Early mobilization strategies in the intensive care unit may result in the prevention and reduction of polyneuromyopathy in the critical patient, improved quality of life, shortened ICU and hospital stay, and lesser mortality during hospitalization. However, it is well known that factors such as the protocol used, the population included in the studies, the timing of the strategy, the severity of the patients and different barriers directly influence the outcomes. This study examines the main protocols described in the literature and their associated results. The main techniques used were kinesitherapy, transfer and locomotion training, as well as neuromuscular electrical stimulation and cycle ergometry. Although two trials and a meta-analysis found no positive results with mobilization, programs that focus on specific populations, such as patients with weakness due to immobility and with preserved neuromuscular excitability can derive more positive effects from such treatment.
Las estrategias de movilización precoz en la unidad de cuidados intensivos pueden asociarse a la prevención y una reducción de la polineuromipatía del paciente crítico, una mejora de la calidad de vida del paciente y la reducción tanto del período de ingreso en la UCI y el hospital como de la mortalidad durante la hospitalización. Sin embargo, se sabe que los resultados se ven afectados por factores como el protocolo utilizado, la población incluida en los estudios, el momento en que se comienza a aplicar la estrategia, la gravedad de los pacientes y distintos tipos de barreras. Este estudio informa sobre los principales protocolos empleados en la literatura científica, así como sus resultados. Las principales técnicas empleadas fueron la quinesioterapia, la formación sobre traslados y locomoción, la estimulación neuromuscular eléctrica y el uso de bicicletas ergométricas. Si bien en dos ensayos y un metaanálisis no se han observado resultados positivos con la movilización, los programas que se centran en poblaciones objetivo específicas, como aquellas formadas por pacientes con debilidad debido a la inmovilidad y excitabilidad neuromuscular preservada, pueden lograr resultados más positivos con el tratamiento.
Interventions in early mobilization are beneficial for patients with critical illness because they reduce muscle weakness acquired in the intensive care unit (ICU). Adequate knowledge of the population that is at risk of developing muscular disorders is extremely important, and the two main evident risks are mechanical ventilation for extended periods and immobility.1 Thus, it is clear that there is a need for the physiotherapy team to evaluate the possible risks of deleterious effects related to mechanical ventilation and immobility of critically ill patients at the ICU, such as loss of strength and muscle mass.
The main changes experienced by critical patients with muscle weakness at cellular and molecular level are reduced excitability of the muscle membrane, altering the link between protein production and degradation resulting in increased protein degradation, increased free radicals and decreased antioxidant defense plus oxidative stress, which results in an increased inflammatory status seen by raising further the interleukins and possible mechanisms involving growth and differentiation factor 15 (GDF-15), transforming growth factor-β (TGF-β).2–4
Unfortunately, molecular mechanisms underlying the muscle atrophy of intensive care unit-acquired weakness (ICUAW) are poorly understood. Jiroutková et al.5 hypothesized that bioenergetics failure of skeletal muscle may contribute to the development of ICU-acquired weakness and conducted a study with the aim to determine whether mitochondrial dysfunction persists until the protracted phase of critical illness. The authors demonstrated that mitochondrial dysfunction in the quadriceps muscle of patients with protracted critical illness compared to metabolically healthy age-matched control patients undergoing hip replacement surgery. There was approximately 50% reduction in the capacity for aerobic ATP synthesis per milligram of muscle wet weight, in correlation with significant reductions in functional subunits of complexes III and IV.
When accounting for the activity of citrate synthase, which we used as a marker of mitochondrial content, there was no difference in global mitochondrial functional indices. Bloch et al. investigated GDF-15 and microRNA expression in patients with ICUAW and to elucidate possible mechanisms by which they cause in vivo and in vitro muscle atrophy and shows that GDF-15 may increase sensitivity to TGF-β signaling by suppressing the expression of muscle microRNAs, thereby promoting muscle atrophy in ICUAW. This study identifies both GDF-15 and associated microRNA as potential therapeutic targets.6
In the literature is possible to find different early mobilization protocols presenting variations related to the progression of exercises and even their start time. Other tools have been incorporated into the early mobilization protocols such as neuromuscular electrical stimulation (NMES), the cycle ergometer, and the orthostatic board. According to Conolly et al.,7 early mobilization and electrostimulation are presented as the most effective alternatives for short-term outcomes.8–10 Interestingly, Stefanou et al.11 proposed a study for exploring the NMES-induced effects on mobilization of endothelial progenitor cells (EPCs) in septic ICU patients. Patients were randomized to one of the two 30-min NMES protocols of different characteristics, a high-frequency (75Hz, 6s on – 21s off), or medium-frequency (45Hz, 5s on – 12s off) protocol both applied at maximally tolerated intensity and blood was sampled before and immediately after the NMES sessions. The authors demonstrated that NMES acutely mobilized EPCs in severe ICU patients and these effects did not depend on NMES protocol or sepsis severity status.
The beneficial effects of the different early mobilization strategies are associated with the prevention and reduction of polyneuropathy and myopathy of the critical patient, improvement of the patients’ quality of life, reduction of ICU stay and hospitalization, and mortality during hospitalization. Other associated outcomes are the reduction of mechanical ventilation time and weaning, and the preservation of peripheral and respiratory muscle strength.
Even passive mobilization strategies demonstrate significant beneficial effects at cellular level, as demonstrated by Llano-Diez et al.,12 which evaluated the effects of a specific intervention aiming at reducing mechanical silencing in sedated and mechanically ventilated ICU patients. The authors evaluated muscle gene/protein expression, post-translational modifications, muscle membrane excitability, muscle mass measurements, and contractile properties at the single muscle fiber level were explored in seven deeply sedated and mechanically ventilated ICU patients subjected to unilateral passive mechanical loading for 10h per day and demonstrated triggering the myosin loss and muscle wasting. The higher neuronal nitric oxide synthase expression found in the ICU patients and its cytoplasmic translocation are regarded as a probable mechanism underlying these modifications. The positive effect of passive loading on muscle fiber function strongly supports the importance of early physical therapy and mobilization in deeply sedated and mechanically ventilated ICU patients.
An important factor to note is that when we evaluate the effectiveness of early mobilization strategies, it should be clear that the observed outcomes may be related to the protocol used, population included in the studies, strategy start time, severity of patients, and possible barriers faced along the process.13 Thus, it is reasonable that the use of early mobilization strategies and associated tools in the ICUs determine the short-term benefits with direct impact on hospital outcomes.
Assessment of muscle strengthMuscle strength is defined as the maximal force that can be generated by specific muscle group, being measured by isometric or dynamic means and expressed in kilograms or newtons.14 Volitional and non-volitional assessments of muscle strength are available. The Medical Research Council Sum Score (MRC-SS) involves assessment of three muscle groups of the upper limbs (shoulder abductors, elbow flexors and extensors of the wrist) and three of the lower limbs (hip flexors, knee extensors and ankle extensor), bilaterally, with your individual score ranging from 0 to 5, and a total between 0 and 60.15 The MRC-SS is currently recommended for the clinical diagnosis of ICU-AW (total score below 48).16 Two common techniques to measure MRC-SS can be adopted: isometric at one point of range and through-range of movement. The isometric technique is preferable, as it has a higher level of reliability and agreement to diagnose ICU-AW.17
The MRC-SS scale limits its sensitivity, particularly at the higher grades,4,5 which results in ceiling effects.18 Hough et al.19 found that MRC-SS could not be performed for most patients. Practical details of the scoring system concerning the adaptation of the original score for bedridden patients and use of rigorous criteria to define cooperation may be crucial to obtain reliable and reproducible results.20 Dynamometry has been recommended as an alternative to evaluate muscle strength in individuals at least antigravity strength, and has a great association with peripheral muscle strength global.21,22 Confirmation of dynapenia in the elderly can be obtained when the values of grip strength are less than 20kgf (in women) and 30kgf (in men), besides serving for the diagnosis of sarcopenia. ICU-acquired weakness when values are less than 7kgf (women) and 11kgf (men).23–25
The relationship between muscle strength and physical function measurements is no longer present. Conolly et al.26 have demonstrated that peripheral muscle strength is not directly related to physical function tests (Timed Up and Go test and Sit to Stand 5 test) at ICU discharge. Thus, it suggested that weakness is not the only wrongdoer limiting physical function. Other factors include static and dynamic balance, mental health, cognitive function and pain may influence in physical function outcomes.20 Further studies that investigate the main factors influencing the deterioration of physical function after critical illness must be developed to address this gap in literature.
Early mobilization protocolsThe use of systematic mobilization protocols is one of the strategies used by the multidisciplinary team to facilitate the progression of the gains in mobility along the hospitalization of patients, as well as to ensure greater safety in the care provided to patients.
The protocols do not generally follow a closed rule during their elaboration. Some only include information related to the motor aspect, while others consider factors such as cardiovascular and respiratory reserve that have an influence on the evolutionary process of early mobilization.
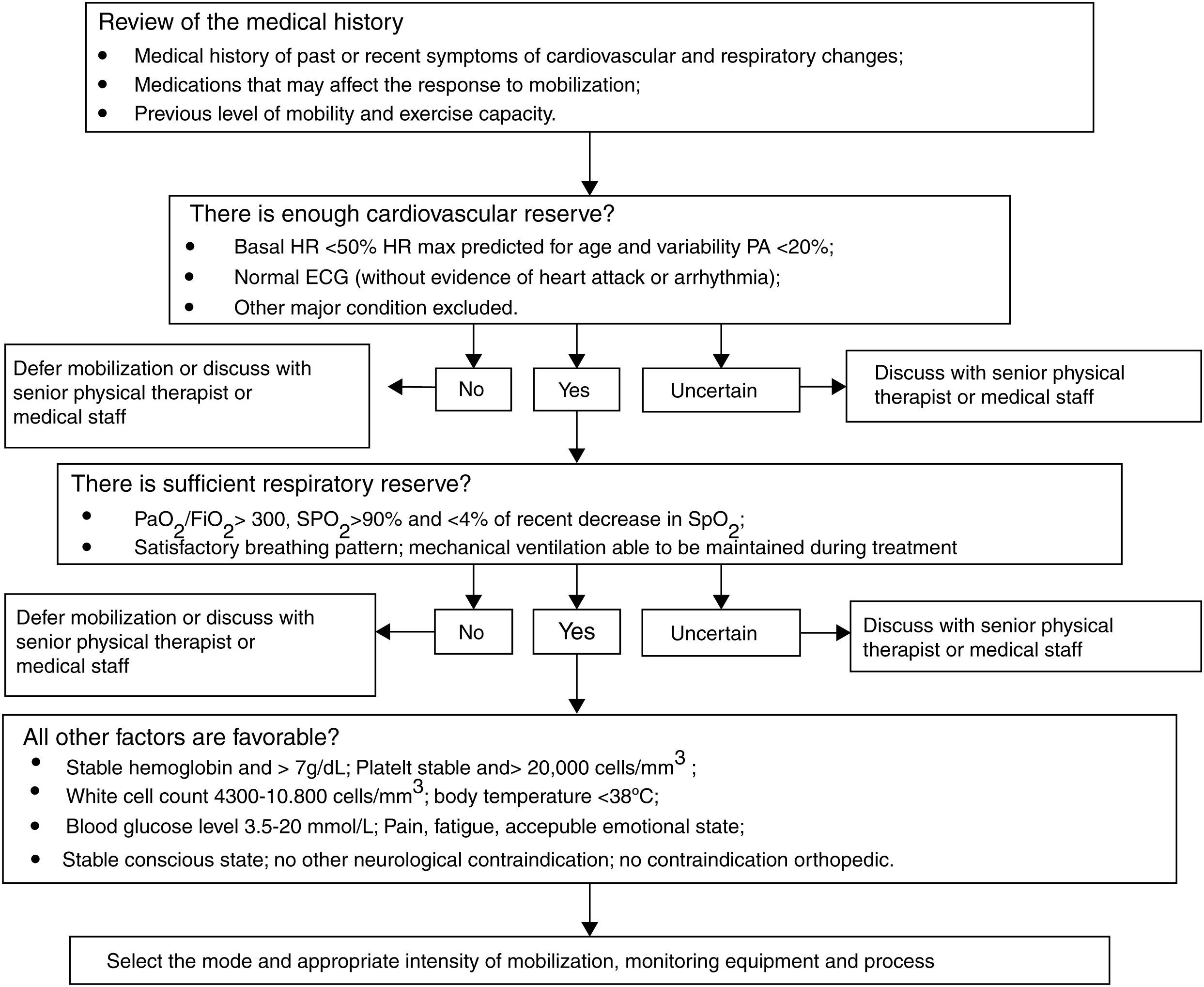
Kathy Stiller27 was one of the first authors to mention the importance of a systematic evaluation of the respiratory reserve followed by cardiovascular reserve and some clinical information. In her study she described physiological parameters considered safe in the institution of the various strategies to promote human movement. Fig. 1 shows the scheme used in this article.
Flowchart for the safety evaluation for mobilization.
The evaluation and understanding of the cardiovascular and respiratory function, as well as other reported factors, is of great importance since in many situations critical patients present an imbalance between the supply and consumption of oxygen. Thus, if prescribed and performed at the wrong time the mobilization of the critical patient may cause more harm than good.
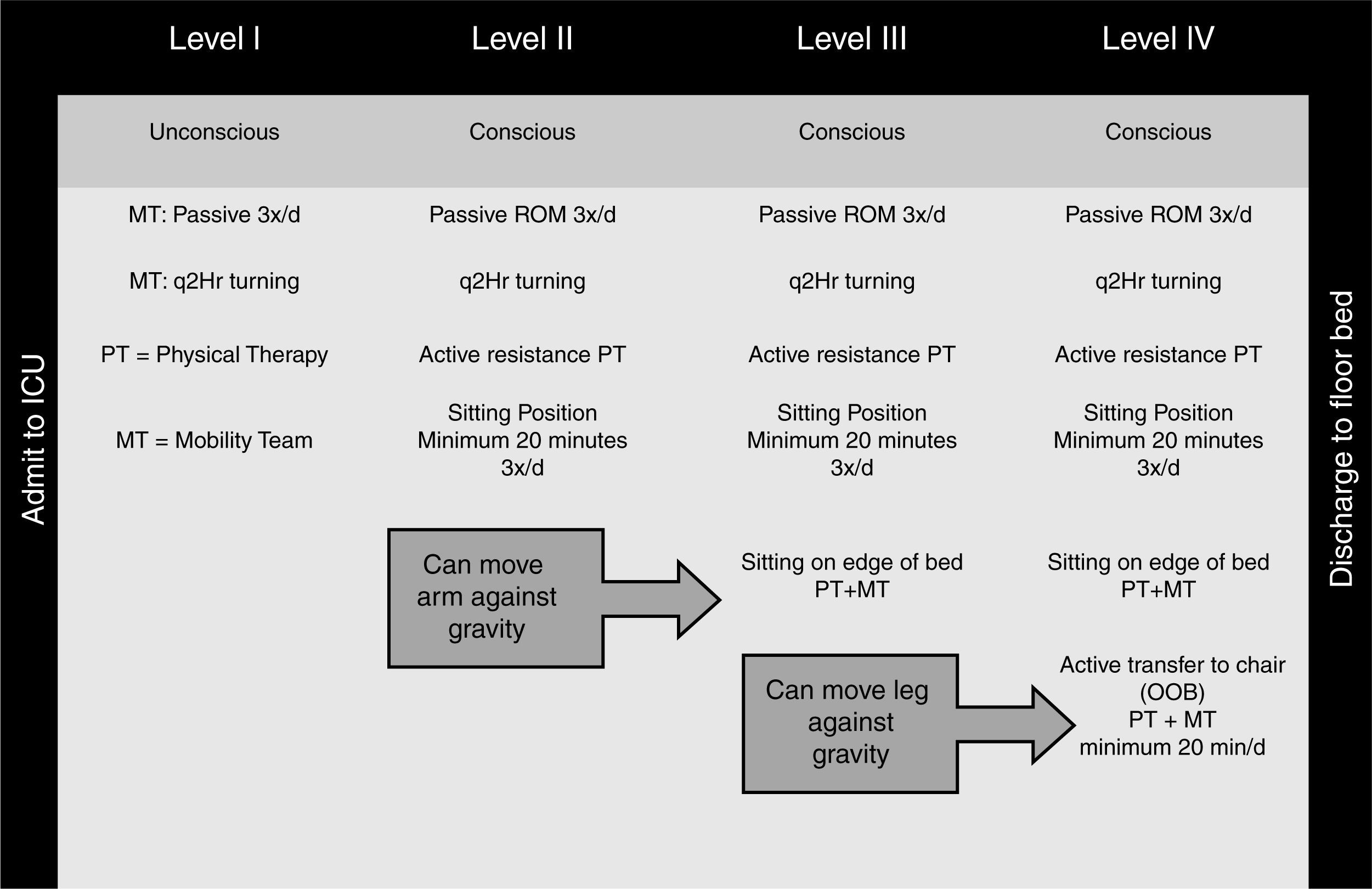
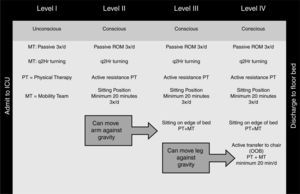
Morris et al.28 were the first to describe a protocol in which the main foundation was the progression of mobilization according to neurological function (conscious and unconscious), cardio respiratory stability and muscle strength in the arms and legs. The authors concluded that the execution of this protocol promoted a lower permanence in the intensive care unit than that of the control group, and there was no increase in associated costs (Fig. 2). Later, Schweickert et al.29 also tested the effects of mobilization in a randomized clinical trial and demonstrated a greater frequency of return to the previous functional independence state, shorter duration of delirium and more ventilator-free days. This study did not use a protocol divided in levels as the aforementioned one, and the progression of mobilization was based on the patient's level of awareness and participation during the mobilization associated to stability and tolerance criteria related to the cardio respiratory function. The mobilization techniques used in a progressive manner were: passive and active exercises in bed; mobility training in bed (sitting on edge of bed); transfer from bed to chair, and walking.
Early mobilization protocol for critically ill patients on mechanical. Ventilation. PROM – passive range of motion therapy; PT – physical therapy; ICU – intensive care unit; OOB – out of bed.
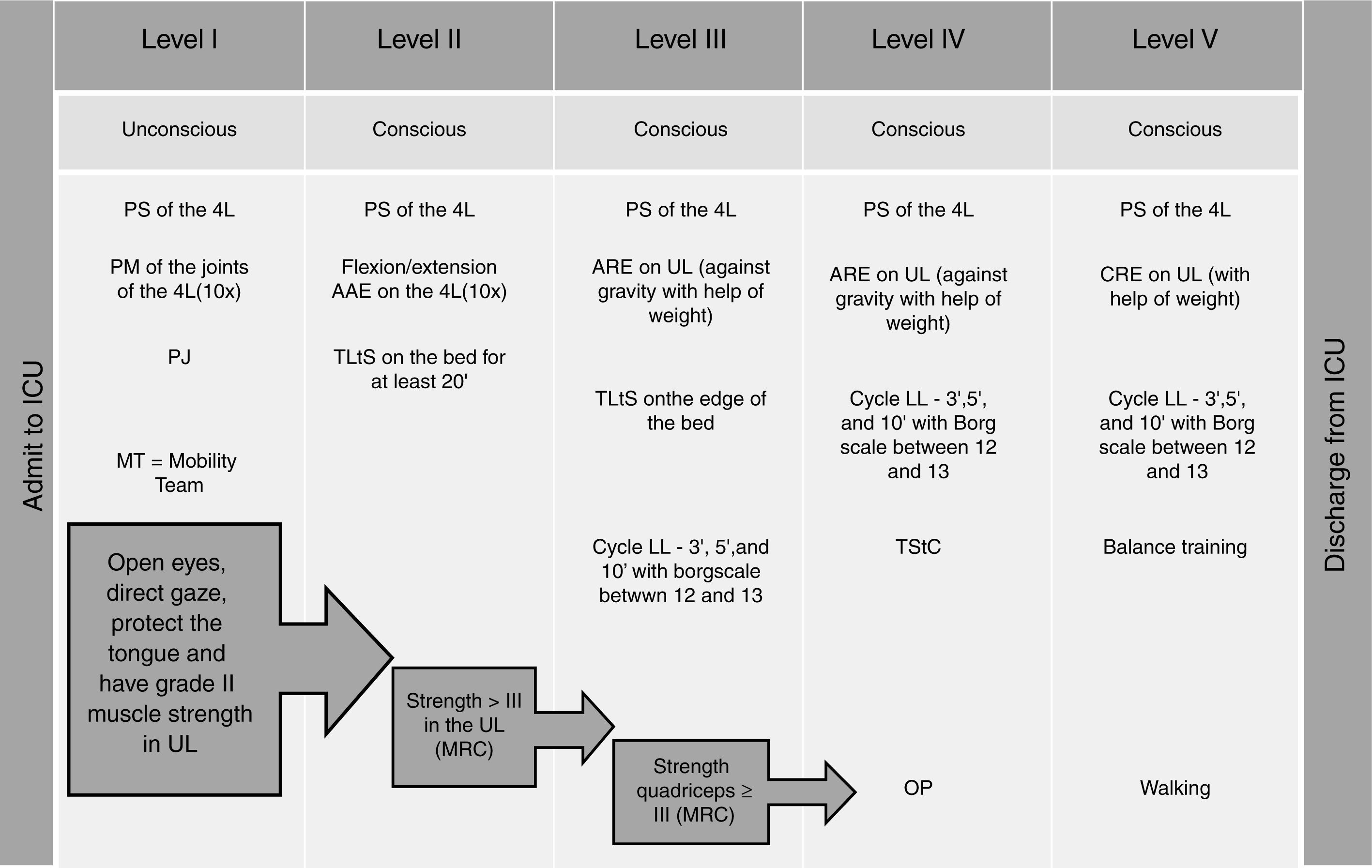
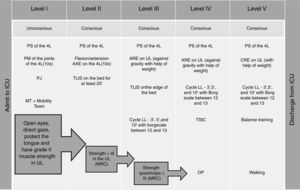
Dantas et al.30 made modifications to the protocol of Morris et al.,28 with the addition of an cycle ergometer and of level 5. The main finding was a gain of peripheral and respiratory muscle strength, with no difference in length of permanence (Fig. 3). Other studies, such as that of Burtin,31 have also described the use of some techniques but without specific description of the protocol. In this study, in the intervention group the authors instituted the use of passive cycle ergometer for 20min a day combined with the other interventions.
Early mobilization protocol for critically ill patients on mechanical ventilation. ICU – intensive care unit; PS – passive stretching; 4L – four limbs; PM – passive mobilization; PJ – positioning of the joint; UL – upper limbs; AAE – active-assisted exercise; TLtS – transfer from lying to sitting position; MRC – Medical Research Council; ARE – active-resistive exercise; LL – lower limbs; cycle LL – cycle ergometry for lower limbs; TStC – transfer from sitting to chair; OP – orthostatic posture; CRE – counter-resistance exercise.
Recently, another mobilization protocol for surgical patients in the intensive care unit identified important results such as reducing the length of stay in ICU (75–12 vs. 106–15 days; p<0.0001) and better mobility at the time of hospital discharge (mmFIM score 84–8 vs. 52–8; p=0.0002).32 The protocol used was the optimal mobilization SICU score (SOMS), which is a numerical scale ranging from 0 to 4 based on the patient mobilization level (dependent to independent transfers and locomotion).
Early mobilization improves outcomes: an absolute truth?Although early mobility in medical and surgical ICUs has shown to be safe and feasible, two trials and a systematic review showed results divergent from what was expected. Moss et al.33 conducted a clinical trial with patients who needed the support of mechanical ventilation for at least 4 days. The patients were randomized into two groups: intensive physical therapy and the standard physical therapy program. Intensive physiotherapy consisted of 7 days a week with the continuity of the protocol at home, and the standard program was offered 3 times a week. Physical function measures were performed at 1, 3 and 6 months after discharge from the ICU. There were no differences between the two groups in those pre-determined intervals. This trial had limited sample size, which may influence on confidence interval of measured effect of PT interventions.
Another large study was conducted in patients who had suffered a stroke (Study AVERT).34 This randomized single blind trial recruited 2083 patients into two groups: standard or usual care and early mobilization within the first 24h of hospital admission. Very early mobilization was associated with a reduced chance of a successful outcome after 3 months of the stroke.
A recent meta-analysis of six randomized trials found that early mobilization while in the ICU was not associated with improvements in functional outcomes, quality of life and use of health care, but there was improvement in the ability to walk without assistance.35 However, this review used articles whose quality assessed on the PEDro scale (which ranges from 0 to 10) was relatively low: most articles varied in score from 4 to 7/10, and only one article obtained 8/10 on that scale. Another factor which contributed to unfavorable results from early mobilization in this meta-analysis was the instruments used for the functional evaluation in the assessed studies: scales such as Katz and Barthel were not created specifically for the environment of intensive care. An adequate functional scale should cover the full distribution of the concept to be measured, that is, it should measure and detect the change in the whole range of possible functional results. The Barthel Index, which has been used in most studies evaluating functionality in intensive care, is not sensitive to changes in the extremes of functionality. These effects, “floor” and “ceiling”, make the scale less demanding in critical patients.36
Other potential factors for the lack of benefits from early mobilization interventions in the critical environment observed in these studies must be discussed: the population of critical patients is very heterogeneous with great variability in the recovery of long-term physical function. On the other hand, early mobilization programs that focus on specific target populations, such as those with weakness due to immobility and preserved neuromuscular excitability, can achieve more positive effects from the treatment. Future studies that seek to identify strategies to stratify which patients demonstrate greater benefits with early mobilization programs should be developed with a larger sample size.
We have yet to determine the optimal level of physical therapy at different times (i.e. fully sedated patients, first awaking) in the ICU. It seems likely the same dose of physical therapy will not adapt to all patients. We do not know how to determine which patients can tolerate an increase of dose of exercise intensity, with either increased duration or frequency. In addition, the best time to start the mobilization program and dose-response analysis of different ICU populations must be investigated based on physical and functional outcomes.
Barriers to early mobilizationAlthough admittedly safe and beneficial, early mobilization is still not a routine in many ICUs worldwide. There are several barriers that prevent this practice from being consolidated and data obtained in research studies from being used in clinical practice. In a review, Dubb et al.37 describe these barriers as: (1) barriers related to the patient, including symptoms and conditions such as hemodynamic instability; (2) structural barriers such as human and technical resources (e.g.: protocols and equipment); (3) barriers related to the ICU culture, including habits and attitudes particular to each institution; and finally (4) barriers related to the process, from lack of coordination to the absence of rules that determine the distribution of tasks and responsibilities. These barriers are multifaceted, and barriers related to the patient are the most commonly cited.
Hodgson et al.,38 in a prospective cohort study conducted in twelve ICUs in Australia and New Zealand, showed that 63.5% of patients were not subject to early mobilization, and that this was due to the fact that patients were intubated or had a high level of sedation. The management of sedation levels with dose reduction and/or adequation so as to allow the participation of the patient in exercises is important to get positive outcomes. Other factors that appear to be associated with the success of early mobilization include adequate analgesia and early recognition/management of delirium.39
The criterion of patient safety also appears as a barrier commonly observed in clinical practice. The increased risk of the detachment of tubes, lines, catheters and probes is a common belief mainly among doctors and limits the role of the physiotherapist and jeopardizes the implementation of mobilization.40,41 Nydahl et al.42 describe this contraindication by physicians as one of the main barriers to early mobilization in mechanically ventilated patients. A number of studies, however, have shown that there is no risk to the patient's safety in an early mobilization program performed by qualified professionals.15,43,44
Factors related to the lack of equipment and professionals can be an important barrier to early mobilization. Cultural and regional differences in the formation of early mobilization teams and the establishment of protocols do apply in this context. The physical therapist should be responsible for prescribing the mobilization program, with the remaining team members contributing to the implementation of therapy. However, it is common in some countries to have the nurse as the exercise executor in the early stages of a mobilization protocol. In Brazil, the practice of mobilization by the nursing team is unusual. Passive or active mobilization techniques are not included in nursing undergraduate course in Brazil, fitting to the physiotherapist all the stages of a mobilization protocol.45,46 However, there are no studies yet for determining whether the outcomes provided by early mobilization as exclusively implemented by physiotherapists differ from those carried out by mobilization teams with the participation of nurses.
In the United States and other countries, the respiratory therapist is part of the team and responsible for managing mechanical ventilation during the process.39 In Brazil the profession of respiratory therapist does not exist. Thus, Brazilian physiotherapists are responsible for managing both the rehabilitation protocols and interact with physicians in mechanical ventilation adjustments and respiratory therapy.47,48 The accumulation of functions by Brazilian physical therapists may put at risk the implementation of early mobilization protocols.49
The availability of professionals to form a mobilization team is small and often cited in studies as one of the barriers for implementing mobilization routines, especially if attempting to remove the patient from bed or make a mechanically ventilated patient to walk.50 Time and the necessary staff to carry out the mobilization were the main barriers reported on a survey in North America. In Brazil, a resolution of the National Sanitary Surveillance Agency (ANVISA)51 rules that in the ICU should be maximum ratio of one physiotherapist every ten beds. Another important factor contained in this resolution is the rule that the physiotherapist should be exclusive for the ICU. This is different from other countries where the physiotherapist serves the ICU and wards. A Canadian study52 showed that the increase in the number of physiotherapists (one to three) during weekends for serving ICU/ward has significantly increased mobilization interventions. However, it is common to find hospitals in which such regulation is not followed, with incomplete duty shifts, physiotherapists assigned to ICUs and wards, or a lesser number of physiotherapists than required by the regulation.53
Pires-Neto et al.,54 in a study conducted at a Brazilian ICU, observed that in mechanically ventilated patients most of the exercises were performed with patients confined to their beds (55%), while out-of-bed activities such as sitting and walking were much less frequent (29%). However, the study authors were unable to determine whether the low percentage of out-of-bed mobilization was the result of sedation, lack of a mobilization culture by physiotherapists, or a decisive time factor. Overcoming the cultural barriers depends on the recognition by all professionals of the importance of early mobilization, and a joint effort by coordinators and senior managers seeking to implement multidisciplinary protocols that can prioritize the mobilization process. They have demonstrated that a culture that favors early mobilization is able to increase by up to three-fold the number of patients mechanically ventilated who are able to walk.
In short, many contraindication criteria to early mobilization are only relative and lack cost/benefit evaluation of the therapy. In a recent study, Hickmann et al.55 used only 5 contraindications to establish mobilization in the first 24h of ICU stay: acute myocardial infarction, active bleeding, increased intracranial pressure with instability of same, unstable pelvic fractures, and discontinuation of therapy. The hemodynamic parameters were rarely affected during mobilization causing discontinuation in only 0.8% of the activities mainly due to reversible hypotension or arrhythmia. The authors have shown that early mobilization is feasible in most critical patients, regardless of the need for mechanical ventilation, high FiO2, vasopressor dosing, or renal replacement therapy. The, the question is: Do we create excessive contraindications to early mobilization given that this type of therapy has been shown to be safe for most cases? Breaking down barriers and implementing ever earlier mobilization protocols is the challenge that lies ahead!
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this investigation.
Confidentiality of dataThe authors declare that no patient data appears in this article.
Right to privacy and informed consentThe authors declare that no patient data appears in this article.
Conflicts of interestThe authors declare that they have no conflicts of interest.