To assess the value of frailty screening tool (Identification of Senior at Risk [ISAR]) in predicting 30-day mortality risk in older patients attended in emergency department (ED) for acute heart failure (AHF).
DesignObservational multicenter cohort study.
SettingOAK-3 register.
SubjectsPatients aged ≥65 years attended with ADHF in 16 Spanish EDs from January to February 2016.
InterventionNo.
VariablesVariable of study was ISAR scale. The outcome was all-cause 30-day mortality.
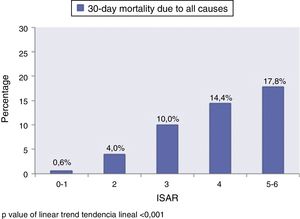
ResultsWe included 1059 patients (mean age 85±5.9 years old). One hundred and sixty (15.1%) cases had 0–1 points, 278 (26.3%) 2 points, 260 (24.6%) 3 points, 209 (19.7%) 4 points, and 152 (14.3%) 5–6 points of ISAR scale. Ninety five (9.0%) patients died within 30 days. The percentage of mortality increased in relation to ISAR category (lineal trend P value<.001). The area under curve of ISAR scale was 0.703 (95%CI 0.655–0.751; P<.001). After adjusting for EFFECT risk categories, we observed a progressive increase in odds ratios of ISAR scale groups compared to reference (0–1 points).
Conclusionsscale is a brief and easy tool that should be considered for frailty screening during initial assessment of older patients attended with AHF for predicting 30-day mortality.
Evaluar la utilidad de la escala de cribado de la fragilidad (Identification of Senior at Risk [ISAR]) para predecir la mortalidad a los 30 días en los pacientes mayores atendidos por insuficiencia cardiaca aguda (ICA) en los servicios de urgencias hospitalarios (SUH).
DiseñoEstudio multicéntrico observacional de cohorte multipropósito.
ÁmbitoRegistro OAK-3.
ParticipantesPacientes ≥ 65 años atendidos por ICA en 16 SUH españoles de enero a febrero del 2016.
IntervenciónNinguna.
VariablesLa variable de estudio fue la escala ISAR. La variable de resultado fue la mortalidad por cualquier causa a los 30 días.
ResultadosSe incluyó a 1.059 pacientes (edad media 85±5,9 años). Ciento sesenta (15,1%) casos tuvieron 0-1 puntos, 278 (26,3%) 2 puntos, 260 (24,6%) 3 puntos, 209 (19,7%) 4 puntos y 152 (14,3%) 5-6 puntos de la escala ISAR. Noventa y cinco (9,0%) pacientes fallecieron a los 30 días. La frecuencia de mortalidad se incrementó en relación a la categoría del ISAR (p tendencia lineal <0,001). El área bajo la curva de la escala ISAR fue de 0,703 (intervalo de confianza del 95%, 0,655-0,751; p <0,001). Tras el ajuste por las categorías del modelo de riesgo EFFECT, hubo un incremento progresivo de la razón de ventajas de los grupos de la escala ISAR en comparación con el grupo de referencia (0-1 puntos).
ConclusionesLa escala ISAR es una herramienta breve y sencilla que debería ser considerada para el despistaje de la fragilidad en la valoración inicial de los pacientes mayores con insuficiencia cardiaca aguda de cara a predecir la mortalidad a 30 días.
Acute heart failure (AHF) is a life-threatening condition that requires urgent evaluation and management.1 The physician in charge of first care, whether in the pre-hospital or the in-hospital setting,2,3 must identify the high-risk patient, start immediate treatment as required, and evaluate whether admission to intensive care is warranted.1,4 The decision to admit the patient to the Intensive Care Unit (ICU) is usually established on an individual basis, and should be fundamented upon risk models corresponding to the specific disease process involved.5,6 In clinical practice, such decision making can be very complex, particularly in elderly patients without severe dependency for activities of daily living and no advance directives referred to the limitation of therapeutic effort.7,8
Acute heart failure is one of the most common situations seen in the hospital Emergency Department (ED), and is the leading cause of hospital admission in elderly people.9 The definition of an “elderly person” is arbitrary, and is fundamented upon sociodemographic factors. Biological age is a term that encompasses the consequences of changes related to aging and associated disease, and is therefore able to characterize the elderly population better than chronological age.10 Frailty in turn is a marker of the biological age of an individual, and is defined as a state of maximum vulnerability in the face of situations of stress. Frailty is associated to poor outcomes.11 Different authors have considered that frailty should be included in the risk models12,13 and ought to be taken into account in the making of decisions referred to patient care.1,14–17
The Identification of Senior at Risk (ISAR) scale is a multidimensional frailty screening tool that has been found to be useful in stratifying the short term risk of adverse outcomes in elderly patients discharged from hospital.18–21 To date, there is no evidence of the usefulness of the ISAR scale in predicting short-term mortality risk in elderly individuals with AHF at the time of first care in the ED. The present study was therefore carried out to assess the usefulness of the ISAR scale in establishing the 30-day prognosis among elderly patients with AHF seen in the ED.
Material and methodsStudy design and patient selectionThe OAK register is a multicenter, multipurpose cohort observational study prospectively including patients≥65 years of age seen due to AHF in Spanish EDs during pre-established periods of two months every 2–3 years. To date, three patient recruitment phases have been completed: OAK-1: November-December 2011 (2 months, 3 EDs); OAK-2: January-February 2014 (2 months, 3 EDs) and OAK-3: January-February 2016 (2 months, 16 EDs). The present study involves the OAK-3 patients, since the ISAR scale was first used as a frailty screening tool in that patient cohort.
The details of the OAK register have been published elsewhere.14,16,22 In brief, the physician in charge of patient care identifies all the cases with a diagnosis of AHF based on the clinical, electrocardiographic and radiological findings, as well as on the type B natriuretic peptide concentrations and data corresponding to ultrasound exploration at the patient bedside, if available. The trained investigators in each center are available from 8a.m. to 10p.m. on working days (Monday to Friday), and select the patients≥65 years of age and conduct a short geriatric assessment while in the ED. The principal investigator of each center subsequently reviews all the selected cases (patients≥65 years of age with AHF that have undergone the short geriatric assessment) and finally includes in the register only those individuals that meet the diagnostic criteria of the heart failure guidelines of the European Society of Cardiology in force at the time of the study.23 The register excludes patients with ST-segment elevation acute myocardial infarction as AHF-triggering factor, as well as those patients who decline to participate.
In the present study we only included patients≥65 years of age with a diagnosis of AHF for which data were available referred to the ISAR scale and follow-up over 30 days.
Collection and definition of variablesThe ISAR scale is a tool applied in patients≥65 years of age that consists of 6 dichotomic (yes/no) questions referred to the patient self-perceived regular need for help in performing activities of daily living before the acute process, or the need for more help after the acute process; sensory deficits; cognitive impairment; hospitalization in the last 6 months; and the use of three or more drugs. The maximum score is 6 points, resulting from the sum of the 6 items that score as 0 or 1 (Table S1, supplementary material, Appendix B annex 2).18
We collected demographic data (age and gender), as well as information referred to the patient medical history (arterial hypertension, diabetes mellitus, dyslipidemia, ischemic heart disease, valve disease, atrial fibrillation, cerebrovascular disease, chronic renal failure, peripheral arterial disease, chronic obstructive pulmonary disease [COPD], dementia, cirrhosis, cancer, previous heart failure episodes and left ventricular function), basal cardiorespiratory condition (according to the New York Heart Association [NYHA] score), comorbidity (Charlson index), basal functional condition (1, severe dependency: Barthel index≤60 points; 2, frail without severe dependency: the patient meets≥3 modified Fried frailty criteria: (a) tiredness: Do you often feel that everything you do requires an effort?; (b) muscle strength: Do you have difficulty standing up from a chair?; (c) slow gait: Do you have big problems walking outside your home?; (d) physical activity: Do you exercise regularly?; (e) weight loss: Have you unintentionally lost weight in the last year?), and has a Barthel index>60 points; 3, no frailty or severe dependency: the patient meets no frailty criteria and has a Barthel index>60 points), clinical and laboratory test data corresponding to the acute episode (systolic blood pressure [SBP], heart rate, respiratory frequency, basal oxygen saturation as recorded by pulsioxymetry, hemoglobin, natremia, potassemia, creatinine clearance calculated using the MDRD-4 equation, and type B natriuretic peptide [NT-proBNP]), the treatment received while in the ED (oxygen, noninvasive mechanical ventilation, intravenous diuretics, intravenous nitroglycerin, angiotensin converting enzyme inhibitors [ACEIs], aldosterone receptor antagonists, beta-blockers and digoxin), and final destination (discharge/hospital admission).
The primary endpoint was mortality due to all causes 30 days after the index event, based on the review of the case history or telephone call to each patient or accompanying person between 31 and 60 days after care in the ED.
Statistical analysisQuantitative variables were expressed as the mean (standard deviation [SD]), while qualitative variables were reported as absolute and relative frequencies. The study sample was divided according to the ISAR score: (a) 0–1 points; (b) 2 points; (c) 3 points; (d) 4 points, and (e) 5–6 points. The comparative univariate analysis of the established ISAR categories was based on the Spearman correlation statistic for quantitative variables and the chi-squared test in the case of qualitative variables. These tests allowed us to evaluate the linear trend on increasing the ISAR score.
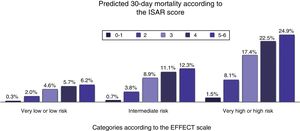
Logistic regression analysis was performed both with and without adjusting for the EFFECT scale risk categories, in order to determine the association between the ISAR categories and 30-day mortality. For this purpose, we used the data to calculate the 30-day mortality risk categories according to the EFFECT risk model (http://www.ccort.ca/Research/CHFRiskModel.aspx), grouping them into very low or low risk (≤ 90 points), intermediate risk (91–120 points) or high or very high risk (> 120 points).24 Multiple imputation techniques were used to produce 50 series of imputed data to replace the lost values of the variables entered in the EFFECT risk model (age, respiratory frequency, systolic blood pressure, blood urea nitrogen [BUN], natremia, cerebrovascular disease, dementia, chronic obstructive pulmonary disease, cirrhosis and cancer). The measures of effect of the different ISAR categories were expressed as the odds ratio (OR), with the corresponding 95% confidence interval (95%CI) (crude and adjusted). The predicted probabilities of the IDSAR risk categories were stratified according to the EFFECT scale risk categories.
The area under the curve (AUC) was calculated, along with the corresponding 95%CI, and the sensitivity, specificity, positive predictive value (PPV) and negative predictive value (NPV) of the different ISAR scale cut-off points for 30-day mortality.
Differences were regarded as statistically significant for p<0.05, when the 95%CI or OR excluded the value 1, and the area (AUC) under the receiver operating characteristic (ROC) curve excluded the value 0.5. The statistical analyses were carried out using the SPSS version 24 (IBM, New Castle, NY, USA) and STATA version 15.1 (Stata Corp., College Station, TX, USA) statistical packages.
Ethical aspectsThe OAK register abided with the guidelines of the Declaration of Helsinki regarding medical research in humans, and the patients gave informed consent to participation in the study, which was approved by the Clinical Research Ethics Committee of Hospital Clínico San Carlos (Madrid, Spain) (Reference: C.P. PI15/00773-C.I. 15/189-E_BS), as well as by the rest of the Committees of the participating hospital centers.
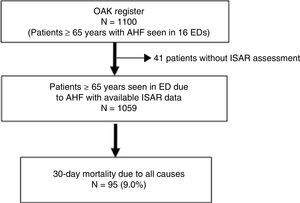
ResultsThe present study included 1059 patients of the 1100 cases of the OAK-3 register. Forty-one patients lacking data referred to the ISAR scale were excluded (Fig. 1).
The mean age of the patients included in the study was 85 (SD 5.9) years; 604 (57.2%) were women; and 701 (66.4%) had suffered a previous AHF episode. The mean ISAR score was 2.9 (SD 1.3) points. Eleven subjects (1.0%) yielded an ISAR score of 0 points, 149 (14.1%) a score of 1 point, 278 (26.3%) a score of 2 points, 260 (24.6%) a score of 3 points, 209 (19.7%) a score of 4 points, 122 (11.5%) a score of 5 points, and 30 (2.8%) a score of 6 points. Ninety-five patients (9.0%) died in the first 30 days following care in the ED. Tables S2a and S2b of the supplementary material (Appendix B annex 2) show the characteristics of the patients included in the study.
Tables S3a and S3b of the supplementary material (Appendix B annex 2) report the distribution of elderly patients with AHF according to the categories established by the ISAR scale. As the ISAR score increased, patient age was seen to rise, with a greater presence of women, arterial hypertension, chronic renal failure, cerebrovascular disease, previous heart failure episodes, dementia, severe comorbidity, physical frailty and dependency for activities of daily living, basal NYHA functional class III–IV, systolic blood pressure <110mmHg, tachypnea, basal oxygen saturation <90%, renal failure, anemia, hospital admission and 30-day mortality.
Fig. 2 shows the increase in frequency of 30-day mortality in relation to the ISAR category. The AUC of ISAR was 0.703 (95%CI: 0.655–0.751; p<0.001) for 30-day mortality. Table 1 reports the measures of effect, both crude and adjusted for the risk groups of the EFFECT scale, corresponding to each of the ISAR categories for the adverse event. Fig. 3 documents the predicted probabilities of the ISAR categories stratified by EFFECT scale risk groups. Table 2 shows the characteristics of the ISAR scale according to the different established cut-off points.
Crude and adjusted odds ratios (OR) corresponding to 30-day mortality due to all causes, according to the 5 categories established by the ISAR scale.
| Univariate analysis | Multivariate analysis | |||||
|---|---|---|---|---|---|---|
| Crude OR | 95%CI | p | Adjusted OR | 95%CI | p | |
| ISAR | ||||||
| 0–1 points | Ref. | Ref. | ||||
| 2 points | 6.5 | 0.8–51.2 | 0.073 | 6.0 | 0.8–47.1 | 0.088 |
| 3 points | 17.7 | 2.4–131.5 | 0.005 | 14.1 | 1.9–105.7 | 0.010 |
| 4 points | 26.6 | 3.6–197.6 | 0.001 | 17.8 | 2.4–133.2 | 0.005 |
| 5–6 points | 34.3 | 4.6–256.2 | 0.001 | 19.3 | 2.5–146.1 | 0.004 |
Adjusted to the EFFECT risk model (age, respiratory frequency, systolic blood pressure, blood urea nitrogen [BUN], natremia, cerebrovascular disease, dementia, chronic obstructive pulmonary disease, cirrhosis and cancer).
Validity of the different ISAR scale cut-off points corresponding to 30-day mortality.
| Frequency | Sensitivity(95%CI) | Specificity(95%CI) | PPV(95%CI) | NPV(95%CI) | AUC(95%CI) | |
|---|---|---|---|---|---|---|
| ISAR | ||||||
| ≥2 points | 94/899 (10.5) | 98.9 (93.4–99.9) | 16.5 (14.2–19.0) | 10.5 (8.6–12.7) | 99.4 (96.0–99.9) | 0.577 (0.524–0.631) |
| ≥3 points | 83/621 (13.4) | 87.4 (7.6–93.0) | 44.2 (41.0–47.4) | 13.4 (10.8–16.4) | 97.3 (95.1–98.5) | 0.658 (0.608–0.708) |
| ≥4 points | 57/361 (15.8) | 60.0 (49.4–69.8) | 68.5 (65.4–71.4) | 15.8 (12.3–20.1) | 94.6 (92.5–96.1) | 0.642 (0.583–0.702) |
| ≥5 points | 27/152 (17.8) | 28.4 (19.9–38.7) | 87.0 (84.7–89.1) | 17.8 (12.2–25.0) | 92.5 (90.5–94.1) | 0.577 (0.513–0.642) |
AUC, area under the curve; CI, confidence interval; PPV, positive predictive value; NPV, negative predictive value.
The present study offers important results: (1) the ISAR scale has good 30-day mortality predictive capacity in patients≥65 years of age with AHF seen in the ED; (2) the ISAR scale should not be applied with a pre-established cut-off point but rather considering that as the total score increases, there is a greater probability of a poorer short-term outcome; (3) the category of the ISAR scale is correlated to the degree of comorbidity, physical and cognitive frailty, and the severity of the episode; and (4) the ISAR scale affords information on variables related to the functional, cognitive and sensory situation of the patient, polypharmacy and previous contact with the healthcare system, generally not contemplated in AHF risk models, and which could prove useful in stratifying short-term risk in this group of patients.
The ISAR scale classically has been used as a frailty screening tool in elderly patients, with a view to predicting short-term adverse effects in individuals discharged directly from the ED, or even to select those patients that might benefit from integral geriatric assessment.19–21,25,26 Such integral assessment is the reference frailty diagnostic test, and has been shown to increase the probability of returning home and of being alive after 12 months among the hospitalized elderly.27 The consumption of human resources and the time needed to complete such assessment limit its application in the ED, however. Consequently, in the case of acute situations, it is preferable to use scales based on self-reporting questions or on the subjective clinical judgment of the healthcare professionals, and to postpone integral geriatric assessment until clinical stabilization has been achieved.14,15 Different frailty screening scales have been described, such as the ISAR scale,18 the Frail scale,28 the Clinical Frailty scale29 or the Tilburg Frailty Indicator.30 Despite the lack of evidence of these scales in application to AHF, the ISAR scale is recommended as the tool of choice in screening for frailty among elderly patients with AHF seen in the ED.14
The present study for the first time evaluates the validity of the ISAR scale in predicting the short-term outcome among elderly patients with AHF seen in the ED. The results show that the scale has good 30-day mortality predictive capacity. This fact is of clinical relevance, since this outcome variable has classically been used to derive the risk models that are of help in decision making referred to issues such as the need for hospital admission or the best place for patient admission.31 Furthermore, the scale has been found to contribute information on frailty to the EFFECT risk model, which focuses on cardiological variables.24 In this respect, it is known that risk models that do not consider variables related to biological age have only limited predictive capacity in the elderly population with AHF.31
The ISAR scale meets the requirements of simplicity and briefness for application in the emergency care setting. The scale comprises 6 dichotomic questions that are answered by the patient and/or caregiver at the time of first care, and which allow us to quantify the degree of multidimensional frailty at the patient bedside, without the need for a physical performance test (e.g., gait speed, up and go test, or the Short Physical Performance Battery), or for lengthy functional scales (e.g., the Barthel index) or short geriatric assessments (e.g., the Multidimensional Prognostic Index), which are sometimes difficult to apply in decision making in a life-threatening scenario.14 For example, it has been estimated that administration of the Barthel index takes about 5min. Therefore, the incorporation of this functional variable to AHF risk models such as the BI-EFFECT scale,32 the FBI-EFFECT scale13 or the MEESSI-AHF scale,33 largely complicates the applicability of these tools at the time of first care in patients with AHF in the emergency care setting.
To date, the ISAR scale has been used in clinical practice as a screening tool with a cut-off score of 2 points, which affords high sensitivity and limited specificity for the adverse outcome variables.19–21,34 Two recent meta-analyses have shown that this cut-off score of 2 points on the ISAR scale has a sensitivity of 97–99% and a specificity of 24–27%20,21 for 30-day mortality. The results of our study are consistent with this. Furthermore, we found a cut-off score of 3 to yield the greatest predictive capacity for this outcome variable. Modification of the ISAR cut-off score to 3 has already been commented by other authors.19–21 However, in our opinion, the scale should be regarded as a frailty index, i.e., as the sum of positive questions increases, so does the 30-day mortality risk.
With regard to the frequency of the different items of the ISAR scale, the item referred to serious memory problems was the least frequent (17.4%), while the use of three or more drugs was identified in practically all of the sample (96.3%). This latter observation caused the question referred to chronic medication to be non-discriminative in our sample. Previous studies have modified the polypharmacy cut-off point to 5, 6 or 8 drugs, without demonstrating clear improvement in the discriminative capacity of this scale.20,34,35
Our results are consistent with the data found in the literature regarding the high frequency of comorbidity, frailty and disability in elderly individuals with AHF.36,37 As in previous studies, the ISAR scale showed increasing scores to be associated to a greater frequency of elderly patients with important comorbidity and physical and cognitive frailty.34 Comorbidity, the cognitive situation and the degree of frailty and disability are poor outcome factors in AHF.16,32 This could explain the direct relationship observed between the ISAR score and the short-term mortality risk after adjusting for the risk categories of the EFFECT model, which includes variables related to age, comorbidity and data referred to the acute episode.
A notorious observation was the fact that two out of every three of the elderly patients had no serious dependency referred to activities of daily living. This shows that there is a potentially large group of elderly individuals who a priori could be admitted to intensive care, and that new parameters related to biological age therefore should be incorporated to the patient assessment process. An evident example of this circumstance is the application of the EAHFE-3D scale as a tool of help in identifying patients at high life-threatening risk,38 and therefore amenable to admission to the ICU. An age of 75 years or older is one of the 7 items on that scale, and is one of the three – along with respiratory failure and inotropic or vasopressor drug use – that contributes most points to the total score. In this regard, the universal application of this prognostic model, without considering frailty, could result in an inappropriate number of admissions to intensive care. In turn, the determination of this frailty index, in combination with other variables or risk models commonly used in clinical practice, could be of great help in decision making and for establishing individualized management plans for elderly patients with AHF.14,15
The present study has limitations. It is an exploratory study based on a multipurpose register – a fact that has limited the number of events required for the number of categories investigated. Selection bias cannot be ruled out, since systematic sampling was performed in which geriatric assessment adapted to the ED setting was made from 8a.m. to 10p.m. on working days. The ISAR data were extracted from the short geriatric assessment of the patient during acute phase care by different investigators in each center; some degree of interindividual variability therefore may exist. The information referred to prognostic biomarkers such as troponin or lactate was not available, since these parameters are not routinely compiled in all patients seen for AHF in Spanish EDs.39 The treatments prescribed during the acute phase and after discharge were left to the criterion of the supervising physicians, and this consequently may have influenced the results.40 Nevertheless, this circumstance allows the findings to be more real and thus more generalizable to clinical practice.
In conclusion, the ISAR scale is a simple tool that could be considered in the initial assessment of elderly patients with AHF in the ED, with a view to stratifying 30-day mortality risk.
AuthorshipFJMS designed the study. FJMS and OM obtained funding for the investigation. FJMS supervised conduction of the study and data collection. All the investigators of the OAK register recruited patients. FJMS managed the data, including the quality controls. FJMS, XR and CFP performed the statistical analysis of the data. FJMS wrote the manuscript, and XR, OM, MGC, ADR contributed substantially to its review. FJMS is responsible for the manuscript as a whole.
FundingThe present study has been possible in part thanks to aids PI15/00773, PI15/01019, PI11/01021 and PI10/01918 of the Instituto de Salud Carlos III with funds from the Spanish Ministerio of Sanidad, Servicios Sociales e Igualdad (MSSSI) and the European Regional Development Fund (ERDF); aids of the Generalitat de Catalunya for Consolidated Research Groups (GRC 2009/1385, 2014/0313 and 2017/1424); and the La Marató aid of TV3 (20152510). Xavier Rossello has been financed by the SEC-CNIC CARDIOJOVEN fellowship.
Conflict of interestThe authors declare that they have no conflicts of interest.
Esther Rodríguez Adrada, María Carmen Santos, Lucía Salgado, Berenice Nayla Brizzi, María Luisa Docavo, María Suárez Cadenas (Hospital Clínico San Carlos, Madrid), Carolina Xipell, Carolina Sánchez, Sira Aguiló, Josep María Gaytan, Alba Jerez (Hospital Clínic de Barcelona), María José Pérez-Durá, Pablo Berrocal Gil (Hospital La Fe de Valencia), María Luisa López-Grima, Amparo Valero (Hospital Dr. Peset de Valencia),Alfons Aguirre, Maria Àngels Pedragosa (Hospital del Mar de Barcelona), Pascual Piñera, Paula Lázaro Aragues, José Andrés Sánchez Nicolás (Hospital Reina Sofía de Murcia), Miguel Alberto Rizzi, Sergio Herrera Mateo, Aitor Alquezar (Hospital de la Santa Creu y Sant Pau de Barcelona), Alex Roset, Carles Ferrer, Ferrán Llopis (Hospital Universitari de Bellvitge, Barcelona), José María Álvarez Pérez, María Pilar López Diez, Fernando Richard (Hospital Universitario de Burgos), José María Fernández-Cañadas, José Manuel Carratalá, Patricia Javaloyes (Hospital General de Alicante), Juan Antonio Andueza, José Antonio Sevillano Fernández, (Hospital General Universitario Gregorio Marañón de Madrid), Rodolfo Romero, Marta Merlo Loranca. Virginia Álvarez Rodríguez (Hospital Getafe de Madrid), María Teresa Lorca, Luis Calderón (Hospital del Tajo de Madrid), Ester Soy Ferrer (Hospital Josep Trueta de Girona), José Manuel Garrido (Hospital Virgen de la Macarena de Sevilla), Enrique Martín Mojarro (Hospital Sant Pau i Santa Tecla, Tarragona, Spain).
Please cite this article as: Martín-Sánchez FJ, Llopis García G, González-Colaço Harmand M, Fernandez Pérez C, González del Castillo J, Llorens P, et al. La escala Identification of Senior At Risk predice la mortalidad a los 30 días en los pacientes mayores con insuficiencia cardiaca aguda. Med Intensiva. 2020;44:9–17.