The impact of left ventricular (LV) systolic dysfunction on weaning failure is unclear.
DesignUpdated meta-analysis assessing the association between LV ejection fraction (LVEF) and weaning failure.
SettingA systematic search of MEDLINE and EMBASE for prospective studies reporting weaning according to echocardiographic data measured before starting a spontaneous breathing trial (SBT).
Patients or participantsStudies included in the meta-analysis that reported on weaning and echocardiographic data.
Main variables of interestLVEF, E/e’ ratio, E velocity, deceleration time of the E wave, and e’ velocity.
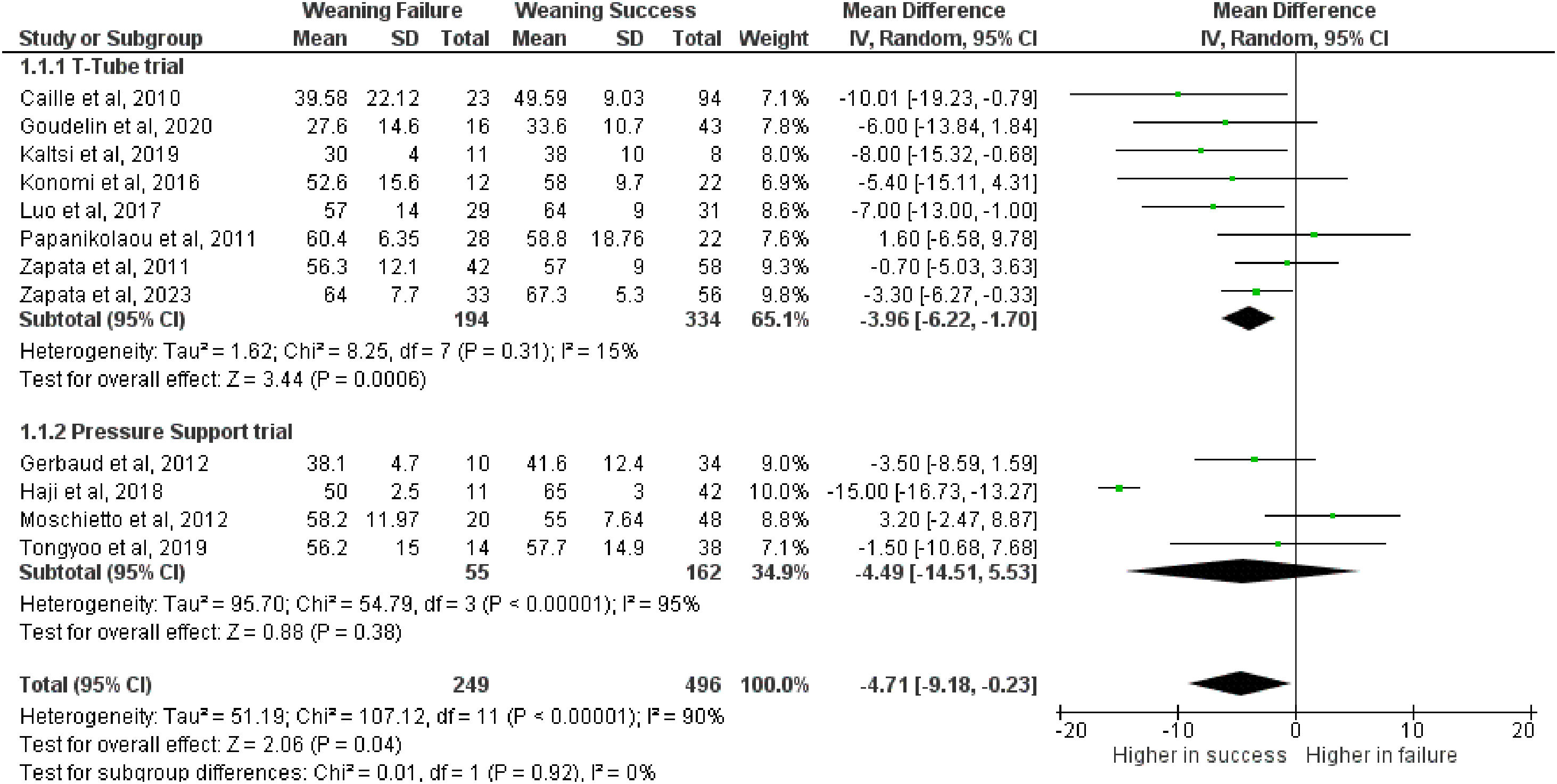
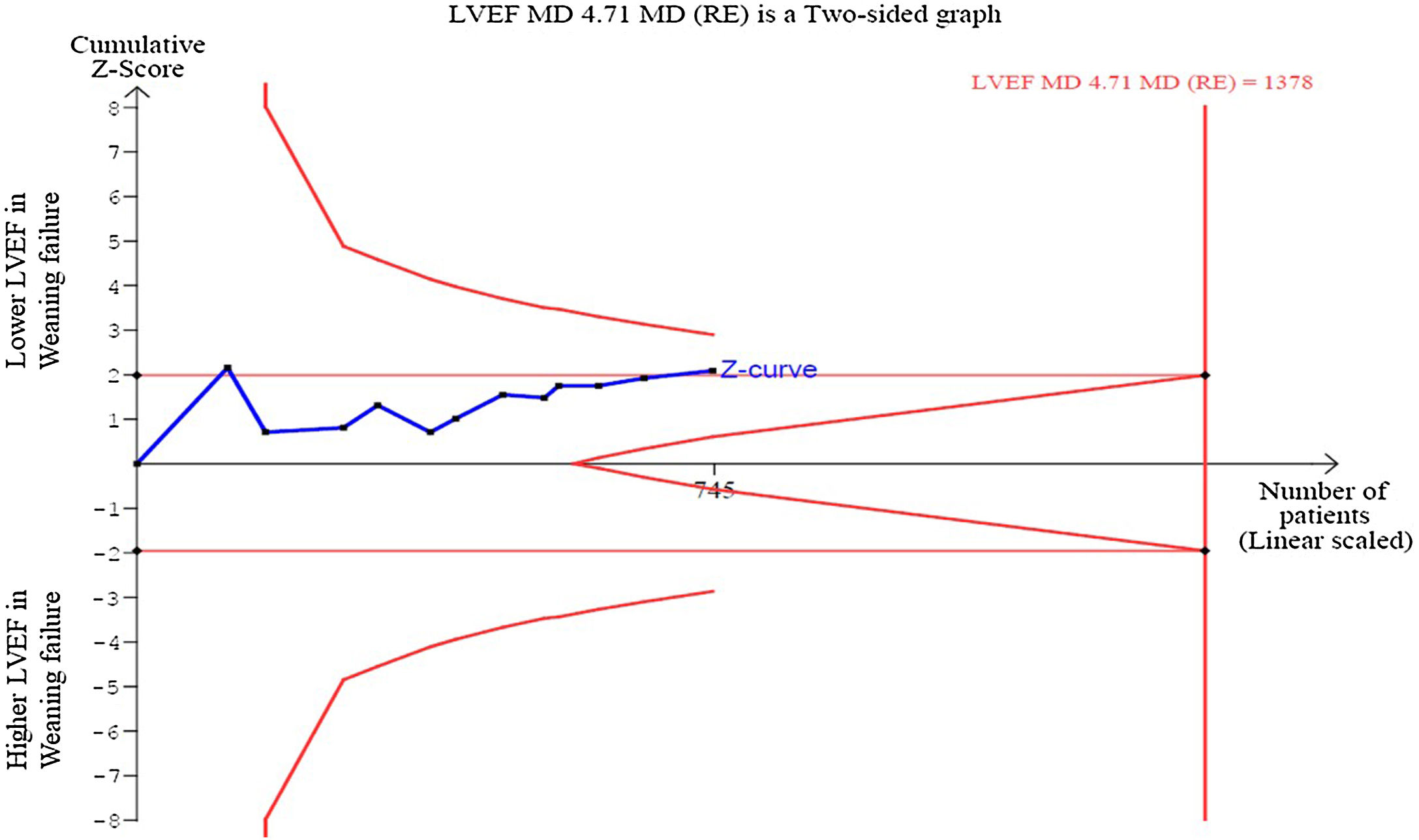
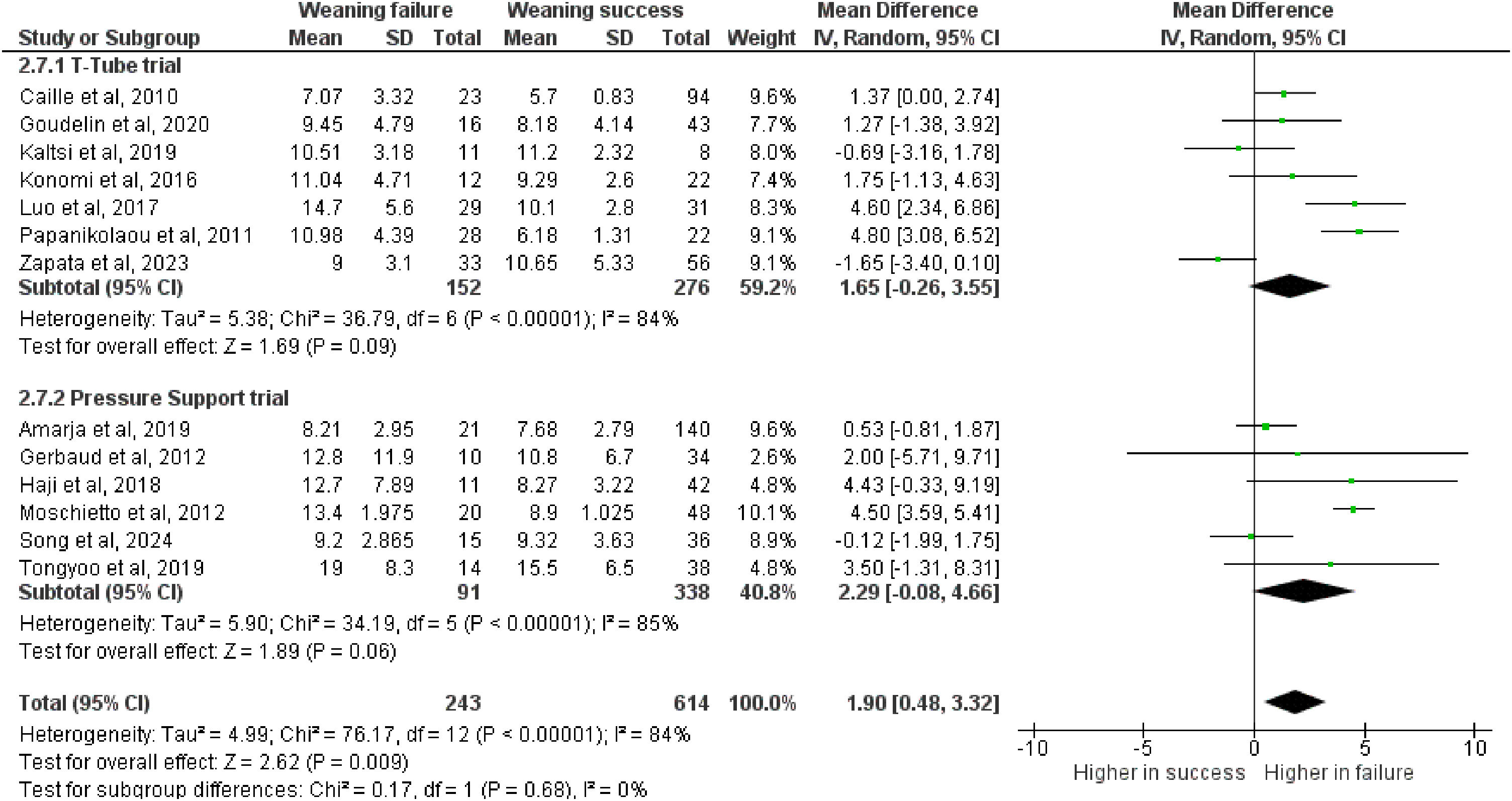
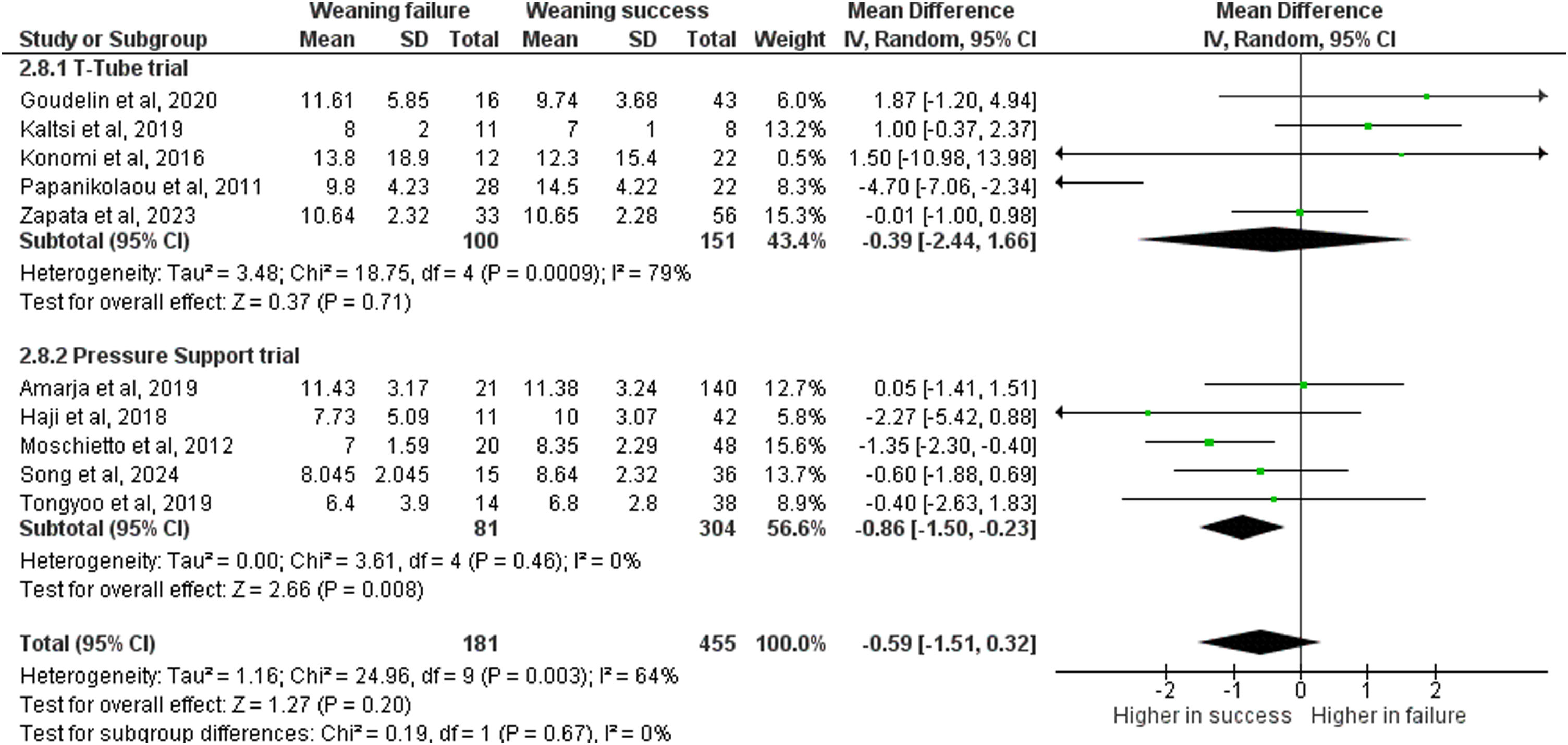
ResultsThree studies were added in this update (n = 14, sample 20–30% larger). Lower LVEF (n = 12) was associated with weaning failure: MD: −4.71 95%CI [−9.18, −0.23]; p = 0.04, I2 = 90%, low certainty of evidence), without subgroups difference according to SBT type or LVEF mean values. Trial sequential analysis showed that results were not robust (information size n = 745/1378). E/e’ ratio (MD: 1.90, 95%CI [0.48,3.32]; p = 0.009, I2 = 84%), E velocity (MD: 8.32, 95%CI [2.59,14.05]; p = 0.004, I2 = 54%) and shorter deceleration time of the E wave (MD: −12.01, 95%CI [−21.13, −2.89]; p = 0.01, I2 = 0%) were associated with weaning failure, whilst e’ velocity was not (MD: -0.59, 95%CI [−1.51,0.32]; p = 0.20, I2 = 64%).
ConclusionsAn association of weaning failure with poorer LV systolic function (LVEF), not detected by the previous meta-analysis, was found. However, such association is highly fragile and with a mean difference below 5%, which seems not clinically relevant. Higher E/e’ ratio and other diastolic parameters confirmed their association with weaning failure, whilst e’ did not.
El impacto de la disfunción sistólica del ventrículo izquierdo (VI) en el fracaso en el weaning de la ventilación mecánica en el paciente crítico no está claro.
DiseñoMetanálisis actualizado que evalúa la asociación entre la fracción de eyección del ventrículo izquierdo (FEVI) y el fracaso del destete.
ÁmbitoBúsqueda sistemática en MEDLINE y EMBASE de estudios prospectivos que reportaran el destete según datos ecocardiográficos medidos antes de iniciar una prueba de respiración espontánea (PRE).
Pacientes o participantesEstudios incluidos en el metanálisis que informaron sobre el destete y los datos ecocardiográficos.
Variables de interés principalesFEVI, relación E/e’, velocidad de la onda E, tiempo de desaceleración de la onda E y velocidad e’.
ResultadosSe añadieron tres estudios en esta actualización (n = 14, muestra un 20-30% mayor). Una menor FEVI (n = 12) se asoció con el fracaso del destete: MD: -4,71 IC95%[-9,18,-0,23]; p = 0,04, I² = 90%, con baja certeza de la evidencia), sin diferencias entre subgrupos según el tipo de PRE o los valores medios de FEVI. El análisis secuencial de ensayos mostró que los resultados no eran robustos (tamaño de información n = 745/1378). La relación E/e’ (MD: 1,90, IC95% [0,48,3,32]; p = 0,009, I² = 84%), la velocidad de la onda E (MD: 8,32, IC95% [2,59,14,05]; p = 0,004, I² = 54%) y un menor tiempo de desaceleración de la onda E (MD: -12,01, IC95% [-21,13,-2,89]; p = 0,01, I² = 0%) se asociaron con el fracaso del destete, mientras que la velocidad e’ no lo hizo (MD: -0,59, IC95% [-1,51,0,32]; p = 0,20, I² = 64%).
ConclusionesEncontramos una asociación entre el fracaso del destete y una peor función sistólica del VI (FEVI), no detectada en el metanálisis previo. Sin embargo, dicha asociación es altamente frágil y con una diferencia media inferior al 5%, lo que parece no ser clínicamente relevante. La relación E/e’ y otros parámetros diastólicos confirmaron su asociación con el fracaso del destete, mientras que la velocidad e’ no lo hizo.
Weaning from mechanical ventilation (MV) is a complex step during the recovery from critical illness, and defined as either the failure of spontaneous breathing trial (SBT) or, in the case of extubation, the need for reintubation, the institution of non invasive ventilation (NIV) or the occurrence of death during the first 48 h after extubation.1 Weaning failure is associated with significant mortality and morbidity in patients admitted to intensive care unit (ICU),1–4 and with substantial financial and economic burden.1,5 When evaluating the readiness for extubation, clinicians integrates several parameters; among others, patient age and comorbidities, indices of respiratory support and gas exchange, laboratory findings, and echocardiographic parameters seems significant predictors.6–11
The most common mechanisms of weaning failure are identified in the heart and lung interaction,12 even if more evidence is available on the contribution of diaphragmatic dysfunction,13 though it also may be worth checking for extra-diaphragmatic respiratory muscle activation/athropy and for abdominal causes of failure (i.e. ascites).14 Nonetheless, in the largest study on the topic, weaning-induced pulmonary edema, accounted for almost 60% of failures; in this cohort, chronic obstructive pulmonary disease, previous “structural” cardiopathy and obesity were independent risk factors.
Echocardiography provides a real-time assessment of cardiac dysfunction. Its use is continuously expanding in the ICU, and it can be a valuable assessment tool during the process of weaning.16,17 A previous metanalysis18 showed that parameters referring to the left ventricular (LV) diastolic dysfunction (DD) were associated with a greater risk of weaning failure. Conversely, the contribution of systolic dysfunction evaluated by LV ejection fraction (LVEF) was more unclear (standardized mean difference, SMD: −0.86 [−1.92;0.20]; p = 0.11, high heterogeneity). Such results were possibly influenced by the sample size. Considering the uncertainty of evidence, we conducted an updated systematic review and meta-analysis to re-evaluate the association between LV systolic dysfunction and the risk of failing the weaning from MV.
MethodsOur systematic review and meta-analysis was registered in PROSPERO, the international prospective register of systematic reviews (CRD42019117832). We regularly recorded the decision to proceed with an update. The metanalysis is reported in accordance with the PRISMA guidelines.19
Eligibility criteriaThe inclusion criteria in this metanalysis have been reported. We included prospective observational studies reporting echocardiographic data that were recorded before attempting weaning from MV with a spontaneous breathing trial (SBT) in view of extubation. Data were divided into two groups of patients, according to the success or failure of weaning. As per the WIND study, weaning failure was considered as: 1) failure of SBT or, 2) in case of patients that were extubated, the need for reintubation, the institution of NIV or the occurrence of death during the first 48 h after extubation.1 The inclusion criteria according to the PICOS framework are provided as Supplementary material (Appendix B). Paediatric studies were excluded. Case series were considered only if at least 10 patients were studied.
Regarding the approach for SBT, we included studies conducted using either a T-tube trial or low level of pressure support ventilation (PSV), the latter defined as the inspiratory support ≤10 cmH2O with a positive end-expiratory pressure (PEEP) ≤5 cmH2O.
Identification of studiesThe updated literature search covered the period from the 4th of December 2019 (the last update of the previous metanalysis) to the 31st December of 2024, with the same search strategy as previously adopted (Supplementary material (Appendix B)) in MEDLINE/PubMed and EMBASE database. Search on EMBASE allowed also to retrieve conference abstracts of studies not published yet. Further independent manual searches were conducted by four authors, and language restrictions were applied (only articles in English were considered).
Analysis of outcomesFor the present update, we primarily focused on the LVEF as the main parameter describing LV systolic dysfunction. Subgroup analyses were performed according to the approach of SBT (conducted in T-Tube or PSV) as in the previous analysis. We also conducted a subgroup analysis separating the studies into two groups according to the mean overall LVEF.
We secondarily evaluated parameters describing LVDD and right ventricular (RV) function. Regarding the Tissue Doppler Imaging (TDI) variables, sub-group analyses were performed using regional criteria of sampling (dividing data in average, lateral or septal values).
Study selection and data extractionThree investigators independently screened findings produced by the search and identified the articles of potential interest. Full text articles of potential interest were downloaded and assessed against the inclusion criteria. Discrepancies were resolved by consensus and/or by involving other two senior authors. Two reviewers independently extracted data from individual studies and entered information into the collection form previously used; a cross-check was performed by three authors.
Quality assessment and certainty of evidenceThe methodological quality of the design in the included studies was performed by four authors using the Newcastle-Ottawa scale (NOS)20 with its three domains (selection, comparability and outcome) and classified as high-risk (1–3 points), intermediate-risk (4–5 points) or low-risk of bias (6–9 points). The grade of evidence was assessed by three authors according to the recommendations of the Grading of Recommendations Assessment, Development, and Evaluation working group using the GRADEpro software.21
Sensitivity analysesAs in the original metanalysis, four types of sensitivity analyses were preventively planned: the first conducted including also studies with criteria for reintubation extended to a longer timeframe; the second with studies of non-prospective methodology; the third excluding studies at high risk of bias, and the last one performed with “leave-one-out at time” approach.
Statistical analysisThe mean and the standard deviation (SD) of each echocardiography variable were collected and in case of data available as median and interquartile range, we followed recommendations to approximate values of mean and SD.22,23 Continuous variables were analysed with the inverse variance (IV) model and a 95% Confidence Interval (95%CI). Differently from previous metanalysis, we decided to report analysis with a mean difference (MD) to gather the clinical difference of the variables between weaning failure and success. The p values were evaluated as two-tailed and statistical significance was set at <0.05. Statistical heterogeneity was assessed with the X2 (Cochran Q) test. Heterogeneity was confirmed if p was ≤0.10 and its quantification performed with I2 statistic (ranges of 0–24.9%, 25–49.9%, 50–74.9% and >75% considered as none, low, moderate and high heterogeneity, respectively).24 The conservative random-effect model was used. Meta-analysis was conducted using a review manager (Revman, Version 5.3. Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration, 2014).
A trial sequential analysis (TSA) was conducted to evaluate the robustness of the outcomes using the freely available TSA Software (Copenhagen Trial Unit’s TSA Software; Copenhagen, Denmark). The estimated effect was computed using the MD obtained in the forest plot, computing information size and adjusted boundaries with an alpha risk of 5% and a power of 80% (beta risk of 20%). Details on TSA and its interpretation are available elsewhere.25
Continuous variables were analysed with the inverse variance (IV) model and a 95% Confidence Interval (95%CI). Differently from previous metanalysis, we decided to report analysis with mean difference (MD) to gather the cinical difference of the variables between weaning failure and success. The p values were evaluated as two-tailed and statistical significance was set at <0.05. Statistical heterogeneity was assessed with the X2 (Cochran Q) test. Heterogeneity was confirmed if p was ≤0.10 and itsquantification performed with I2 statistic (Ranges of 0–24.9%, 25–49.9%, 50–74.9% and >75% considered as none, low, moderate and high heterogeneity, respectively).24 The conservative random-effect model was used. Publication bias was investigated inspecting the funnel plot. Meta-analysis was conducted using review manager (Revman, Version 5.3. Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration, 2014). A trial sequential analysis (TSA) was conducted to evaluate robustness of the outcomes using the freely-available TSA Software (Copenhagen Trial Unit’s TSA Software; Copenhagen, Denmark). Estimated effect was computed using the MD obtained in the forest plot, computing information size and adjusted boundaries with an alpha risk of 5% and a power of 80% (beta risk of 20%). Details on TSA and its interpretation are available elsewhere.25
ResultsThe update literature search identified a further 1810 titles between MEDLINE/PubMed and EMBASE. A modified PRISMA flowchart and the PRISMA checklist are reported as Supplementary material (Appendix B). After removing articles deemed not pertinent, 12 full-text were assessed, with eight excluded as not reporting data and one as the approach for SBT was not reported. Hence, in the present metanalysis we pooled together the previously included eleven studies26–36 with the addition of data from three new findings.37–39 Of note, regarding the study by Goudelin et al., we gathered the echocardiography data from a letter that the authors subsequently published.40 The previous metanalysis could not include a study from Lamia et al. as the authors did not explicitly report echocardiographic findings according to weaning failure or success, and it was not possible to retrieve such data of interest.41
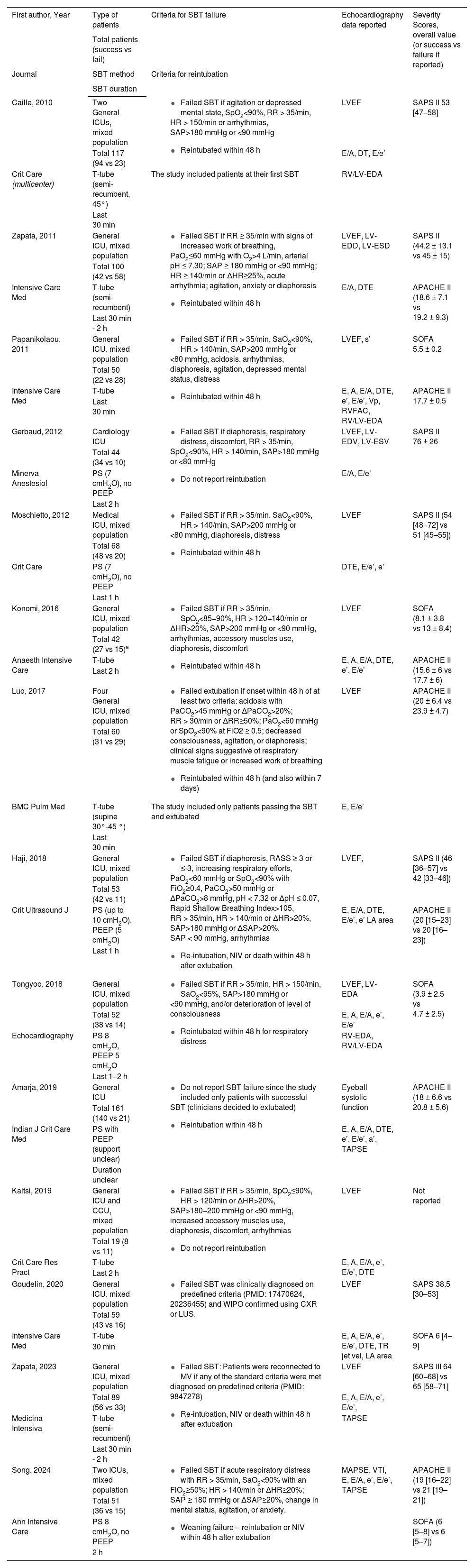
All studies assessed heart function with transthoracic echocardiography, and as shown in Table 1, data extracted from each study included: setting of critically ill patients enrolled, number of patients examined, mode of SBT and criteria for SBT failure, echocardiography parameters evaluated and severity scores. The most commonly reported echocardiographic parameter was the E/e’ ratio (n = 13), followed by LVEF and E/A ratio (n = 12 for both), E wave (n = 11) and TDI e’ wave (n = 10). Regarding the LV diastolic function, only two studies reported measure of left atrial area,36,37 and two reported tricuspid regurgitant jet velocity.37,38 In the previous metanalysis,18 we found not enough data to analyse the impact of RV dysfunction in the setting of weaning from MV. In this update metanalysis, we pooled data from three studies reporting the tricuspid annular plane systolic excursion (TAPSE),30,38,39 but not other data on RV function were ameanable of meaningful analysis.
Summary of characteristics of included studies. Results are indicated as mean ± standard deviation or as median, interquartile range.
| First author, Year | Type of patients | Criteria for SBT failure | Echocardiography data reported | Severity Scores, overall value (or success vs failure if reported) |
|---|---|---|---|---|
| Total patients (success vs fail) | ||||
| Journal | SBT method | Criteria for reintubation | ||
| SBT duration | ||||
| Caille, 2010 | Two General ICUs, mixed population |
| LVEF | SAPS II 53 [47–58] |
| Total 117 (94 vs 23) | E/A, DT, E/e’ | |||
| Crit Care (multicenter) | T-tube (semi-recumbent, 45°) | The study included patients at their first SBT | RV/LV-EDA | |
| Last 30 min | ||||
| Zapata, 2011 | General ICU, mixed population |
| LVEF, LV-EDD, LV-ESD | SAPS II (44.2 ± 13.1 vs 45 ± 15) |
| Total 100 (42 vs 58) | ||||
| Intensive Care Med | T-tube (semi-recumbent) | E/A, DTE | APACHE II (18.6 ± 7.1 vs 19.2 ± 9.3) | |
| Last 30 min - 2 h | ||||
| Papanikolaou, 2011 | General ICU, mixed population |
| LVEF, s’ | SOFA 5.5 ± 0.2 |
| Total 50 (22 vs 28) | ||||
| Intensive Care Med | T-tube | E, A, E/A, DTE, e’, E/e’, Vp, RVFAC, RV/LV-EDA | APACHE II 17.7 ± 0.5 | |
| Last 30 min | ||||
| Gerbaud, 2012 | Cardiology ICU |
| LVEF, LV-EDV, LV-ESV | SAPS II 76 ± 26 |
| Total 44 (34 vs 10) | ||||
| Minerva Anestesiol | PS (7 cmH2O), no PEEP | E/A, E/e’ | ||
| Last 2 h | ||||
| Moschietto, 2012 | Medical ICU, mixed population |
| LVEF | SAPS II (54 [48−72] vs 51 [45–55]) |
| Total 68 (48 vs 20) | ||||
| Crit Care | PS (7 cmH2O), no PEEP | DTE, E/e’, e’ | ||
| Last 1 h | ||||
| Konomi, 2016 | General ICU, mixed population |
| LVEF | SOFA (8.1 ± 3.8 vs 13 ± 8.4) |
| Total 42 (27 vs 15)a | ||||
| Anaesth Intensive Care | T-tube | E, A, E/A, DTE, e’, E/e’ | APACHE II (15.6 ± 6 vs 17.7 ± 6) | |
| Last 2 h | ||||
| Luo, 2017 | Four General ICU, mixed population |
| LVEF | APACHE II (20 ± 6.4 vs 23.9 ± 4.7) |
| Total 60 (31 vs 29) | ||||
| BMC Pulm Med | T-tube (supine 30°-45 °) | The study included only patients passing the SBT and extubated | E, E/e’ | |
| Last 30 min | ||||
| Haji, 2018 | General ICU, mixed population |
| LVEF, | SAPS II (46 [36–57] vs 42 [33–46]) |
| Total 53 (42 vs 11) | ||||
| Crit Ultrasound J | PS (up to 10 cmH2O), PEEP (5 cmH2O) | E, E/A, DTE, E/e’, e’ LA area | APACHE II (20 [15–23] vs 20 [16–23]) | |
| Last 1 h | ||||
| Tongyoo, 2018 | General ICU, mixed population |
| LVEF, LV-EDA | SOFA (3.9 ± 2.5 vs 4.7 ± 2.5) |
| Total 52 (38 vs 14) | E, A, E/A, e’, E/e’ | |||
| Echocardiography | PS 8 cmH2O, PEEP 5 cmH2O | RV-EDA, RV/LV-EDA | ||
| Last 1–2 h | ||||
| Amarja, 2019 | General ICU |
| Eyeball systolic function | APACHE II (18 ± 6.6 vs 20.8 ± 5.6) |
| Total 161 (140 vs 21) | ||||
| Indian J Crit Care Med | PS with PEEP (support unclear) | E, A, E/A, DTE, e’, E/e’, a’, TAPSE | ||
| Duration unclear | ||||
| Kaltsi, 2019 | General ICU and CCU, mixed population |
| LVEF | Not reported |
| Total 19 (8 vs 11) | ||||
| Crit Care Res Pract | T-tube | E, A, E/A, e’, E/e’, DTE | ||
| Last 2 h | ||||
| Goudelin, 2020 | General ICU, mixed population |
| LVEF | SAPS 38.5 [30–53] |
| Total 59 (43 vs 16) | ||||
| Intensive Care Med | T-tube | E, A, E/A, e’, E/e’, DTE, TR jet vel, LA area | SOFA 6 [4–9] | |
| 30 min | ||||
| Zapata, 2023 | General ICU, mixed population |
| LVEF | SAPS III 64 [60−68] vs 65 [58–71] |
| Total 89 (56 vs 33) | E, A, E/A, e’, E/e’, | |||
| Medicina Intensiva | T-tube (semi-recumbent) | TAPSE | ||
| Last 30 min - 2 h | ||||
| Song, 2024 | Two ICUs, mixed population |
| MAPSE, VTI, E, E/A, e’, E/e’, TAPSE | APACHE II (19 [16–22] vs 21 [19–21]) |
| Total 51 (36 vs 15) | ||||
| Ann Intensive Care | PS 8 cmH2O, no PEEP | SOFA (6 [5–8] vs 6 [5–7]) | ||
| 2 h |
Echocardiography data reported refers to the data provided by authors as continuous variable. Δ: (delta) variation from baseline; A: late mitral inflow velocity; APACHE II: Acute Physiology and Chronic Health Disease Classification System II; CCU: Coronary Care Unit; DTE: deceleration time of the E wave; E: early mitral inflow velocity; e’: mitral annular early diastolic velocity; FiO2: fraction of inspired oxygen; HR heart rate; ICU: Intensive Care Unit; LA: left atrial; LVEF: left ventricular ejection fraction; LV-EDA: left ventricular end-diastolic area; LV-EDD: left ventricular end-diastolic diameter; LV-ESD: left ventricular end-systolic diameter; MAPSE: mitral annular plane systolic excursion; NIV: non-invasive ventilation; PaCO2: arterial blood partial pressure of carbon dioxide; PaO2: arterial blood partial pressure of oxygen; PEEP: positive end expiratory pressure; PS: pressure support; RASS: Richmond Agitation-Sedation Scale; RVFAC: right ventricular fractional area changes; RV/LV-EDA: right ventricular to the left ventricular end-diastolic areas ratio; RR: respiratory rate; SAP: systolic arterial blood pressure; SBT: spontaneous breathing trial; SAPS II: Simplified Acute Physiology Score II; SOFA: Sequential Organ Failure Assessment; SpO2: peripheral blood oxygen saturation; s’: mitral annular systolic velocity; TAPSE: tricuspid annular plane systolic excursion; Vp: color M-mode Doppler velocity of propagation; VTI: Velocity time integral.
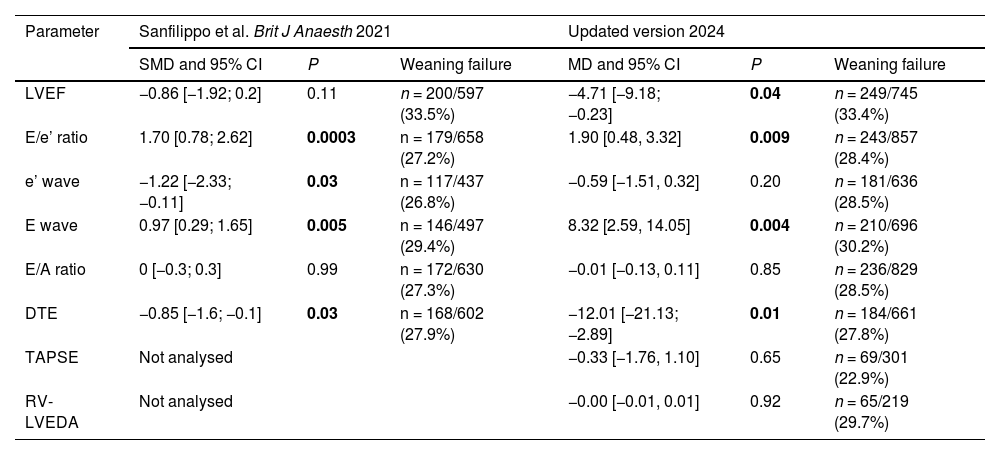
The methodological quality of the included studies performed with the NOS showed that seven studies had the maximum score (9 points),26–29,37–39 six scored 8 points30–35 and one scored 7 points36; thus all studies were judged at low risk of bias. Also the two studies using a longer time-frame for reintubation and used for sensitivity analysis had low risk of bias.15,42 The assessment of the risk of bias for each study is provided separately as Supplementary material (Appendix B). In Table 2 we provide a comparison of the results between the previous and the updated metanalysis, reporting also the sample size and the weaning failure rate.
Comparison of the findings of the previous metanalysis and the present update. Results of the previous work are reported as standardized mean difference (SMD), whilst resuls of the current update are expressed in terms of Mean Difference (MD).
| Parameter | Sanfilippo et al. Brit J Anaesth 2021 | Updated version 2024 | ||||
|---|---|---|---|---|---|---|
| SMD and 95% CI | P | Weaning failure | MD and 95% CI | P | Weaning failure | |
| LVEF | −0.86 [−1.92; 0.2] | 0.11 | n = 200/597 (33.5%) | −4.71 [−9.18; −0.23] | 0.04 | n = 249/745 (33.4%) |
| E/e’ ratio | 1.70 [0.78; 2.62] | 0.0003 | n = 179/658 (27.2%) | 1.90 [0.48, 3.32] | 0.009 | n = 243/857 (28.4%) |
| e’ wave | −1.22 [−2.33; −0.11] | 0.03 | n = 117/437 (26.8%) | −0.59 [−1.51, 0.32] | 0.20 | n = 181/636 (28.5%) |
| E wave | 0.97 [0.29; 1.65] | 0.005 | n = 146/497 (29.4%) | 8.32 [2.59, 14.05] | 0.004 | n = 210/696 (30.2%) |
| E/A ratio | 0 [−0.3; 0.3] | 0.99 | n = 172/630 (27.3%) | −0.01 [−0.13, 0.11] | 0.85 | n = 236/829 (28.5%) |
| DTE | −0.85 [−1.6; −0.1] | 0.03 | n = 168/602 (27.9%) | −12.01 [−21.13; −2.89] | 0.01 | n = 184/661 (27.8%) |
| TAPSE | Not analysed | −0.33 [−1.76, 1.10] | 0.65 | n = 69/301 (22.9%) | ||
| RV-LVEDA | Not analysed | −0.00 [−0.01, 0.01] | 0.92 | n = 65/219 (29.7%) | ||
CI: Confidence Interval. DTE: deceleration time of the E wave; E: early mitral inflow velocity; e’: mitral annular early diastolic velocity; LVEF: left ventricular ejection fraction; TAPSE: tricuspid annular plane systolic excursion. ;), with high heterogeneity (I2 = 84%, p < 0.0001).
Among the included studies, we found LVEF data on 745 patients from 12 studies.26–29,31–37,39 Four studies approached the SBT in PSV and eight in T-tube trial. The overall weaning failure was 33.4% (n = 249/745). The weaning failure rate was 36.7% (n = 194/528) with T-tube trial and 25.3% (n = 55/217) with PSV. Weaning failure was significantly associated with lower LVEF: MD −4.71 95%CI [−9.18, −0.23]; p = 0.04, Fig. 1), with high heterogeneity (I2 = 90%, p < 0.0001). There were no subgroup differences according to the type of SBT (p = 0.92, I2 = 0%). Two further subgroup analyses were conducted (Figures in Supplementary material (Appendix B)). When dividing the twelve studies according to the mean LVEF in the upper and lower half, we found no subgroup differences (p = 0.91, I2 = 0%); similarly, when separating subgroups according to studies with a mean LVEF > or <50% (n = 8 and n = 4, respectively), we found no subgroup differences (p = 0.55, I2 = 0%).
Forest plot comparing values of left ventricular ejection fraction between critically ill patients experiencing weaning failures vs successes. Studies are analysed in sub-groups according to the modality of spontaneous breathing trial.
CI: confidence interval; df: degrees of freedom; IV: inverse variance, SD: standard deviation.
The TSA performed to explore the robustness of the analysis regarding the impact of LVEF on the outcome of weaning from MV and computed with a MD of −4.71% showed that more research is needed. In fact, the Z-curve did not cross the adjusted boundaries nor reached the information size required (n = 745/1378, Fig. 2). Grade of evidence according to the current recommendations resulted in a low certainty of evidence (Supplementary material (Appendix B)).
Trial sequential analysis on the impact of left ventricular ejection fraction (LVEF) on the outcome of weaning from mechanical ventilation. The Z-curve describes the results after pooling data on 745 patients. The curve crosses the 1.96 × standard deviation, suggesting a significant result; however it also lays in the area between the adjusted boundaries (curved line on the top) and the futility (triangular) area, meaning that results are not robust.
MD, mean difference; RE, random effect.
Data on E/e’ ratio were gathered from 857 patients included in 13 studies,26–34,36–39 six in the PSV and seven in the T-tube trial subgroups. One study38 reported the values of E/e’ for both septal and lateral annulus; the analysis is presented with data from the average of their mean and SD. As shown in Fig. 3, weaning failure was confirmed as significantly associated with higher E/e’ ratio: MD 1.90, 95%CI [0.48, 3.32]; p = 0.009), with high heterogeneity (I2 = 84%, p < 0.0001), and no subgroup differences according to the type of SBT (p = 0.68, I2 = 0%). The subgroup analysis performed according to the regional criteria of TDI sampling showed significant differences between subgroups (p = 0.02, I2 = 75.3%; Supplementary material (Appendix B)), with greater association for the average E/e’ values and weaning failure. Analyses performed with either the septal or the lateral E/e’ values from Song et al.38 did not produce statistical changes.
Forest plot comparing values of E/e’ ratio between critically ill patients experiencing weaning failures vs successes. Studies are analysed in sub-groups according to the modality of spontaneous breathing trial.
CI: confidence interval; df: degrees of freedom; IV: inverse variance; SD: standard deviation.
Data on TDI e’ wave were available from 585 patients includeed in 10 studies,26,28–30,33,34,36–39 five in the PSV and five in the T-tube trial subgroups. As above, Song et al.38 reported both septal and lateral e’ values; the analysis is presented with data from average of their mean and SD. Weaning failure was not confirmed as associated with lower e’ wave values: MD −0.59, 95%CI [−1.51, 0.32]; p = 0.20, Fig. 4), with moderate heterogeneity (I2 = 64%, p = 0.003). There were no subgroup differences according to the type of SBT (p = 0.67), with no heterogeneity (I2 = 0%). The subgroup analysis performed according to the regional criteria of TDI sampling showed significant differences between subgroups (p = 0.03, I2 = 72.2%), with greater association for the average e’ wave values and weaning failure (Supplementary material (Appendix B)). Analyses performed with the septal or the lateral e’ values from Song et al.38 did not affect the above-mentioned statistical findings.
Forest plot comparing values of e’ wave between critically ill patients experiencing weaning failures vs successes. Analysis is performed in sub-groups according to the modality of spontaneous breathing trial.
CI: confidence interval; df: degrees of freedom; IV: inverse variance; SD: standard deviation.
The E wave data were available on 696 patients from 11 studies,26–30,33,34,36–39 five in the PSV and six in the T-tube trial subgroups. Weaning failure was significantly associated with higher E wave velocity: MD 8.32, 95%CI [2.59, 14.05]; p = 0.004), with moderate heterogeneity (I2 = 54%, p = 0.02). There were no subgroup differences according to the type of SBT (p = 0.29, I2 = 11.5%; Supplementary material (Appendix B)).
Data on E/A ratio were reported by 12 studies including 829 patients,26,29–37,39 five in the PSV and seven in the T-tube trial subgroups. Weaning failure was confirmed as not significantly associated with E/A ratio: MD −0.01, 95%CI [−0.13, 0.11]; p = 0.85), with mild heterogeneity (I2 = 47%, p = 0.04). There were no subgroup differences according to the type of SBT (p = 0.70, I2 = 0%; Supplementary material (Appendix B)).
The data on deceleration time of the E wave (DTE) were available from 661 patients from 9 studies,26,28–31,33,35–37 three in the PSV and six in the T-tube trial subgroups. Weaning failure was confirmed as significantly associated with lower DTE: MD −12.01, 95%CI [−21.13,−2.89]; p = 0.01), with no heterogeneity (I2 = 0%, p = 0.46). There were no subgroup differences according to the type of SBT (p = 0.99, I2 = 0%; Supplementary material (Appendix B)).
Parameters for the evaluation of RV systolic functionThe values of TAPSE according to weaning were reported by three studies,30,38,39 with data on a total of 301 patients. One study performed SBT with T-tube and two with PSV. The overall weaning failure was 22.9% (n = 69/301). TAPSE was not different between weaning failure and success groups: MD −0.33 95%CI [−1.76, 1.10]; p = 0.65), with no heterogeneity (I2 = 0%, p = 0.50; Supplementary material (Appendix B)). No subgroup analysis was conducted due to paucity of data.
Three studies reported the values of the ratio between the RV and the LV end-diastolic area (RV-LVEDA) according to weaning,29,31,34 with data on a total of 219 patients (two studies performed SBT with T-tube and one with PSV). The overall weaning failure was 29.7% (n = 65/219). The RV-LVEDA was not different between groups: MD: −0.00 95%CI [−0.01, 0.01]; p = 0.92), with no heterogeneity (I2 = 0%, p = 0.79; Supplementary material (Appendix B)). As for TAPSE, no subgroup analysis was conducted.
Sensitivity analysesTwo studies used a longer timeframe for reintubation criteria (one week, rather than 48 h).15,42 The inclusion of these two studies to the evaluation of LVEF in predicting weaning outcome did not affect the result (MD: −4.20 95%CI [−8.35, −0.05]; p = 0.049). Similarly, the inclusion of these data on the E wave, the E/e’ and the E/A ratios did not change the statistical meaning of the results shown in the primary analysis (p = 0.005, p = 0.009 and p = 0.91, respectively).
When conducting 12 sensitivity analyses with “leave-one-out at time” for the primary outcome (LVEF), in six cases the association of lower LVEF with weaning failure remained significant, whilst in the other half became not significant (p ranging from 0.051 to 0.07). Regarding the E/e’ ratio and the e’ wave, we conducted 13 and 10 sensitivity analyses removing one study at time, respectively. All these analyses confirmed the significant association of higher E/e’ ratio and weaning failure and the lack of association of the weaning outcome with e’ wave velocity. We did not identify non-prospective studies reporting the LVEF, and none of the studies were classified at high risk of bias. Hence, the other two preplanned sensitivity analyses were not conducted.
DiscussionWe conducted this pre-planned updated metanalysis primarily to explore the association of weaning failure from MV with LVEF, the only parameter describing LV systolic dysfunction consistently investigated and reported in the previous metanalysis.18 That analysis resulted in an unclear link between LVEF and weaning failure (p = 0.11), with no evaluation of its robustness with TSA. Moreover, the effect was statistically described by standardized means (instead of MD), with no signal on the clinical relevance and magnitude of the difference. The present update was pre-planned (registration in PROSPERO database); despite we retrieved only three further studies in the updated search (with only two providing usable data on LVEF), it increased the sample size of data ranging between 20% and 30%. We found that lower LVEF was significantly associated with weaning failure; however, this result should be interpreted cautiously for at least three reasons. First, in term of magnitude of effect, the MD in LVEF between groups was lower than 5%, a value well-below the known intra- and inter-observer variability.43,44 The second reason is linked to the statistical fragility of our finding as in half of the sensitivity analyses conducted removing one study at time the association with weaning failure was lost; moreover, the TSA suggested that the result is not robust and more research would be needed before drawing firm conclusions. A third reason for suggesting caution is that lower LVEF could partially act as a surrogate for altered diastolic function and increased filling pressure. Indeed, according to the most recent guidelines,45 any patient with depressed LVEF is diagnosed by definition with LVDD. Moreover, it is becoming increasingly apparent the “U-shaped” effects of LVEF on clinical outcomes in the ICU setting,46 with negative impact on the outcome of critically ill patients also from hyperdynamic LVEF,47,48 a finding confirmed by a recent metanalysis.49 However, whether a hyperdynamic LVEF has negative effects at the time of weaning from MV has not been adequately investigated.
Other parameters describing the LV systolic function (i.e. the s’ TDI wave) could be valuable during the weaning process; differently from the LVEF, s’ TDI wave has a more linear association with outcome,48 although its predictive value remains controversial.50 In our metanalysis the s’ TDI wave was described by one study only.29 The mitral annular plane systolic excursion (MAPSE) is an interesting echocardiographic parameter in the critically ill patients, at least for its simplicity and reproducibility.51 MAPSE describes longitudinal LV systolic function but it was reported only by one study in the context of weaning38 and therefore analysis was not feasible. Similarly, strain echocardiography, which seems associated with prognosis in septic patients,52 has not been yet adequately explored in the setting of weaning.
The shift to negative pressure ventilation during weaning produces both an increase in venous return (which may cause issues in patients with LVDD and higher LV filling pressures),53 and an increase in LV afterload, especially if significant inspiratory efforts are made.54 In this update, we confirmed the association of higher E/e’ ratio with weaning failure. Apart from being physiologically sound, a MD between groups of almost 2 points could be a clinically relevant difference. Moreover, the inter- and intra-individual variability for this parameter is relatively low.55,56 Notably, E/e’ ratio is the most used surrogate marker of increased LV filling pressure. Cut-off values of E/e’ suggested by the guidelines refer to the outpatient setting,57 and much lower values (7.5–9) are associated with increased LV filling pressures in patients supported by MV.58,59 Conversely, we found no association of e’ velocity values and outcome of weaning in this updated meta-analysis, contraddicting our previous findings.18 Nonetheless, previous literature suggests the importance of e’ velcoity on the outcome of critically ill patients with sepsis.60 With regard to weaning, Moschietto et al. showed that improvements in e’ during the course of SBT were positively associated with weaning success, suggesting the importance of a LV relaxation reserve during weaning. Further, a significant association of lower e’ values and weaning failure was seen in our sub-group analyses, and particularly according to sampling site (average e’) and SBT mode (PSV). In light of these arguments and considering the association of lower values of e’ velocity with outcome in septic patients,60 the present metanalysis suggests the fragility of results not only regarding LVEF but also of e’ velocity. The link between LVDD and worse outcomes in weaning remains highly likely, considering also the results of E wave velocity and DTE, both pointing towards an association of weaning failure and worse LV relaxation.53 The increase of E wave velocity during the SBT reflects the increased venous return with the shift to negative pressure breathing. From a clinical standpoint, the management of these patients during weaning shuold be tailored with particular attentions on prevention of arrhythmias and tachycardia, reduction of afterload, avoidance of positive fluid balance whenever possible and early initiation of fluid removal.61
Apart lack of enough data on s’ TDI wave and on strain echocardiography, we found inadequate reporting in the context of weaning of left atrial size and tricuspid regurgitation jet velocity (variables currently recommended for the evaluation of LV diastolic function57). Regarding the influence of RV function on weaning outcome we found another gap in the literature, though we were able to pool data from a very limited number of studies regardig the TAPSE and the RV-LVEDA. In both cases the results suggested not differences between groups.
Finally, results were consistent across SBT appraoches performed with either T-tube or PSV. Some authors suggested that T-tube trial could be a more challenging test for the cardiorespiratory function,62 but a meta-analysis showed that both approaches are comparable in predicting the outcomes of weaning.63 Moreover, a recent large randomized controlled trial suggested that, in patients at high risk of extubation failure, SBT performed with PSV do not improve outcomes as compared to T-piece.64
Our meta-analysis has several limitations. The major one is exploring just associations between one echocardiographic variable and the weaning outcome, with no adjustment for confounders by regression/multivariate analyses. Hence, we are not able to explore the clinical value of combining echocardiographic parameters as in the pioneer study by Lamia et al. where the combination of E/A and E/e’ ratio allowed an accurate noninvasive detection of weaning-induced pulmonary oedema in patients with difficult weaning.41 Further, we could not explore the prognostic value of a more holistic evaluation, where echocardiography is added to other ultrasound imaging (i.e. lung and/or diaphragm) or labaraturistic findings (i.e. troponin). In this regard, when exploring the outcome of weaning with echocardiography only, a more adequate approach would be probably to focus on the occurrence of weaning-induced pulmonary oedema (as studied by Liu et al.),12 as compared to using as outcome non-specific weaning failure, where non-cardiac factors may act as confounders. However, in this study the authors did not find an association between this phenomenon and concomitant myocardial ischemia.12 Similarly, Bedet et al. found no association of weaning-induced cardiac ischemia with weaning-induced pulmonary edema nor with weaning outcomes.15
From a clinical standpoint, our results suggest particular attention to the weaning in patients with increased LV filling pressures and possibly in those with abnormal LVEF, though a proper interpretation could be made only with an individual pateints data metanalysis. Such issue is common to the other meta-analyses conducted in the field of critically care echocardiography,60,65,66 mainly due to large heterogeneity in data reporting.67 Second, we evaluated the association between echocardiography data performed before the SBT is started with the weaning outcome. However, it could be very valuable to explore changes of echocardiography parameter from their baseline during the course of weaning attempt. In this regards, Moschietto et al. showed that increase in e’ during SBT could be a positive predictor of weaning success.28 Goudelin et al. showed also that an echocardiography-guided treatment enabled to successfully extubate all the patients that previously failed the SBT.37 A third limitation is that the included studies enrolled critically ill patients with different pathologies with significant clinical heterogeneity, spamming from those with heart failure and patients with normal premorbid heart performance. Forth, the included studies did not consistently report hemodynamic data at the time of echocardiography, nor described if any patient had developed LV outflow tract obstruction or experienced worsening of mitral regurgitation. Clearly, patients developing any of these two, would have experienced an increase in LA pressures facilitating the occurrence of pulmonary oedema, and further reducing the cardiac output. All these factors are confounders that add complexity to the topic. Moreover, another confounding effect may be introduced by “non-cardiac” causes of weaning failure (i.e. respiratory and/or diaphragmatic), though the cardiac function is the commonest cause of weaning failure12. Finally, statistical heterogeneity was moderate to high in most of our analyses.
ConclusionsThe association between failure to wean from MV and worse LV systolic performance as evaluated by LVEF is possible, but such result seems very fragile for several reasons. The difference in LVEF between failures and successes is well-below a clinically relevant inter- and intra-observer variability, and results are not robust. Weaning failure confirms its association with elevated LV filling pressures, and in general with parameters indicating worse LV diastolic function, though the role of e’ is now questioned. There is still a gap in the literature regarding weaning failure and other echocardiographic parameters describing LV performance (i.e. s’ TDI wave, MAPSE and longitudinal strain), as well as with those evaluating RV function.
CRediT authorship contribution statement- •
Conception and design: CS, AN, EB, SS, AM, FS
- •
Screening of automated search: FS, AP, CS
- •
Consensus on discrepancies: AN, AM
- •
Independent manual search: CS, SM, MZ, FS
- •
Acquisition of data and/or data cross-check: FS, AP, AN, CS, MZ
- •
Analysis: CS, SM, AN, FS
- •
Risk of Bias Assessment: CS, AP, MZ, FS
- •
Interpretation of data: FS, AN, CS, AM, EB, SS, MZ
- •
Drafting the article: CS, MZ, FS
- •
Critically Revising draft for important intellectual content: AM, EB, SS, AN, SM, AP
All Authors.
FundingNo funding was received for this study.
Declaration of Generative AI and AI-assisted technologies in the writing processAI program Resub.app was used to check adherence to journal formatting.
The authors declare that they have no conflict of interest related to the present research.
None.