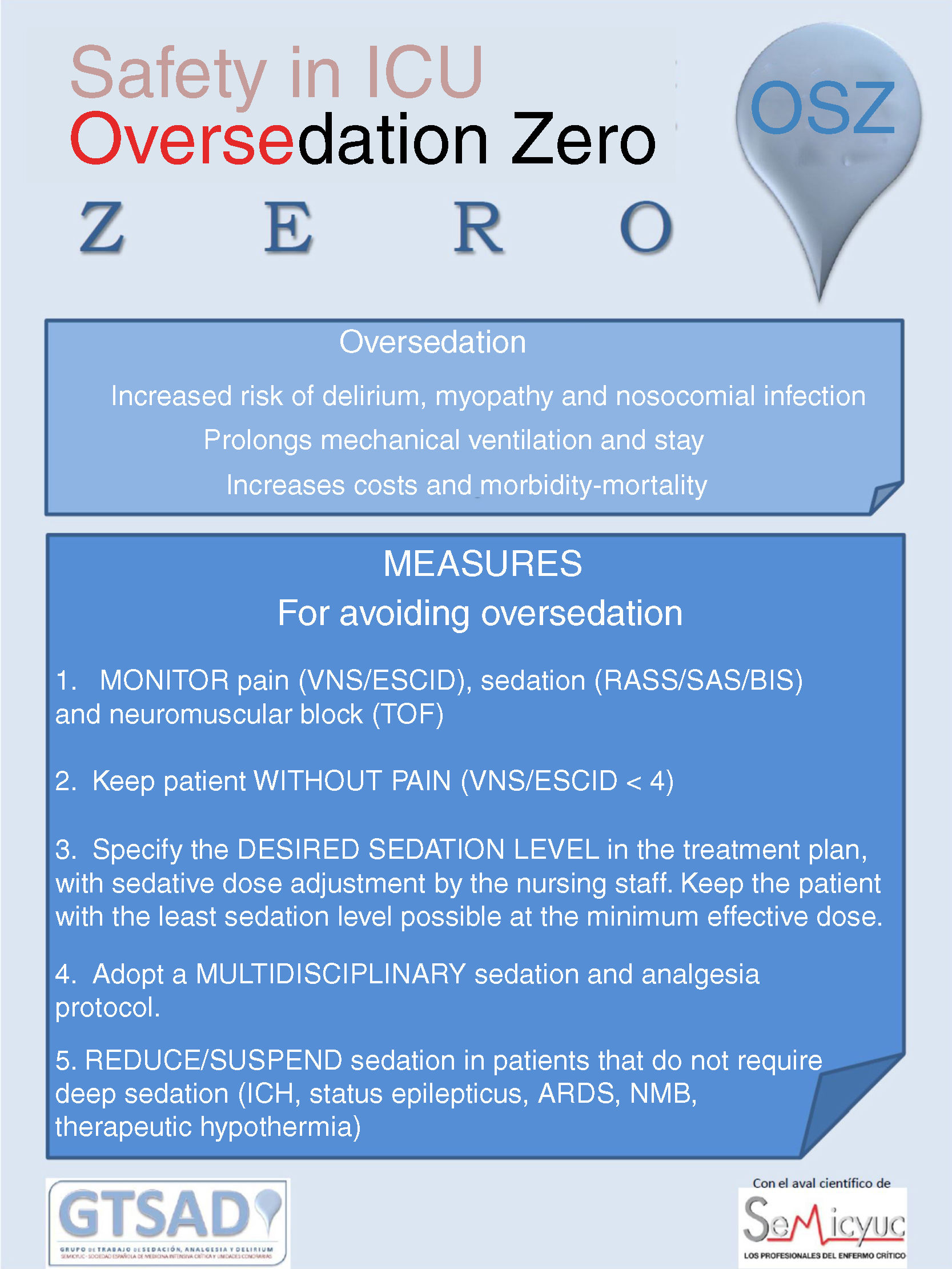
Sedation is necessary in the management of critically ill patients, both to alleviate suffering and to cure patients with diseases that require admission to the intensive care unit. Such sedation should be appropriate to the patient needs at each timepoint during clinical evolution, and neither too low (undersedation) nor too high (oversedation). Adequate sedation influences patient comfort, safety, survival, subsequent quality of life, bed rotation of critical care units and costs. Undersedation is detected and quickly corrected. In contrast, oversedation is silent and difficult to prevent in the absence of management guidelines, collective awareness and teamwork. The Zero Oversedation Project of the Sedation, Analgesia and Delirium Working Group of the Spanish Society of Intensive and Critical Care Medicine and Coronary Units aims to offer a practical teaching and collective awareness tool for ensuring patient comfort, safety and management with a view to optimizing the clinical outcomes and minimizing the deleterious effects of excessive sedation. The tool is based on a package of measures that include monitoring pain, analgesia, agitation, sedation, delirium and neuromuscular block, keeping patients pain-free, performing dynamic sedation according to clinical objectives, agreeing upon the multidisciplinary protocol to be followed, and avoiding deep sedation where not clinically indicated.
La sedación es necesaria en el tratamiento de los pacientes críticos, tanto para aliviar el sufrimiento como para curar a los pacientes con enfermedades que precisan el ingreso en unidades de cuidados intensivos. Esta sedación debe ser la adecuada a las necesidades del paciente en cada momento de su evolución clínica, ni por debajo (infrasedación) ni por encima (sobresedación). Una sedación adecuada influye en la comodidad, la seguridad, la supervivencia, la calidad de vida posterior, la rotación de camas de las unidades de críticos y los costes. La infrasedación se detecta y corrige rápidamente. Sin embargo, la sobresedación es silente y difícil de prevenir sin unas pautas de actuación, una concienciación colectiva y un trabajo en equipo. El proyecto «Sobresedación Zero» del Grupo de Trabajo de Sedación, Analgesia y Delirium de la Sociedad Española de Medicina Intensiva, Crítica y Unidades Coronarias pretende ser una herramienta docente, práctica y de concienciación colectiva de comodidad, seguridad y gestión para maximizar el resultado clínico y minimizar los efectos perjudiciales de la sedación excesiva. Se basa en un paquete de medidas que se incluye monitorizar el dolor, la analgesia, la agitación, la sedación, el delirium y el bloqueo neuromuscular, mantener a los pacientes sin dolor, realizar una sedación dinámica según objetivos clínicos, consensuar el protocolo multidisciplinar a seguir y evitar la sedación profunda no indicada clínicamente.
Sedation is necessary in the intensive care of the critically ill. The administration of analgesics and hypnotics in critical patients is a common practice in Intensive Care Units (ICUs) throughout the world. Sedation of the critical patient in the ICU should be understood as forming part of a bundle of measures addressing aspects such as analgesia, delirium, humanization, early mobilization and the facilitation of nighttime sleep.1,2 The reasons why sedation is necessary in critical patients include the reduction of anxiety and oxygen consumption, the control of agitation, and the facilitation of tolerance of the orotracheal tube, mechanical ventilation and/or other invasive techniques.
Over the years, the evidence-based international clinical practice guides (CPGs) on the management of analgesia, sedation and delirium have consistently recommended mild analgesia levels, as these are associated to better clinical outcomes.2–5 In contrast, deep sedation started early upon admission to the ICU has been independently associated to a delay in extubation and to increased early and late patient mortality.6
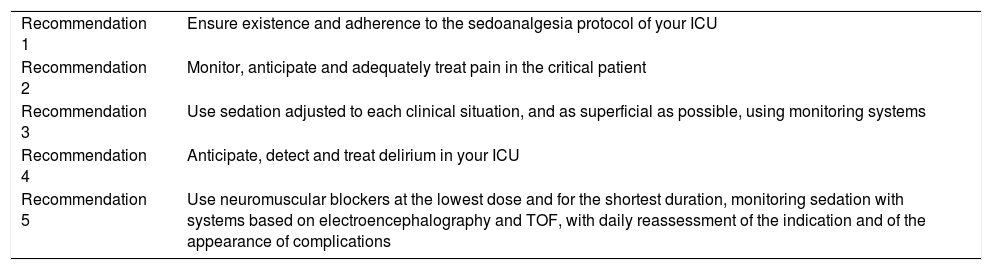
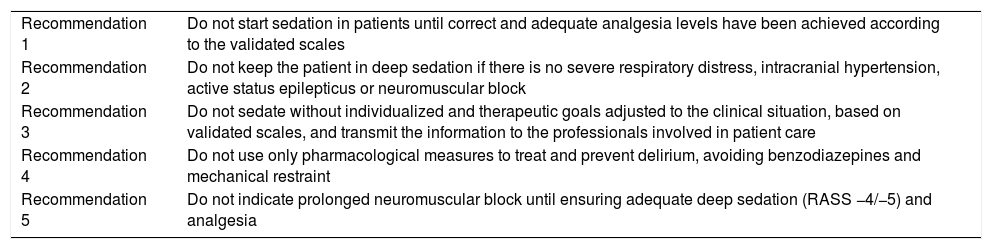
In 2008, in the journal Medicina Intensiva, the Sedation and Analgesia Working Group of the Spanish Society of Intensive and Critical Care Medicine and Coronary Units (Sociedad Española de Medicina Intensiva, Crítica y Unidades Coronarias [SEMICYUC]) – created in the year 2007 – published recommendations on short and long duration sedation, difficult sedation, delirium and neuromuscular block in the ICU.7–11 The Working Group incorporated the “D” for “delirium” to its name in 2017, becoming the Sedation, Analgesia and Delirium Working Group (Grupo de Trabajo de Sedación, Analgesia y Delirium [GTSAD]). It also participated in the elaboration of the evidence-based Pan-American Clinical Practice Guide for the management of sedoanalgesia in critically ill adults3; in the critical patient “Do”12 (Table 1) and “Do not do”13 (Table 2) SEMICYUC Working Group recommendations; and in the Critical Patient Quality Indicators of the SEMICYUC.14
“Do” recommendations of the GTSAD/SEMICYUC for the management of critical patients.
| Recommendation 1 | Ensure existence and adherence to the sedoanalgesia protocol of your ICU |
| Recommendation 2 | Monitor, anticipate and adequately treat pain in the critical patient |
| Recommendation 3 | Use sedation adjusted to each clinical situation, and as superficial as possible, using monitoring systems |
| Recommendation 4 | Anticipate, detect and treat delirium in your ICU |
| Recommendation 5 | Use neuromuscular blockers at the lowest dose and for the shortest duration, monitoring sedation with systems based on electroencephalography and TOF, with daily reassessment of the indication and of the appearance of complications |
GTSAD: Sedation, Analgesia and Delirium Working Group (Grupo de Trabajo de Sedación, Analgesia y Delirium [GTSAD]); SEMICYUC: Spanish Society of Intensive and Critical Care Medicine and Coronary Units (Sociedad Española de Medicina Intensiva, Crítica y Unidades Coronarias [SEMICYUC]); TOF: train-of-four.
Source: Hernández-Tejedor et al.12
“Do not do” recommendations of the GTSAD/SEMICYUC for the management of critical patients.
| Recommendation 1 | Do not start sedation in patients until correct and adequate analgesia levels have been achieved according to the validated scales |
| Recommendation 2 | Do not keep the patient in deep sedation if there is no severe respiratory distress, intracranial hypertension, active status epilepticus or neuromuscular block |
| Recommendation 3 | Do not sedate without individualized and therapeutic goals adjusted to the clinical situation, based on validated scales, and transmit the information to the professionals involved in patient care |
| Recommendation 4 | Do not use only pharmacological measures to treat and prevent delirium, avoiding benzodiazepines and mechanical restraint |
| Recommendation 5 | Do not indicate prolonged neuromuscular block until ensuring adequate deep sedation (RASS −4/−5) and analgesia |
GTSAD: Sedation, Analgesia and Delirium Working Group (Grupo de Trabajo de Sedación, Analgesia y Delirium [GTSAD]); RASS: Richmond Agitation Sedation Scale; SEMICYUC: Spanish Society of Intensive and Critical Care Medicine and Coronary Units (Sociedad Española de Medicina Intensiva, Crítica y Unidades Coronarias [SEMICYUC]).
Source: González de Molina-Ortiz et al.13
Although all these clinical practice guides recommend mild sedation levels, the surveys carried out in different countries to evidence real life clinical practices have revealed discrepancies between the recommendations and routine clinical practice.15 Notwithstanding the response biases which studies of this kind may have, the published data indicate that there is a high percentage of patients subjected to sedation levels that are deeper than clinically necessary or justified. In the years 2013 and 2014, the GTSAD conducted surveys that have been recently published, confirming the gap between the established recommendations and routine clinical practice.16
Adequate sedation should be dynamic, affording comfort for the critical patient while avoiding both under- and oversedation. In this regard, undersedation can cause patient discomfort, stress and the self-removal of medical devices. In contrast, oversedation is more silent, proves less noticeable, and is more tolerated, and can give rise to increased morbidity-mortality. Health professionals need to be aware of this fact in order to detect and avoid oversedation. The mentioned increase in morbidity-mortality leads to safety problems for the patient, since it implies poorer clinical outcomes, an increased duration of mechanical ventilation, longer ICU and in-hospital stay, and higher costs. In this context, some studies have reported oversedation rates of 35%.17
Excessive sedation of critical patients unresponsive to stimuli has been shown to be an independent mortality risk factor. In addition, deep sedation has been associated to deleterious effects such as myopathy, myocardial depression, hemodynamic instability, ileus, an increased risk of pressure ulcers, immune suppression, acquired muscle weakness, short- and long-term cognitive and/or psychic dysfunction, delirium, respiratory depression, diaphragmatic dysfunction, increased dependency upon mechanical ventilation, increased pneumonia risk, longer ICU and in-hospital stay, and higher costs.6,18–20
ObjectivesThe “Oversedation Zero” project of the GTSAD seeks to propose tools to avoid oversedation, ensure patient comfort, and improve patent safety and clinical outcomes, and bed management.
Deep sedation is not always equivalent to oversedation. Deep sedation is initially indicated in patients with acute respiratory distress syndrome (ARDS), intracranial hypertension (ICH) or status epilepticus (SE), or subjected to neuromuscular block (NMB).
The definition of oversedation is fundamented upon three scenarios. The first scenario refers to a patient with a sedation level deeper than that established as the target for that patient, during the day in question and as evidenced by two or more consecutive measurements. Sedation should be administered dynamically according to clinical objectives and not based on fixed doses.8 The second scenario refers to a patient with deep sedation lacking clinical justification, i.e., a patient with none of the aforementioned clinical situations warranting deep sedation. The third scenario in turn refers to a patient in which deep sedation is justified, with objective monitoring using devices based on electroencephalography (EEG), but presenting suppression rates or sedation levels so deep that they exceed the anesthetic range.
MethodologyThe “Oversedation Zero” project was created in the setting of the Working Group with the purpose of avoiding excessive sedation in the ICU. During the meeting of the GTSAD on occasion of the SEMICYUC Congress of 2012, this divulgation project was proposed as a complement to the study of sedation and analgesia practice in Spanish ICUs. Through both telematics and physical presence meetings of the GTSAD during the following national SEMICYUC congresses and on occasion of the winter meetings in the SEMICYUC national head offices, consensus was reached regarding the causes of oversedation, the objectives for avoiding it, and the bundle of measures to be divulgated by the members of the GTSAD. All this was done under the guidance of the coordinators, vice-coordinators and secretary of the Working Group.
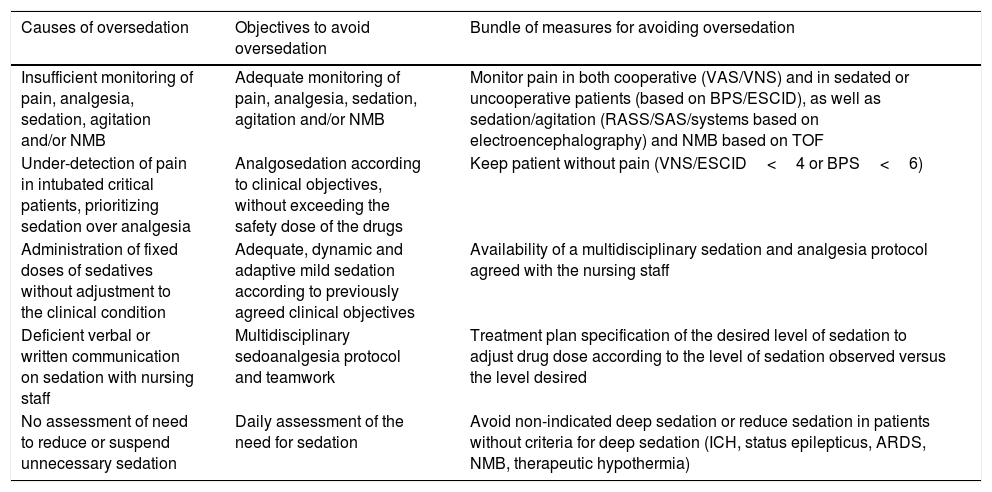
The members of the GTSAD established consensus on 5 possible causes of oversedation (Table 3). The first cause is the provision of insufficient analgesia in intubated critical patients, placing priority on sedation (sedoanalgesia) over analgesia (analgosedation). Both the PAD4 and the PADIS guides,2 and the eCASH concept,1 recommend sedation management based on analgesia.
Causes, objectives and recommendations of the “Oversedation Zero” project of the GTSAD.
| Causes of oversedation | Objectives to avoid oversedation | Bundle of measures for avoiding oversedation |
|---|---|---|
| Insufficient monitoring of pain, analgesia, sedation, agitation and/or NMB | Adequate monitoring of pain, analgesia, sedation, agitation and/or NMB | Monitor pain in both cooperative (VAS/VNS) and in sedated or uncooperative patients (based on BPS/ESCID), as well as sedation/agitation (RASS/SAS/systems based on electroencephalography) and NMB based on TOF |
| Under-detection of pain in intubated critical patients, prioritizing sedation over analgesia | Analgosedation according to clinical objectives, without exceeding the safety dose of the drugs | Keep patient without pain (VNS/ESCID<4 or BPS<6) |
| Administration of fixed doses of sedatives without adjustment to the clinical condition | Adequate, dynamic and adaptive mild sedation according to previously agreed clinical objectives | Availability of a multidisciplinary sedation and analgesia protocol agreed with the nursing staff |
| Deficient verbal or written communication on sedation with nursing staff | Multidisciplinary sedoanalgesia protocol and teamwork | Treatment plan specification of the desired level of sedation to adjust drug dose according to the level of sedation observed versus the level desired |
| No assessment of need to reduce or suspend unnecessary sedation | Daily assessment of the need for sedation | Avoid non-indicated deep sedation or reduce sedation in patients without criteria for deep sedation (ICH, status epilepticus, ARDS, NMB, therapeutic hypothermia) |
NMB: neuromuscular block; BPS: Behavioral Pain Scale; ESCID: pain indicating behavioral scale (ESCID); VAS: visual analog scale; VNS: verbal numeric scale; GTSAD: Sedation, Analgesia and Delirium Working Group (Grupo de Trabajo de Sedación, Analgesia y Delirium [GTSAD]); ICH: intracranial hypertension; RASS: Richmond Agitation Sedation Scale; SAS: Sedation Agitation Scale; ARDS: acute respiratory distress syndrome; TOF: train-of-four.
The second cause is deficient or absent monitoring of analgesia, sedation or neuromuscular block. In cooperative patients pain should be monitored using visual scales such as the visual analog scale (VAS) or verbal scales such as the verbal numeric scale (VNS). In uncooperative or sedated patients, the recommendation is to use behavioral scales such as the behavioral pain scale (BPS)21 or the pain indicating behavioral scale (ESCID).22 Patients exhibiting behavior indicative of pain not noticed by the healthcare professionals of the critical care unit receive more sedation for symptoms controls, when in fact what would be indicated in such situations is treatment for pain. Such under-detection of pain due to insufficient pain monitoring in sedated patients may result in avoidable prolongation of mechanical ventilation – with all its deleterious implications.23 Regarding the monitoring of sedation and agitation, each individual ICU should decide which validated scale to use for monitoring sedation level, allowing all the professionals to speak a common language in this regard. The Richmond Agitation Sedation Scale (RASS) has become the most widely used instrument in the world for this purpose.24 Another useful tool is the Sedation Agitation Scale (SAS). A currently less useful and therefore less frequently used scale is the Ramsay score, which focuses more on the monitoring of sedation than agitation. Lastly, and in order to minimize the deleterious effects of neuromuscular block, justification of the latter must be established on a daily basis, with routine monitoring based on the train-of-four (TOF).
The third cause of oversedation is inadequate adjustment of the sedative dose to the clinical situation of the patient, maintaining a fixed perfusion of hypnotics which the patient might not actually need. This practice leads to an unnecessary accumulation of sedatives which the patient takes time to eliminate once the clinical condition for which sedation was initially prescribed has improved.
The fourth cause is deficient verbal and/or written communication regarding sedation among the professionals caring for the critical patient, or with no clear clinical objective for the desired level of sedation in the treatment regimen.
Lastly, the fifth cause of oversedation is the lack of daily assessment of the need to reduce sedation, determining whether the patient does not require deep sedation, or directly suspending sedation if the latter is no longer indicated.
One objective established by the GTSAD to avoid oversedation is mild and cooperative sedation based on analgesia or analgosedation, according to clinical criteria, without exceeding the drug safety doses. A second objective is to monitor pain, sedation/agitation and delirium. Analgesia is monitored using VNS or VAS in cooperative patients and behavioral scales in uncooperative or sedated patients. Sedation or agitation is monitored in all critical patients not subjected to neuromuscular block, using validated scales. If muscle relaxants are required, sedation is to be monitored objectively using electroencephalography-based techniques25 and neuromuscular block based on the TOF. A third objective is to ensure that sedation is mild in the absence of clinical contraindications to the effect, dynamic, adaptive and always guided by clinical objectives or targets. A fourth objective for avoiding oversedation is the availability of a multidisciplinary sedation protocol, allowing work as a team while minimizing therapeutic variability and empowering the nursing staff to manage hypnotic drug boluses and perfusions, as occurs in a sense with the perfusion of vasoactive drugs. Lastly, a fifth objective is daily assessment of the sedation requirements of the patients based on their individualized clinical circumstances, with reduction or suspension of the medication as required.
Bundle of measuresFollowing the analysis of the possible causes and the reaching of consensus regarding the objectives, the GTSAD produced a bundle of measures seeking to increase awareness of the deleterious consequences of oversedation and offer tools for avoiding it.
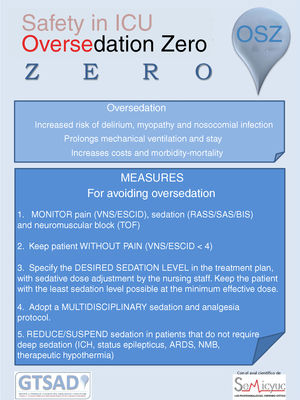
The bundle of measures comprises the availability of a multidisciplinary sedation and analgesia protocol agreed with the nursing staff; the monitoring of pain in both cooperative patients (VAS/VNS) and in sedated or uncooperative patients (BPS/ESCID), and the monitoring of sedation/agitation (RASS/SAS/BIS); keeping the patient without pain (VNS/ESCID<4 or BPS<6); due specification in the treatment plan of the desired level of sedation in order to adjust the drug doses according to the observed versus the desired level of sedation; and the avoidance of non-indicated deep sedation or the reduction of sedation in patients with no criterion for deep sedation (ICH, status epilepticus, ARDS, NMB, therapeutic hypothermia) (Fig. 1).
ImplementationThe “Oversedation Zero” project comprises four phases. The first phase refers to consensus among the members of the GTSAD regarding the best bundle of measures. The second phase comprises the study of the real-life analgosedation practices in Spanish ICU, as published by Garcia-Sanchez et al.16 The third phase involves divulgation of the bundle of measures at congresses and by means of the present manuscript. Finally, the fourth phase (still pending) is the conduction of a new study on the analgosedation practices, with a view to analyzing the differences with respect to the scenario in the years 2013 and 2014.
In this respect, as part of the divulgation phase, the project has been launched at two congresses of the SEMICYUC: the first on occasion of the LII congress of the SEMICYUC, which coincided with the XXX Pan-American congress held in Madrid in June 2014, and the second on occasion of the XXX congress of the SEMICYUC, held in San Sebastian in 2015, where posters were distributed among the participants for posting in the different ICUs throughout the country. Likewise, all the members of the GTSAD are engaged in divulgating activities in the ICUs where they work, and also in the context of their teaching functions.
On a concomitant basis, other bundles of measures have been developed internationally to improve the prognosis of critical patients. The best known is the “ABCDEF” protocol. Initially launched as the “ABCDE” initiative,26,27 it contemplated daily waking and spontaneous breathing tests, the adequate choice of analgesics and sedatives, the management of delirium, and early mobilization. In recent years, “A” has been referred to the management of pain, and “F” has been added in reference to empowerment of the family of the patient. Recent studies show the adoption of this bundle of measures to result in significantly improved survival statistics and clinical outcomes. According to a multicenter study published by Pun et al., compliance with the full bundle of measures of the “ABCDEF” protocol in 15,226 patients resulted in statistically significant reductions referred to in-hospital mortality after 7 days, the need for mechanical ventilation, coma, delirium, the need for mechanical restraints, readmission to the ICU, and patient transfer to sociosanitary centers. Furthermore, the authors recorded a directly proportional relationship between the degree of compliance with the bundle of measures and improvement of the abovementioned clinical outcomes. The investigators also evidenced increased reporting of pain – probably as a consequence of the monitoring of pain, which otherwise could have been underdiagnosed.28
Evaluation of the resultsThe success of the “Zero” projects endorsed by the Infectious Diseases and Sepsis Working Group (Grupo de Trabajo de Enfermedades Infecciosas y Sepsis [GTEIS]) of the SEMICYUC has been enormous. These projects include the “Bacteremia Zero”, “Pneumonia Zero” and “Resistance Zero” initiatives. The first of them demonstrated a decrease in bacteremia episodes secondary to catheter-related infection29; the second evidenced a decrease in nosocomial infections related to mechanical ventilation30; and the third demonstrated a decrease in antibiotic resistance in both the hospital setting and in the community – a genuine epidemic of the present century. In order to evidence these results, the GTEIS possesses a tool which for over two decades has made it possible to record the incidence of infections in the ICU, antibiotic use, clinical outcomes and risk factors: the Spanish National Nosocomial Infection Surveillance Study (Estudio Nacional de Vigilancia de Infección Nosocomial [ENVIN]).
In the years 2013 and 2014, the GTSAD conducted studies to know the real analgesia and sedation practices in the ICU.16 These initiatives were embodied in the Spanish National Analgesia and Sedation Surveillance Study (Estudio Nacional de Vigilancia de la Analgesia y la Sedación [ENVAS]). This registry has not been able to follow an annual periodicity in the way of the ENVIN. With this tool, the scientific community and critical care professionals may know whether the awareness-enhancing campaigns effectively result in changes in sedoanalgesia practices and – secondarily – in the clinical outcomes. Once this divulgation phase ends with the publication of the project, a new study is planned by the GTSAD on the real-life analgosedation practices in Spanish ICUs, with a view to evaluating the differences with respect to the studies conducted in 2013 and 2014. With due consideration of the limitations involved, the analysis of these differences could facilitate the evaluation of this national project.
The “Oversedation Zero” project focuses on patient-centered care and meets the criteria of a patient safety program, since it would allow the reduction of ICU and in-hospital stay, as well as of the morbidity-mortality associated to excessive sedation. This could also be illustrated in terms of the “Swiss cheese model”,31 whereby if a given problem (in this case oversedation) passes all the control filters, it ultimately reaches and causes harm to the patient.
ConclusionsThe scientific evidence and international clinical practice guides on the management of pain, agitation and delirium recommend mild sedation, which is associated to improved clinical outcomes. Under certain clinical circumstances, deep sedation is justified by the patient condition. However, oversedation needs to be detected and avoided. The GTSAD proposes a bundle of measures that seeks to increase collective awareness of this problem and to improve multidisciplinary communication among professionals. This bundle of measures addresses protocolization, monitoring, analgesia, communication and wakening. Real-life clinical practice registry and management tools will allow us to scale the problem, identify ways for improvement, establish more adequate teaching procedures, and evaluate the impact of adherence to the bundle of measures and to the international guidelines.
Financial supportThe authors declare that no financial support has been received for conduction of the present study.
Conflicts of interestJesus Caballero has received payment for traveling and housing expenses in the context of scientific meetings and teaching activities from Astellas, Sedana, Orion and Medtronic.
Manuela García has received payment for speeches from Medtronic and Orion.
Eduardo Palencia declares that he has no conflicts of interest.
Tomás Muñoz declares that he has no conflicts of interest.
Jose Manuel Gómez has received payment for speech moderator activities from Orion.
Isabel Ceniceros declares that she has no conflicts of interest.
The authors thank the SEMICYUC and the editorial board of Medicina Intensiva for support and kindness in facilitating the activity of the GTSAD in developing the bundle of measures and in promoting collective awareness.
Members of the Sedation, Analgesia and Delirium Working Group (Grupo de Trabajo de Sedación, Analgesia y Delirium [GTSAD])/Spanish Society of Intensive and Critical Care Medicine and Coronary Units (Sociedad Española de Medicina Intensiva, Crítica y Unidades Coronarias [SEMICYUC]).
Más información sobre los miembros del Grupo de Trabajo de Sedación, Analgesia y Delirium (GTSAD)/Sociedad Española de Medicina Intensiva, Crítica y Unidades Coronarias (SEMICYUC) están disponibles en el Appendix A.
Please cite this article as: Caballero J, García-Sánchez M, Palencia-Herrejón E, Muñoz-Martínez T, Gómez-García JM, Ceniceros-Rozalén I, et al. Sobresedación Zero como herramienta de confort, seguridad y gestión en la unidades de cuidados intensivos. Med Intensiva. 2020;44:239–247.