Alveolar recruitment in acute respiratory distress syndrome (ARDS) is defined as the penetration of gas into previously unventilated areas or poorly ventilated areas. Alveolar recruitment during recruitment maneuvering (RM) depends on the duration of the maneuver, the recruitable lung tissue, and the balance between the recruitment of collapsed areas and over-insufflation of the ventilated areas. Alveolar recruitment is estimated using computed tomography of the lung and, at the patient bedside, through assessment of the recruited volume using pressure-volume curves and assessing lung morphology with pulmonary ultrasound and/or impedance tomography. The scientific evidence on RM in patients with ARDS remains subject to controversy. Randomized studies on ARDS have shown no benefit or have even reflected an increase in mortality. The routine use of RM is therefore not recommended.
Reclutamiento alveolar en el síndrome de distrés respiratorio agudo (SDRA) se define como la entrada de gas en zonas previamente no ventiladas o en zonas pobremente ventiladas. El reclutamiento alveolar durante una maniobra de reclutamiento (MR) dependerá de la duración de la maniobra, del tejido pulmonar reclutable, del balance entre reclutamiento de áreas colapsadas y sobredistensión de las áreas ventiladas. La estimación del reclutamiento alveolar se realiza con la tomografía computarizada de tórax y, a pie de cama, con la construcción de curvas de volumen y presión, la ecografía pulmonar y la tomografía por impedancia. La evidencia científica nos indica que la utilización de las MR en pacientes con SDRA sigue sujeta a controversia. Estudios aleatorizados del SDRA o bien no han demostrado beneficio o bien han revelado un incremento de la mortalidad y, por ello, no se recomienda su uso rutinario.
No universally accepted definition from either the anatomical/morphological perspective or the functional viewpoint has been established for alveolar recruitment in patients with acute respiratory distress syndrome (ARDS).1,2 This is due to the methodology used for the analysis and quantification of alveolar recruitment. The commonly accepted definition of recruitment is based on the pulmonary tomographic evaluation of gas penetration into previously unventilated areas of the lungs – including or not the penetration of gas into poorly ventilated zones.3,4 This evaluation is made in accordance with the modification of the radiological density range within the lungs. When using methods based on pulmonary mechanics or the dilution of inert gases, recruitment takes into account both the gas that has penetrated into previously unventilated zones and the gas that has penetrated into partially ventilated zones.4,5
Types of recruitment maneuversAn alveolar recruitment maneuver (RM) consists of a transient increase in alveolar pressure to levels above those of protective ventilation. Alveolar recruitment during RM depends on a number of factors: the duration of the maneuver, the existence of recruitable lung tissue, the balance between recruitment of collapsed areas and overdistension of ventilated areas, the hemodynamic response during the maneuver (which largely determine its tolerance) and the positive end-expiratory pressure (PEEP) required after RM. This PEEP level after RM is usually adjusted according to the increase in pulmonary compliance or a sustained increase in oxygenation.6–9 Many alveolar recruitment procedures have been described, of which two are the most widely used6,10,11:
- -
Application of CPAP between 30–40 cmH2O during a period of 30–40 s.
- -
Pressure control ventilation and the elevation of PEEP to limits of 30–40 cmH2O with peak pressures no higher than 50–60 cmH2O.
Maneuvers with sustained CPAP produce more marked reductions of cardiac output and arterial pressure than pressure control ventilation recruitment maneuvering – probably because the latter affords a limited and intermittent peak inspiratory pressure within the airway, which allows venous return, in contrast to the constant pressure of maneuvering with CPAP.6,12 To date, no studies have compared the incidence of barotrauma or the impact upon mortality according to the type of recruitment maneuver used.
The degree of hemodynamic impairment produced by RM is largely dependent upon the volemia level at the time of the maneuver. Experimental studies have shown that the hemodynamic effects of RM can be enhanced by hypovolemia – the main underlying mechanism being the drop in venous return and ventricular filling. Asystolia may result in extreme cases. In normovolemic situations, the increase in right ventricle afterload due to the elevation of intrathoracic pressure is the main cause of lowered cardiac output.12–15
Estimation of recruitmentImaging and lung mechanical studies show that alveolar recruitment takes place from the start of insufflation to the end of the latter.16 Thus, a fundamental characteristic of recruitment is that it occurs during inspiration. In this regard, positive end-expiratory pressure (PEEP) per se does not give rise to recruitment, but rather avoids derecruitment and expiratory alveolar collapse.1,2
Consequently, the magnitude of recruitment will depend on the end-inspiratory pressure, and for the same PEEP levels, the recruitment observed in patients with acute lung injury and ventilated with low circulating volumes (6 ml/kg) is less than that observed at higher circulating volumes (10 ml/kg).17 However, when patients are ventilated with an airway plateau pressure of about 30 cmH2O, the combination of elevated PEEP with low circulating volume generates greater recruitment than the combination of high circulating volume and lower PEEP. These findings evidence the importance of avoiding derecruitment following any alveolar recruitment maneuver.17
Different methods have been developed to assess the degree of alveolar recruitment. Some of them are based on the plotting of volume and pressure curves, where the PEEP level is modified and an estimation is made of the gain between the increase or decrease in total expired gas volume between two PEEP points. On constructing these two points, any modification of the PEEP level will result in an increase or decrease in expired gas volume: if the latter is greater than expected (determined by compliance and the pressure gradient), recruitment will have taken place.17,18 This principle is also applicable to the gas dilution methods, where evaluation is made of the concentration of inert gases (usually helium or nitrogen), with calculation at different PEEP levels of the greater or lesser dilution of the gas – corresponding to greater or lesser lung volume.4,6
Thoracic computed tomography is the imaging technique traditionally used to estimate alveolar recruitment, and may be regarded as the gold standard in this regard. The technique analyzes the radiological densities of the lung tissue from the images obtained. Density is expressed in Hounsfield units (HU), and ranges from +100 to −1000. Thus, and depending on the authors,3,4 unventilated zones are considered to present between +100 and −100 HU, poorly ventilated zones between −100 and −500 HU, well ventilated zones between −500 and −900 HU, and hyperinsufflated zones between −900 and −1000 HU. Based on the respective densities, calculation is made of the volume of gas in each of the zones and the changes induced by PEEP and/or the circulating volume, thus providing an estimation of recruitment.
More recently, the estimation of alveolar recruitment has been made on a point-of-care and noninvasive basis using imaging techniques simpler than thoracic computed tomography. These techniques include lung ultrasound and electrical impedance tomography.19,20 In expert hands, different lung ultrasound indices have shown good correlation to alveolar recruitment estimated from thoracic computed tomography.21,22 Lastly, electrical impedance tomography allows us to estimate not only alveolar recruitment but also the hyperinsufflation induced by ventilation. Accordingly, it may be a useful tool for individualizing the ventilatory parameters.23,24
Oxygenation is the most widely used method for evaluating the response to alveolar recruitment. The simplest methods for assessing the response to recruitment with oxygenation are those used in the ART study and in the ALVEOLI trial. In the ART study, the criterion for determining the response to recruitment was a change in the PaO2/FiO2 ratio of >50 mmHg, and the method used was the gradual increase in PEEP level with an inspiratory pressure of 15 cmH2O.15 In the ALVEOLI study, the criterion for determining the response to alveolar recruitment was an increase of between 5–9% in SaO2 following CPAP 40 cmH2O during 40 s.25
Recruitment maneuvering in neurocritical patientsLung–brain interaction is one of the main challenges in the management of neurocritical patients, where it has been shown that hypoventilation and hypoxemia increase cerebral blood flow, resulting in an increased risk of brain edema and intracranial hypertension. Acute respiratory distress syndrome has been associated to high morbidity-mortality in neurocritical patients; alveolar RM is therefore of considerable interest in the management of these individuals.26–28
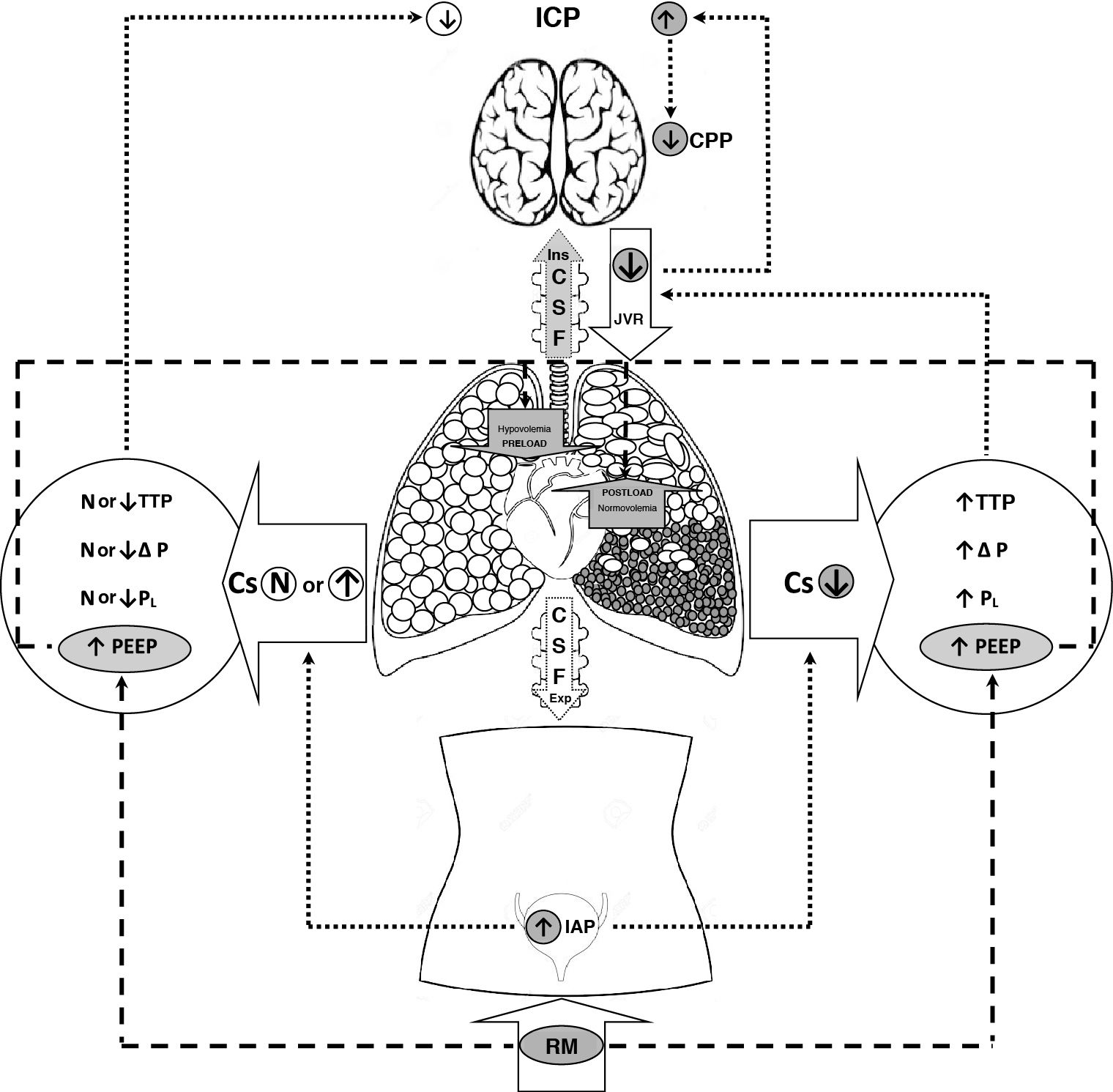
The benefits of protective ventilation have been well established, in the same way as the benefits of measures such as prone decubitus. Recruitment maneuvers and the use of high PEEP levels have been prescribed to improve oxygenation in patients with refractory acute respiratory failure. However, due to the increase in intrathoracic pressure and the consequent decrease in venous return, these measures may cause deleterious effects such as an increase in intracranial pressure (ICP) and a decrease in cerebral perfusion pressure (CPP).27,29,30Fig. 1 describes the different interactions between intracranial, intraabdominal and intrathoracic pressure.
Multicompartment system of intraabdominal, intrathoracic and intracranial pressure interaction. The increase in IAP and TTP (RM) with low Cs, and its repercussion upon the intrapulmonary pressures, result in an ascending LCR flow during inspiration and difficult JVR, with the consequent increase in ICP. On the other hand, the increase in PEEP (RM), according to volemia status, may result in a decrease in cardiac preload and an increase in right ventricle afterload.
Abbreviations: Cs: pulmonary compliance, TTP: transthoracic pressure, ΔP: driving pressure, PL: transpulmonary pressure, IAP: intraabdominal pressure, PEEP: positive end-expiratory pressure, CSF: cerebrospinal fluid, JVR: jugular venous return, CPP: cerebral perfusion pressure, ICP: intracranial pressure, RM: recruitment maneuver.
Recruitment maneuvering in neurocritical patients is subject to controversy.31 Wolf et al.,32 Pulitano et al.,26 and McGuire et al.33 documented the safety of high PEEP in patients with brain damage, showing that the ICP increments secondary to an increase in PEEP were not clinically significant. Nermer et al.34 likewise documented the safety of RM based on the increase in inspiratory levels over PEEP levels of 15 cmH2O, with the aim of improving oxygenation; their study evidenced no significant changes in ICP or CPP. Borsellino et al.,29 in a systematic review, observed great variability among the published studies, and concluded that there are no scientific reasons for not performing RM in patients with acute brain damage, provided brain perfusion and hemodynamics can be monitored. Lastly, the association between the variations in PEEP and their effect upon ICP is related to the respiratory system mechanics.26,35
In sum, RM based on an increase in inspiratory pressure in neurocritical patients has been shown to improve oxygenation. However, due to the risk of secondary brain damage, such measures should only be adopted under strict monitoring of brain perfusion and hemodynamics – placing priority on the safety of the patient neurological condition, and individualizing each case.
Scientific evidenceThe use of RM in patients with ARDS remains subject to controversy. The latest randomized studies on the utilization of RM have unanimously demonstrated an increase in oxygenation, though without improvements in terms of mortality8,36–38 or with an increase in mortality in the group subjected to the optimization of PEEP following alveolar RM.15 It is therefore considered that RM should not be used on a generalized basis in patients with ARDS.2,39,40 Recently, Papazian et al.41 personalized mechanical ventilation (MV) in ARDS according to the radiological morphology of lung damage. The patients randomized to the control group received a tidal volume (TV) of 6 ml/kg and a PEEP level according to a FiO2/PEEP table, and were placed in early prone decubitus, while the personalized group was treated according to the morphology of the lung injury. The patients with focal lung injury received a TV of 8 ml/kg and PEEP between 5–9 cmH2O, and were placed in early prone decubitus. The patients with diffuse lesions received a TV of 6 ml/kg, PEEP to reach an end-inspiratory pressure of 30 cmH2O, and RM. There were no differences in mortality between the control group and the personalized treatment group, though 21% of the patients were wrongly classified due to incorrect identification of the lung injury as being either focal or diffuse. A relevant finding of this study was greater survival in the correctly classified personalized treatment cases and greater mortality in the wrongly classified personalized treatment cases. The study published by Constantin et al.41 evidences the difficult of providing individualized MV in patients with ARDS. Recruitment maneuvering applied to patients with focal ARDS may prove deleterious, since it can induce overpressure phenomena and deformation in aerated lung zones, redistribution of pulmonary circulation towards unventilated zones with an increase in pulmonary shunting, and elevation of the pulmonary vascular resistances and right ventricle afterload – all these phenomena being known to be able to increase the damage already established by ARDS itself.7,12,15,42
ConclusionsInvasive ventilatory support in ARDS should be based on the evidence of a protective TV with early prone decubitus, and on the individualization of PEEP and other adjuvant treatments according to the etiology of ARDS and the morphology of the lung injury.39,40 Alveolar RM has been used as a rescue strategy in situations of refractory hypoxemia, and its application requires good knowledge of respiratory pathophysiology and precise assessment of the impact of these maneuvers upon organs at a distance from the lungs – particularly the cardiovascular system. In sum, RM is a risky intervention when not performed on an individualized basis, and when the response to maneuvering is not adequately monitored.
Financial supportThe present study has received partial funding from CIBER Enfermedades Respiratorias (ISCiii, Madrid, Spain).
Contribution of the authorsAll the authors of the VentiBarna group have contributed to the prior discussions on the orientation of the manuscript and its drafting.
Conflicts of interestThe authors of the VentiBarna Group declare that they have no personal or financial conflicts of interest in relation to the present study.
Please cite this article as: Lomeli M, Dominguez Cenzano L, Torres L, Chavarría U, Poblano M, Tendillo F, et al. Reclutamiento alveolar agresivo en el SDRA: más sombras que luces. Med Intensiva. 2021;45:431–436.