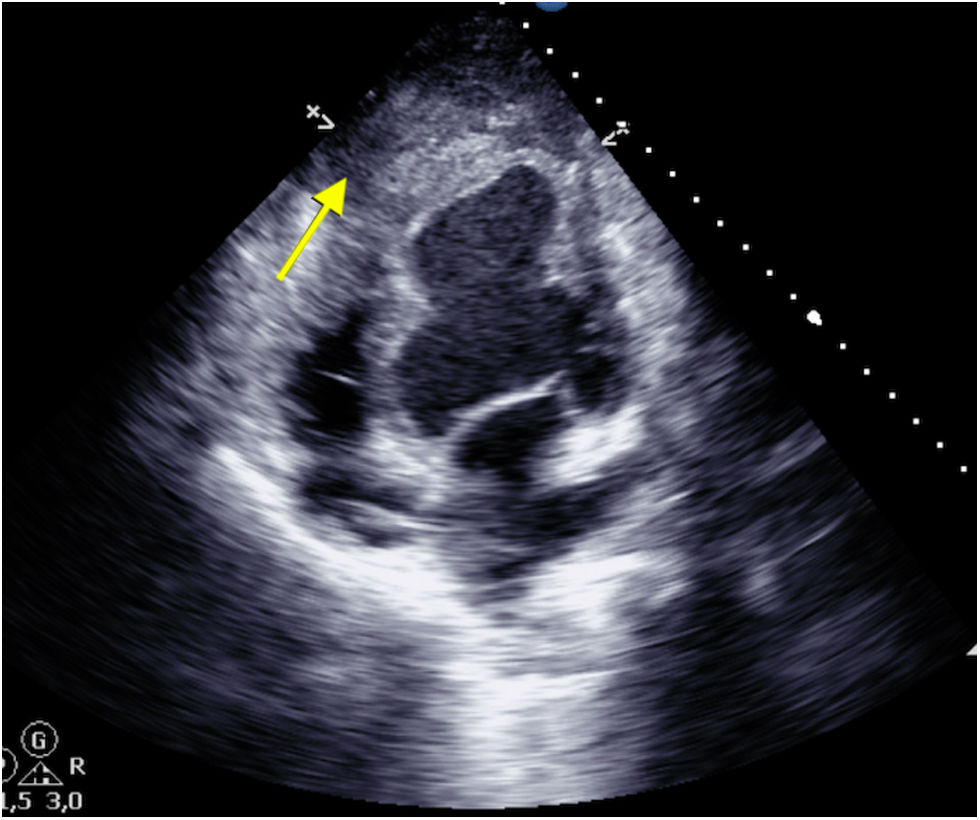
A 49-year-old male was admitted with a SCAI D cardiogenic shock following a 12-day history of non-ST-elevation acute coronary syndrome, not revascularized in his country of origin, complicated by intramyocardial dissection, resulting in a contained apical posterior hematoma (Fig. 1, yellow arrow), hemodynamic instability, and severe biventricular dysfunction requiring veno-Arterial extracorporeal membrane oxygenation (ECMO) as a bridge therapy to heart transplantation.
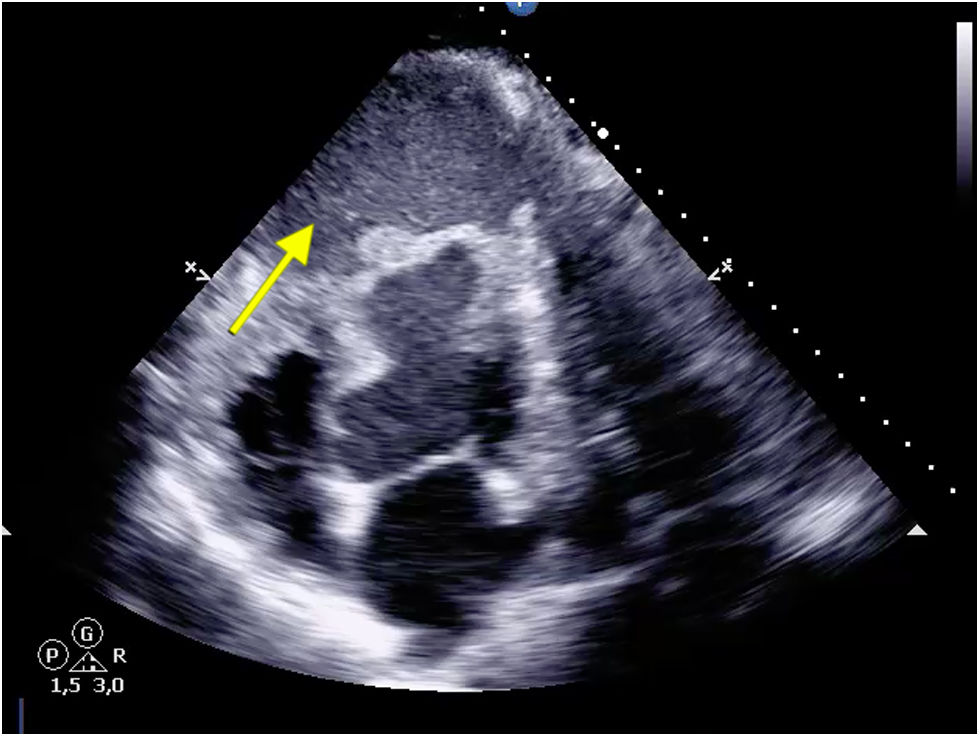
After 1 week on the urgent 0A waiting list, hemodynamic instability required an increase in pharmacological support, with transthoracic ultrasound revealing the rupture of the contained apical hematoma (Fig. 2, yellow arrow). Given the presence of refractory hemorrhagic shock despite measures, emergency surgery was scheduled to control the bleeding. However, coincidentally, a compatible organ became available for our patient, and a heart transplant was ultimately performed.
Ethical considerationsAll guidelines for publication in the journal have been followed.
Declaration of Generative AI and AI-assisted technologies in the writing processNo artificial intelligence tools were used in the generation of figures or in the drafting or refinement of the text.
FundingWe have not received any funding for this work or this document.