (vasoactive drugs, parenteral nutrition, dialysis, and/or tracheostomy), stay in the ICU, and hospital stay. As morbidity parameters we recorded the appearance of acute renal failure and the development of nosocomial infection (respiratory infection, ventilator associated pneumonia (VAP), urinary infection and/or catheter-related bacteremia). Due to the population based approach of the study, with adoption of the “standard treatment” concept, no consensus was established regarding the different diagnoses or definitions–the decisions referred to diagnostic techniques and treatments (weaning, dialysis, etc.) being left to the criterion of the participating physician. As outcome variables we included readmission to the ICU, mortality in the ICU, and hospital mortality. The hospital mortality data recorded in each of the groups (IMV, NIV-success and NIV-failure) were compared with mortality predicted by the severity scale used in the different participating centers (APACHE II, SAPS 2 and SAPS 3 scores).
Statistical analysisQualitative variables, expressed as percentages, were compared using the chi-squared test or the Fisher exact test in the case of very small samples. Quantitative variables in turn were expressed as the mean and standard deviation in the presence of a normal distribution, and as the median and interquartile range in the case of a non-uniform distribution or a sample size (n) of less than 20. These variables were compared with the Student t-test for unpaired data, accepting a significance level of p<0.05. On the other hand, we analyzed the Kaplan–Meier survival distribution for each of the groups (IMV, NIV-failure and NIV-success). Cox multiple logistic regression analysis was used for those variables that might influence patient prognosis (predicted mortality, acute renal failure, use of vasoactive drugs, nosocomial infection). The Epiinfo v.3.5.1 package was used for the statistical analysis (CDC, Atlanta, GA, USA).
ResultsOf the 4132 patients registered, 2131 (52%) presented acute respiratory failure and required some type of ventilatory support (Fig. 1). Invasive mechanical ventilation was used from the start in 1602 patients (75%), and NIV in 529 (25%). Among these cases, failure was recorded in 50% and IMV thus proved necessary, while the remaining 50% evolved adequately.
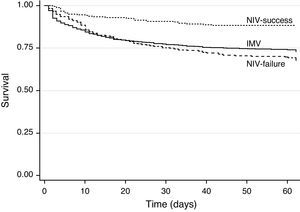
The comparison of IMV and NIV showed the patient age to be younger (61±16 years vs 63±15 years, p=0.001) and the use of vasoactive drugs greater (63% vs 57%, p<0.01) in the IMV group (Table 1). However, there were no differences in terms of patient gender (males 67% vs 65%, p=NS), the stay in the ICU (10±13 days vs 11±11 days, p=NS), or in the duration of hospital stay after leaving the ICU (14±20 days vs 15±19 days, p=NS). Likewise, there were no differences between the IMV and NIV groups in terms of the development of acute renal failure, infection acquired in the ICU, or readmission to the ICU. In patients with IMV, the observed mortality was similar to the predicted mortality, while in the NIV group the observed mortality was clearly lower than the predicted mortality (Fig. 2).
Characteristics of the patients compared according to the ventilatory mode used.
| IMV n: 1602 | NIV n: 529 | p | |
| Age, years | 61±16 | 63±15 | 0.001 |
| Male gender, n (%) | 1073 (67%) | 345 (65%) | NS |
| Vasoactive drugs, n (%) | 1008 (63%) | 304 (57%) | 0.01 |
| Infection in ICU, n (%) | 298 (18%) | 97 (18%) | NS |
| Acute renal failure, n (%) | 425 (26%) | 149 (28%) | NS |
| Readmission to ICU, n (%) | 78 (5%) | 28 (6%) | NS |
| Stay in ICU, days | 10±13 | 11±11 | NS |
| Post-ICU hospital stay, days | 14±20 | 15±19 | NS |
| Predicted mortality (%) | 29% | 33% | 0.001 |
| Observed mortality (%) | 27% | 22% | 0.02 |
The analysis of the NIV group according to the success or failure of the technique is shown in Table 2. There were no differences in either age or gender distribution. However, differences were noted both in the use of vasoactive drugs (74% vs 40%, respectively, p<0.001) and in infections acquired in the ICU (33% vs 4%, p<0.001), as well as in acute renal failure (35% vs 21%, p<0.001) and stay in the ICU (16±14% vs 6±5 days, p<0.001). In contrast, neither post-ICU hospital stay (14±17 vs 16±21, p=NS) nor readmission to the ICU (6% vs 6%, p=NS) showed differences. The observed mortality was always lower than the predicted mortality in both groups; in the NIV-success group, the observed mortality was 12% and the predicted mortality was 28% (standardized mortality ratio (SMR) 0.43), while in the NIV-failure group the observed mortality was slightly lower than the predicted mortality (32% vs 38%, SMR 0.84) (Fig. 2).
Characteristics of the patients with NIV compared according to success or failure of the technique.
| NIV-success n: 266 | NIV-failure n: 263 | p | |
| Age, years | 64±15 | 63±15 | NS |
| Male gender, n (%) | 182 (68%) | 163 (62%) | NS |
| Vasoactive drugs, n (%) | 40 (15%) | 74 (28%) | 0.001 |
| Infection in ICU, n (%) | 10 (4%) | 87 (33%) | 0.001 |
| Acute renal failure, n (%) | 56 (21%) | 93 (35%) | 0.001 |
| Readmission to ICU, n (%) | 14 (6%) | 14 (6%) | NS |
| Stay in ICU, days | 6±5 | 16±14 | 0.001 |
| Post-ICU hospital stay, days | 14±17 | 16±21 | NS |
| Predicted mortality (%) | 28% | 38% | 0.001 |
| Observed mortality (%) | 12% | 32% | 0.001 |
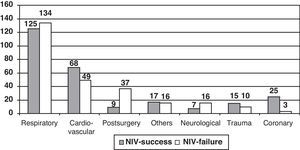
The distribution of patients with NIV according to the reason for admission (Fig. 3) was found to be similar for both success and failure in the case of respiratory diseases and traumatisms. However, in the patients with coronary and non-coronary cardiovascular disease, NIV was seen to be more successful–in contrast to the situation seen in postsurgical and neurological patients.
The Kaplan–Meier survival analysis between groups (IMV, NIV-failure and NIV-success) yielded significant differences (log-rank 28.7, p<0.001, Fig. 4). Survival was clearly greater in the NIV-success group (88%), with no differences between the IMV and NIV-failure groups (73% vs 68%, p=NS).
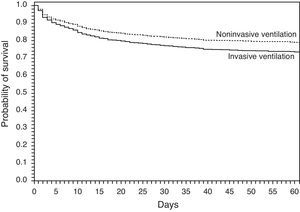
The Cox logistic regression analysis of these variables is shown in Table 3 and Fig. 5. The need for vasoactive drugs (odds ratio (OR) 3.1), the development of infections in the ICU (OR 1.4), acute renal failure (OR 2) and predicted mortality (OR 1.035) were associated to poorer survival. Lastly, the utilization of NIV was associated to a protective effect (OR 0.6).
The routine clinical use of NIV in patients with acute respiratory failure, analyzed during a period of three months in 31 Spanish hospitals, revealed a decrease in mortality with respect to the expected mortality as estimated from the severity scales. When NIV proved successful, mortality was far lower than expected, and it should be underscored that when NIV failed to avoid the need for intubation, the observed mortality remained lower than expected. These data support NIV as a safe option, with potential benefits in terms of the avoidance of intubation and ventilator associated pneumonia, and especially regarding the fact that the delay in intubation resulting from the use of NIV does not in itself imply an increased risk of mortality.
A significant observation was the fact that patient stay both in the ICU and subsequently in hospital proved similar regardless of the type of ventilation used (NIV or IMV). When NIV proved effective, the stay in the ICU was shorter than in cases of failure–though hospital stay remained similar (Table 2). The randomized, prospective study carried out by Conti et al.2 yielded results very similar to our own, both as regards improvement in patient survival with NIV and as refers to hospital stay. Our study, involving a 10-fold greater number of patients, would offer more reliable evidence of the effectiveness of the technique–while also demonstrating its effectiveness in the context of routine clinical practice. A study of NIV in 123 Spanish centers, conducted in 2005 with objectives very different from those of our study, investigated the proportion of NIV used according to the different disease processes involved.12 Of the 232 patients subjected to NIV, 76% evolved adequately on the basis of a series of prior inclusion criteria–excluding postsurgical and neurological cases and patients with prior metabolic disturbances, etc. In comparison, our series comprised all subjects requiring NIV, independently of the underlying pathology or origin; as a result, the results are not fully comparable in this sense. Nevertheless, the findings of both studies coincide in that no differences were observed on comparing patients intubated after NIV failure versus those intubated from the start, in terms of mortality in the ICU (47% vs 38%, p=0.2) or in hospital (55% vs 43%, p=0.1), or in terms of the development of pneumonia (16% vs 18%, p=0.7).
When NIV proved successful, our data referred to the development of intra-ICU infections or acute renal failure were also positive. The development of acute renal failure and infections in the ICU was more limited in the NIV-success group, and proved significantly greater in the NIV-failure group. Renal failure could play an additional role in the failure of NIV, while in the case of the infections, the development of ventilator associated pneumonia would play a role, following intubation. The logistic regression analysis showed these to be independent factors multiplying mortality risk.
The analysis of the patients by disease subgroups proved consistent with the findings of earlier studies. The multicenter study published by Antonelli et al.8 involving NIV in 354 patients with hypoxemic acute respiratory failure, recorded a global failure rate of 30%. The frequency of NIV failure in acute respiratory distress syndrome (ARDS) and in pneumonia was 50%, while in decompensated CHF and in pulmonary contusion the failure rate was found to be very low (10% and 18%, respectively). In this same line, Demoule et al., in a multicenter study in French ICUs, compared the utilization of NIV in two periods in 1997 and 2002.13 The NIV failure rate was close to 45% for a heterogeneous group of patients–a high SAPS score and hypoxemic ARF being the factors most closely associated to NIV failure. In 2001, Lasdica et al.14 analyzed the effect of NIV in hypoxemic patients involving different etiologies (pneumonias, pancreatitis, postsurgical patients, sepsis, etc.), after excluding those with COPD. The authors evaluated 27 patients; of these, failure occurred in 25%, with a need for intubation. All the patients in which NIV avoided the need for intubation survived–in contrast to the failure group, where a fatal outcome was recorded in all cases. Despite the small size of this series, NIV was found to be of benefit in the hypoxemic patients, with improvement of the hemodynamic and gas exchange parameters. Here again our own findings support the above data and would indicate that the results obtained with NIV in routine clinical practice are equivalent to those obtained in methodologically very controlled and selected study series. The important severity of the patients in which NIV was proposed appears to confirm that physicians continue to limit this ventilatory support modality to truly critical patients, where the effectiveness of the technique has been more clearly demonstrated. In the review published by Keenan et al.6 referred to NIV in hypoxemic patients, a proportionally greater effect was observed in more serious patient conditions. In contrast, a possible deleterious effect of the technique was suggested in patients with a very low risk of death.
The meta-analysis conducted by Agarwal et al.15 evaluated 13 studies comprising 540 patients, comparing the efficacy of NIV in patients with ALI/ARDS. The percentage of patients with NIV who ultimately required intubation was 48%–the patient series being quite heterogeneous, with hypoxemia of pulmonary and extrapulmonary origin, and involving different pathological conditions. In our study, on examining the group of patients presenting respiratory causes (Fig. 3), the NIV failure rate was likewise in the order of 51%–though it must be noted that in our case we made no distinction between patients with hypoxemic and/or hypercapnic etiologies.
NIV in postsurgery patients is also subject to controversy. Chiumello et al.16 in an analysis of 29 studies, found both prophylactic and therapeutic NIV to improve the blood gas parameters in only 19 studies, while in only 11 did it lead to a decreased need for intubation. Our study recorded increased failure of NIV, though the number of patients is too limited to allow the drawing of conclusions.
Study limitationsThe present study is a subanalysis of a previous prospective study; accordingly, analysis of the efficacy of NIV was not the primary objective of the initial data.
No separation was made in patients with respiratory failure between acute hypoxemic disease and exacerbated COPD; as a result, we are unable to describe how each respiratory condition responded separately to NIV. Likewise, since an observational design was involved, the original study did not protocolize data collection with respect to factors associated to the prognosis of patients subjected to NIV (age, PaO2/FiO2, blood gases, timing of intubation, etc.). On the other hand, since our patients comprised one-half of the total patients, their behavior exerted a greater impact upon the global study series; we therefore described each disease group separately.
The inclusion criteria, the timing of orotracheal intubation or the application of NIV, the selection of the NIV or IMV arm, the type of interface used or the ventilation modality employed were not protocolized; rather, data were collected in the context of routine clinical practice. Nevertheless, the results of previous protocolized studies coincide with those of our own study.
Different severity scales were used by the different participating centers for predicting mortality and comparing it with the observed mortality. This may be regarded as a limitation, though the original study11 compared the three severity scales (APACHE II, SAPS 2 and SAPS 3) without observing differences in the estimation of global patient prognosis. It is important to underscore that this study did not aim to determine which values of the different severity scales define a poorer prognosis or risk of NIV failure; rather, the objective was to estimate expected mortality. In our study the values referred to observed and predicted mortality in mechanical ventilation were similar, while observed mortality proved lower in the case of NIV–a circumstance which could be related to the protective effect associated with the noninvasive technique.
We conclude that the use of NIV in routine clinical practice improves the survival of patients in the ICU, and that even in the case of NIV failure requiring patient intubation, the mortality rate remains lower than expected. When NIV proves successful, the complications and days of stay in the ICU are moreover reduced.
The present study was not supported by any type of grant of financial aid. Likewise, there are no conflicts of interest on the part of the authors.
Conflicts of interestThe authors declare that they have no conflicts of interest.
José Felipe Solsona (H. del Mar. Barcelona), Fernando Frutos (H. U. de Getafe. Madrid), Frutos del Nogal (H. Severo Ochoa. Leganés), Gonzalo Hernández (H. Infanta Sofía. Madrid), Javier González (H. Clínico U. de Salamanca), José Manuel Añon (H. Virgen de la Luz. Cuenca), José Manuel Serrano (H. Reina Sofía. Córdoba), Lluis Cabre (SCIAS H. de Barcelona), M Isabel Umaran (H. de Cruces. Baracaldo), M. Victoria De la Torre (H. U. Virgen de la Victoria. Málaga), M. Jesús López-Pueyo (H. General Yagüe. Burgos), M. José Gutiérrez (H. San Agustín. Aviles), Manuela García (H. Virgen Macarena. Sevilla), María Jesús Gómez (H. Reina Sofía. Murcia), Pablo Monedero (Clínica U. de Navarra. Pamplona), Paula Vera (H. Sant Joan. Reus), Pedro Ibáñez (H. Son Llatzer. Mallorca), Pedro Rascado (H. Juan Canalejo. La Coruña), Ramón Fernández-Cid (H. Mateu Orfila. Menorca), Rosa Catalán (Consorci H. de Vic), Susana Altaba (H. G. de Castellón), Vicente Gómez-Tello (H. Moncloa. Madrid), Victoria Lacueva (H. de Sagunto. Valencia).
Please cite this article as: Delgado M, et al. Impacto del fracaso de la ventilacion no invasiva en el pronóstico de los pacientes. Subanálisis de un estudio multicéntrico. Med Intensiva. 2012;36:604–10.