To determine the incidence of acute renal failure (ARF) in critically ill patients using the RIFLE and AKIN criteria.
DesignA prospective, multicenter observational study with a duration of one year from February 2010 was carried out. RIFLE and AKIN were employed using the urinary (UC) and creatinine criteria (CC) jointly and separately.
ScopeNine polyvalent Critical Care Units (CCUs) in Argentina.
PatientsA total of 627 critical patients over 18 years of age were admitted to the CCU for more than 48h. Exclusion criteria: inability to quantify diuresis, surgical instrumentation of the urinary tract, and need for renal support therapy (RST).
Variables of interestCalculated hourly diuresis (CHD) was used to apply the UC.
ResultsThe incidence of ARF was 69.4% and 51.8% according to RIFLE and AKIN, respectively. UC detected ARF in 59.5% of cases, while CC identified ARF in 34.7% (RIFLE) and 25.3% (AKIN). The mortality rate was 40.9% and 44.6% according to RIFLE and AKIN respectively, was significantly higher than in patients without ARF, and increased with disease severity (Data processing: Excel, SQL and SPSS. Levene test, comparison of means with Student t and chi-squared, with 95% confidence interval).
ConclusionsRIFLE identified more cases of ARF. UC proved more effective than CC. The presence of ARF and severity levels were correlated to mortality but not to days of stay in the CCU. Implementation of the unified CHD was useful for implementing UC and achieving comparable results.
Determinar la incidencia de insuficiencia renal aguda (IRA) en pacientes críticos usando RIFLE y AKIN.
DiseñoEstudio observacional prospectivo multicéntrico, realizado durante un año desde febrero de 2010. Se emplearon RIFLE y AKIN aplicando los criterios urinario (criterio U) y creatinina (criterio C) juntos y separados.
ÁmbitoNueve Unidades de Cuidados Críticos (UCC) polivalentes de Argentina.
PacientesUn total de 627 pacientes críticos mayores de 18 años de edad internados en UCC durante más de 48 h; motivos de exclusión: imposibilidad de cuantificar diuresis, instrumentación quirúrgica de la vía urinaria y necesidad de terapias de soporte renal (TSR).
Variables de interésSe utilizó una diuresis horaria calculada (DHC) para aplicar el criterio U.
ResultadosLa incidencia de IRA fue de 69,4 y 51,8% (RIFLE y AKIN, respectivamente). El criterio U detectó IRA en el 59,5% de los casos, mientras que el criterio C identificó IRA en el 34,7% (RIFLE) y 25,3% (AKIN). La mortalidad fue de 40,9 y 44,6% según RIFLE y AKIN, respectivamente, significativamente mayor a la de los pacientes sin IRA, y aumentó con la gravedad de la enfermedad. (Procesamiento de datos: Excel, SQL y SPSS. Test de Levenne, comparación de medias/promedios con t de Student y chi-cuadrado, con 95% de confianza).
ConclusionesRIFLE identificó más casos de IRA que AKIN. El criterio U fue más eficaz que el criterio C. La presencia de IRA y sus niveles de gravedad tuvieron correlación con la mortalidad pero no con los días de estancia en UCC. La implementación de la DHC fue útil para unificar la aplicación del criterio C y lograr resultados comparables.
There have been great difficulties for decades in defining the syndrome which we now refer to as acute renal failure (ARF). The inconvenience of not having a single definition was first addressed by a review in which 28 studies published in the period between 1965 and 19891 were seen to have used different criteria for diagnosing the condition.
In the year 2001, Bellomo, Kellum and Ronco2 proposed unification of the definition of ARF, and considered that only two of the multiple functions of the kidneys–urine production and the excretion of waste products of nitrogen metabolism–are easily and routinely determined in all Intensive Care Units (ICUs).3 Accordingly, in 2004 the Second International Consensus Conference of the Acute Dialysis Quality Initiative (ADQI)4 proposed the diagnosis and stratification of ARF according to the RIFLE classification, contemplating three levels or stages of acute renal dysfunction (“risk”, “injury” and “failure”) according to the changes in plasma creatinine levels or urine output.
The validity of this approach and its capacity to predict mortality have been evaluated by a number of studies. Ricci et al.,5 in a systematic review of all the studies using the RIFLE criteria between 2004 and 2007, identified 24 articles (with over 71,000 patients) that were scantly comparable among each other and moreover had clear weaknesses: small sample sizes, heterogeneous populations (healthy subjects, severe burn victims, bone marrow transplant patients, heart surgery patients, liver transplant patients, etc.), or participation of a single institution (single-center studies). Not surprisingly, the review reported an extremely variable incidence of ARF (10–82%).
The results of a second consensus conference with the participation of representative specialists in Critical Care Medicine and Nephrology (the Acute Kidney Injury Network) were published in 2007,6 and proposed the AKIN classification with the purpose of improving the sensitivity and specificity of the RIFLE system.
Large studies have evaluated both systems. In 2008, Bagshaw et al.7 published the results of the analysis of a database containing over 120,000 patients, comparing the RIFLE and AKIN systems. The incidence of ARF was 36.1% and 37.1%, respectively, and despite the weaknesses, the authors concluded that AKIN does not offer advantages in terms of sensitivity, consistency or predictive capacity with respect to RIFLE.
In 2008, Osterman et al.8 applied the AKIN classification in 22,300 patients, recording an incidence of ARF of 35.4% and a good correlation between the severity of ARF and the prognosis–though only the most severe disease grade was identified as an independent mortality predictor. In 2009, Joannidis et al.9 published a comparison of the RIFLE versus the AKIN system in 14,300 patients, based on the data of the SAPS-3. The incidence of ARF was found to be 28.5% and 38.5%, respectively, and the RIFLE classification showed greater consistency and a high ARF detection rate. However, the lack of urine output information biased the results, since AKIN grades 1 and 2, and RIFLE grades I and F, could not be differentiated. Both of the mentioned studies demonstrated an increase in morbidity-mortality associated to the development of ARF.
The recommendations of an international consensus conference held in Canada in 200710 with the purpose of establishing guidelines for the prevention and management of ARF in critical patients were published in 2010. The mentioned consensus document considered cystatin C to be a promising marker that appears to detect ARF earlier than changes in plasma creatinine. However, both this and other biomarkers (NGAL, kidney injury molecule-1, interleukin-18) are still in the investigational stages. It therefore was concluded that plasma creatinine remains the main marker (despite the disadvantages related to the influence of body weight, catabolic status, the presence of rhabdomyolysis, dilutional effects and drugs or other substances that alter creatinine secretion), along with the measurement of diuresis. The document thus recommends the RIFLE and AKIN criteria for diagnosing ARF, and points out that although validation is still needed, the AKIN system is able to identify ARF earlier than the RIFLE classification.
The present study analyzes the incidence of ARF in different ICUs, using the RIFLE and AKIN criteria applied in strict compliance with the consensus definitions, and compares the usefulness of both systems in predicting mortality and duration of stay in the ICU.
Patients and methodsStudy populationA prospective study of 627 patients from 9 polyvalent ICUs was carried out between February 2010 and February 2011 (Table 1). The study was approved by the Ethics Committee of each participating center.
Centers participating in the study.
| No. of beds | No. of cases | |
| Hospital Emilio Ferreyra Necochea, Buenos Aires, Argentina | 6 | 67 |
| Sanatorio Otamendi, CABA, Buenos Aires, Argentina | 16 | 73 |
| Hospital Italiano, CABA, Buenos Aires, Argentina | 28 | 197 |
| Sanatorio Nuestra Señora del Rosario, San Salvador Jujuy, Argentina | 12 | 160 |
| Other centers | 31 | 55 |
| Total | 124 | 627 |
CABA: Ciudad Autónoma de Buenos Aires; Other centers: Instituto Ecuatoriano de Seguridad Social (IESS) de Portoviejo, Manaví, Ecuador; Hospital Pablo Soria de San Salvador de Jujuy, Argentina; Hospital Municipal Ramón Santamarina de Tandil, Buenos Aires, Argentina; Hospital Municipal Agudos Leónidas Lucero de Bahía Blanca, Buenos Aires, Argentina.
The study included patients over 18 years of age admitted to the ICU for at least 48h, with evaluation during the first 7 days of admission. The exclusion criteria were: inability to quantify diuresis at any time during the study period, surgical instrumentation of the urinary tract (cystostomy, nephrostomy, urinary fistulas, etc.), and the need for renal support therapy (RST)–whether de novo (RIFLE “loss” and “end” stages) or chronic.
Data collection and analysisMicrosoft Excel was used for data collection, with recording of the following parameters: age, sex, ethnic origin, current body weight (reported by the patient or relatives), height, body mass index (BMI), the APACHE II and SOFA scores upon admission, disease leading to admission (clinical or surgical), days of stay in the ICU, and mortality in the ICU and 30, 60 and 90 days after discharge. The APACHE II and SOFA scores were calculated without excluding the creatinine parameters.
Urine collection was carried out in two ways depending on whether the patient carried a urinary catheter or not. In patients without a catheter, each micturition episode was quantified, while urine was collected every two hours in the patients with a bladder catheter. In both cases these amounts were used to calculate the hourly average from previous sampling.
In all cases hourly diuresis was expressed in relation to patient body weight, yielding the calculated hourly diuresis (CHD) reported in ml/kg/h. In all patients we recorded the daily measured plasma creatinine (MPC) value.
Based on the data referred to patient age, sex, ethnic origin and MPC, the Modification of Diet in Renal Disease (MDRD) formula11 was used to automatically calculate basal plasma creatinine (BPC), defined as the ideal creatinine value of the patient, assuming a normal glomerular filtration rate (GFR) of 75ml/min/1.73m2, and assigning a theoretical normal BPC for each age, sex and ethnic group.
All the patients were evaluated by means of the RIFLE and AKIN systems (Tables 1 and 2). As established by consensus, compliance with one or more of the urinary (U) and creatinine criteria (C) determined the diagnosis of ARF (ARF-UC). In addition, both criteria were evaluated separately.
Acute renal failure according to urinary criterion (ARF-U)Based on CHD, we identified the cases that met the U criterion before the C criterion, during a continuous period of 6, 12 and 24 hours. In this way the patients were simultaneously stratified according to RIFLE and AKIN every hour and during the 7 days of study into one of the four possible grades. For RIFLE: RIFLE zero (without ARF), R (risk), I (injury) and F (failure). For AKIN: AKIN 0, AKIN 1, AKIN 2 and AKIN 3. Based on these hourly results referred to RIFLE and AKIN, the program detected the most severe grade of ARF for each day of study, with the obtainment of a daily stratification of ARF only according to the U criterion as established by RIFLE and AKIN.
Acute renal failure according to creatinine criterion (ARF-C)Based on the MPC and BPC registries, we identified those cases that first met the C criterion before the U criterion, on a daily basis. In the case of the RIFLE system, we considered the daily increments in MPC with respect to BPC, stratifying the patients only according to the C criterion. For RIFLE: zero, R, I and F. For AKIN we considered the increases in MPC with respect to MPC in the previous 48h. Accordingly, the registry of ARF was only obtained on days 3, 5 and 7 of the study, yielding one of the four possible grades: AKIN zero, AKIN 1, AKIN 2 and AKIN 3.
Acute renal failure according to both criteria (ARF-UC)The patients meeting the U and C criteria simultaneously were identified and stratified into four possible ARF levels referred to both the RIFLE and the AKIN classification.
Neither volemia nor prior fluid therapy was considered.
The analysis of the selected variables was made using a program that generated an SQL database with the collected registries. The database in turn was processed using the Statistical Package for the Social Sciences (SPSS).
The homogeneity of the variables was controlled using the Levene test. The Student t-test for the comparison of means was used to detect significant differences between the participating institutions. In the case of patient sex, we assessed differences in the proportion of females between institutions based on the chi-squared test. A 95% confidence level was considered for all the statistical tests.
ResultsSample characteristicsThe mean values of the different characteristics of the global study sample (n=627) were: age 62 years (range 18–97); 63% males and 37% females; BMI 26.4kg/m2 (range 12.4–70.3); days of stay 13.6; APACHE score 15; SOFA score 5; 27.6% postsurgery cases (elective surgery 16.4%; emergency surgery 11.2%).
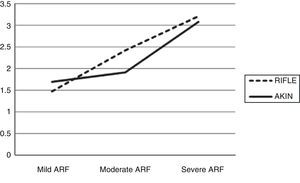
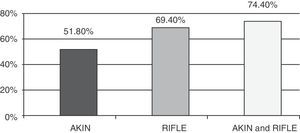
Incidence of acute renal failureA total of 69.4% and 51.8% of the patients presented some grade of ARF according to the RIFLE and AKIN classification, respectively (Fig. 1).
Most of the patients with ARF presented the mildest grade of renal failure (RIFLE R: 30.6% and AKIN 1: 31.1%), though RIFLE detected a larger number of patients with intermediate and severe grade ARF (26.6% and 12.1%, respectively) than AKIN (14.7% and 6.1%, respectively).
A total of 8.7% of the patients classified as presenting ARF according to RIFLE did not have ARF according to AKIN, while 9.8% of the patients with ARF according to AKIN did not have ARF according to RIFLE. On the other hand, a larger number of cases of ARF were detected on applying both classifications jointly (467 patients) than on applying only RIFLE (435 patients) or only AKIN (325 patients) (Fig. 1).
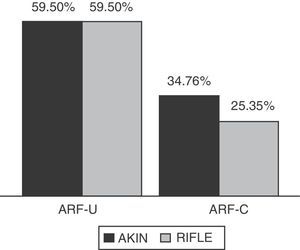
On examining the data only according to the U criterion, the results were seen to be the same for RIFLE and AKIN, since both systems had identical cutoff points in the consensus. A total of 59.5% of the cases of ARF complied with the U criterion before they complied with the C criterion, exhibiting no significant differences versus compliance with both criteria simultaneously. In contrast, the cases of ARF that first complied with the C criterion were fewer in number than the cases that complied with both criteria simultaneously: 34.7% for RIFLE and 25.3% for AKIN (Fig. 2).
There were no significant differences regarding the days of stay in the ICU (mean 14 days) between the patients with and without ARF, as evaluated by both the RIFLE and the AKIN classification.
The patients with ARF according to RIFLE were significantly older than those without ARF according to RIFLE. Moreover, older age was associated to increased severity. A similar tendency was observed in the patients evaluated with the AKIN system, though in this case the values failed to reach statistical significance. Neither classification showed significant differences in the incidence of ARF with respect to patient sex; however, on only evaluating the U criterion, the proportion of males was seen to increase with increasing severity of ARF, with both the RIFLE and the AKIN system. On the other hand, BMI was significantly greater (mean 27kg/m2) in the patients with ARF. The APACHE II and SOFA scores increased significantly with increasing severity of ARF, with both the RIFLE and the AKIN system. Most of the patients with ARF were non-surgical cases. Only 34 patients required RST (intermittent daily hemodialysis in 31 cases, and continuous RST in 3 cases), based on the following indications: anuria, acidosis, volume overload, refractory shock, progressive plasma creatinine elevation and hyperpotassemia.
Daily diuresis among the patients without ARF was 2268ml/day with RIFLE and 2109ml/day in the case of AKIN. The corresponding values were lower in the patients with ARF, with significantly lesser values in situations of increasing severity. However, on evaluating the sensitivity of daily diuresis in detecting patients with ARF, the area under the receiver operating characteristic (ROC) curve was found to be 66.7% for RIFLE and 62.8% for AKIN, i.e., sensitivity was low. In turn, on evaluating the patients only with the U criterion, daily diuresis decreased significantly with increasing risk of ARF. Those patients without ARF presented a higher mean value (2177ml/day), which proved significant with respect to all grades of ARF.
The MPC of the patients without ARF according to the RIFLE classification was 0.77mg/dl, versus 1.01mg/dl in those without ARF according to the AKIN system. The MPC values were higher in the patients with ARF according to RIFLE, and increased significantly with increasing severity. The correlation between MPC and the presence of ARF and its severity was not observed in the patients stratified according to the AKIN system. On the other hand, MPC among the patients evaluated only according to the U criterion was also significantly higher in the more severe cases. However, on evaluating the sensitivity of MPC in detecting ARF, the area of the ROC curve for RIFLE was 75.5%, versus 59.9% in the case of AKIN.
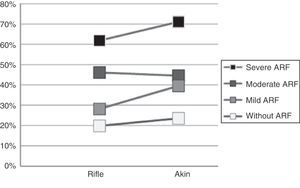
MortalityGlobal mortality (mortality in the ICU and up to 90 days after discharge) was 40.9% and 44.6% among the patients with ARF according to the RIFLE and ARF classification, respectively, and was significantly higher than among the patients without ARF (19.79% and 23.5% according to RIFLE and AKIN, respectively). These values were similar to those obtained when the diagnosis of ARF was established based only on the C criterion (ARF-C: 49.08% and 51.7% according to RIFLE and AKIN, respectively) or only on the U criterion (ARF-U: 41.82% according to both RIFLE and AKIN). The proportion of deaths increased significantly with increasing severity of ARF (Fig. 3). The most severe grade of ARF was associated to markedly higher mortality rates (71.1% and 61.8% according to AKIN and RIFLE, respectively).
According to the AKIN classification, the mortality rate of the most severe grade of ARF was significantly higher than in the case of mild or moderate ARF. In the case of the RIFLE system, the mortality rates corresponding to moderate and severe ARF were considerably higher than in the case of mild ARF or patients without ARF. The largest proportion of deaths was recorded in the ICU, in both the patients without ARF and in those of ARF of any grade of severity.
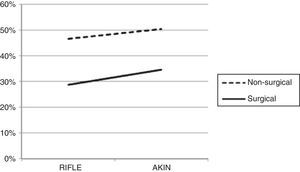
The mortality rate was higher in subjects with non-surgical conditions (46.56% and 50.40%, respectively) than in surgical cases (28.69% and 34.56%, respectively) among the patients with ARF according to both the RIFLE and the AKIN classification (Fig. 4).
The mortality relative risk increased progressively with increasing severity of ARF among the patients stratified according to both the RIFLE and the AKIN classification (Fig. 5).
DiscussionAccording to our results, the incidence of ARF was greater than in the large studies published in the literature, on applying both the RIFLE system and the AKIN classification (Table 2). This increased incidence was observed for all grades of severity.
Incidence of acute renal failure according to the literature.
| No. of patients | Urinary criterion | RIFLE total (%) | RIFLE R (%) | RIFLE I (%) | RIFLE F (%) | AKIN total (%) | AKIN 1 (%) | AKIN 2 (%) | AKIN 3 (%) | |
| Bagshaw | 120,123 | Yes, 24h | 36.10 | 16.20 | 13.60 | 6.30 | 37.10 | 18.10 | 10.10 | 8.90 |
| Johannidis | 6784 | Yes, 24h | 35.50 | 7.60 | 11.10 | 16.80 | 28.50 | 7.40 | 7.20 | 13.80 |
| Osterman et al. | 22,303 | No | – | – | – | – | 35.40 | 19.10 | 3.80 | 12.50 |
| Our data | 627 | Yes, hourly | 69.40 | 44.20 | 38.30 | 17.50 | 51.80 | 28.30 | 28.30 | 11.70 |
The RIFLE system classified a larger number of patients with ARF than the AKIN classification, in contrast to the observations of Brochard.10 The difference in the incidence of ARF according to RIFLE and AKIN was circumscribed to the intermediate and severe cases of ARF, since the proportion of patients with mild ARF was similar according to both RIFLE and AKIN. On the other hand, there were patients classified as having ARF according to the RIFLE system but not according to the AKIN classification, and vice versa. This suggested that the use of both systems would increase the capacity to detect ARF, as was effectively confirmed by the results obtained.
On comparing the RIFLE and AKIN classifications, the differences can only be attributed to the C criterion, since the U criterion has the same cutoff points in both systems. The weaknesses of using plasma creatinine for the diagnosis of ARF have been widely commented in the literature. In the case of the RIFLE system, the C criterion is based on comparison of the actual MPC of the patient with the BPC intended to represent “ideal creatinine”, and is estimated according to the MDRD formula. The latter has been validated only in patients who are stable (an uncommon circumstance in the critically ill), and ignores the nonlinear relationship between the creatinine levels and the glomerular filtration rate (GFR). Moreover, this formula includes information which is not usually reliable in the ICU: the patient weight is often not known or is altered as a consequence of losses or increments in body water, in the same way as the creatinine distribution volume. On the other hand, the formula also contemplates an arbitrary “normal” estimated GFR of 75ml/min/m2, when in fact this value may differ widely among normal individuals with different dietetic habits or with different renal functional reserves.3,12 The MDRD formula likewise does not take into account the changes in MPC due to non-renal causes, as in patients with diminished muscle mass or impaired liver function. All these factors question the usefulness of BPC in the RIFLE classification. In the case of the AKIN system, comparison is made of the actual MPC with the MPC value of the previous 48h. Here the previous creatinine value is not calculated but measured–suggesting that the results could be more reliable than in the case of the RIFLE system. However, a patient may have an already elevated previous MPC if ARF developed days before determination of the value, and consequently comparison of the two MPC values would be unable to detect ARF. Thus, analysis of the changes in creatinine is questioned in both methods, and discussion focuses on which of the two is more reliable. Since there is no gold standard for defining ARF, the specificity of the two methods cannot be compared. However, as suggested by Bellomo in 2004,3 the importance of the definition of ARF does not seem to center on whether it is “correct” or “reliable”, but on its usefulness. We thus consider that the most useful method should be that capable of detecting a larger number of cases of ARF with the purpose of adopting preventive or early management measures, despite the consequent incidence of false-positive results.
If we assume that the most useful method is that able to detect a larger number of patients with ARF, then the RIFLE system would be more useful than the AKIN classification. In turn, the use of RIFLE and AKIN simultaneously in one same patient would prove more useful than RIFLE alone.
In our study, the U criterion detected a larger number of patients with ARF than the C criterion, and was therefore more effective. This increased sensitivity of the U criterion could be explained by the fact that we stratified the patients in an hourly manner (according to a calculated hourly diuresis), in contrast to creatinine, which requires a new value after 24h in the case of the RIFLE system or after 48h in the AKIN classification.
In our experience there was great variation in the way of monitoring diuresis in the different participating centers, and the literature likewise describes a lack of uniformity in the way this parameter is determined. On the other hand, when the urinary tract is not catheterized it is not possible to record the urine produced every hour–theoretically making it impossible to apply the U criterion recommended by consensus in such patients who, although perhaps in a less critical condition, are not free from risk of developing ARF. For these reasons we decided to implement calculated hourly diuresis (CHD), making it possible to apply the RIFLE and AKIN systems with greater precision and obtain comparable results in all patients, i.e., with or without urinary catheterization.
Since diuresis was evaluated in ml/day, the sensitivity in diagnosing ARF was 66.7% and 62.8% in relation to RIFLE and AKIN, respectively; in other words, daily diuresis as an isolated value is of scant diagnostic utility. However, the decrease in hourly urine output showed a good correlation to the presence of ARF and to more severe grades of the disease. The diuresis/time ratio therefore could be regarded as having prognostic value.
The increase in the values of MPC among the patients with ARF was not correlated to progressing severity of ARF when using the AKIN system, though a correlation was observed in the case of the RIFLE classification. Here we must remember that the creatinine data were registered daily in the RIFLE system versus once every 48h in the AKIN system; as a result, we can assume that increases in MPC have prognostic value when creatinine is measured at least once every 24h. On the other hand, the isolated MPC values showed a sensitivity of 75.5% and 59.9% in relation to RIFLE and AKIN, respectively, i.e., their diagnostic value is poor.
In coincidence with the published data, our mortality rates were significantly higher among the patients with ARF than in the patients without ARF, on applying both the RIFLE and the AKIN classification–higher rates being associated to increased severity of the disease. The results were similar on stratifying the patients according to the U criterion or C criterion separately. The larger proportion of deaths recorded among non-surgical patients is also consistent with the findings in the literature.
In agreement with the observations of other authors, our data showed patients with ARF to be older, with a larger number of previous disease conditions, and with higher BMI values and APACHE II and SOFA scores than patients without ARF. There were no significant differences with respect to patient sex or days of stay in the ICU. Furthermore, we found the highest incidence of ARF to correspond to non-surgical patients.
ConclusionsSince there is no gold standard for knowing the true sensitivity and specificity of the RIFLE and AKIN systems, comparative assessment should aim to establish which of the two systems is more useful for improving the outcome in critically ill patients.
The literature continues to present data that are difficult to compare, despite the consensus-based definitions. Perhaps the incidences of ARF reported in the literature would have been greater if strict application of the U criterion had been observed.
Despite the recommendations, it remains unclear how diuresis should be measured, particularly in patients without catheterization of the urinary tract. In our experience, CHD allowed application of the urinary criterion in a standardized manner in all patients, independently of the diuresis monitoring intervals and the presence or absence of a bladder catheter. We therefore recommend its use in this context.
We feel the originality of our study to be fundamentally attributable to the fact of having applied the U criterion exactly as recommended by consensus, in contrast to most studies in which insufficient or absent diuresis information constituted an acknowledged weak point.
Conflicts of interestThe authors declare that they have no conflicts of interest.
Please cite this article as: Salgado G, Landa M, Masevicius D, Gianassi S, San-Román JE, Silva L, et al. Insuficiencia renal aguda según RIFLE y AKIN: estudio multicéntrico. Med Intensiva. 2014;38:271–277.