To assess whether patient age is independently associated to Intensive Care Unit (ICU) admission after non-cardiac surgery.
DesignAn observational cohort study of the Spanish subset of the European Surgical Outcome Study (EuSOS) was carried out.
SettingHospitals of the public National Health Care System and private hospitals in Spain.
InterventionNone.
Patients and methodsAll patients over 16 years of age undergoing inpatient non-cardiac surgery in the participating hospitals during a 7-day period in the month of April 2011 were consecutively included.
Main variables of interestICU admission rate, factors associated with ICU admission and hospital mortality were assessed using logistic regression analysis and fractional polynomial regression.
ResultsOut of 5412 patients, 677 (12.5%) were admitted to the ICU after surgery. The adjusted odds ratio (95% confidence interval [CI]) for ICU admission was 1.1 (0.8–1.4) for patients aged 65–74 years, 0.7 (0.5–1) for patients aged 75–85 years, and 0.4 (0.2–0.8) for patients over 85 years, respectively. Age, ASA score, grade of surgery (minor, intermediate, major), urgent surgery, surgical specialty, laparoscopic surgery and metastatic disease were independent factors for ICU admission. Global risk-adjusted mortality was 1.4 (95% CI 0.9–2.2). The ASA score, urgent surgery, surgical specialty and diabetes were predictors of hospital mortality.
ConclusionsElderly patients (over 80 years) appear less likely to be admitted to ICU after non-cardiac surgery in Spanish hospitals. There was no significant association between age and postoperative mortality in this cohort.
Evaluar si la edad del paciente se asociaba independientemente con el ingreso en la unidad de cuidados intensivos (UCI) tras cirugía no cardiaca.
DiseñoEstudio observacional de cohortes del subgrupo español del European Surgical Outcome Study (EuSOS).
ÁmbitoHospitales públicos y privados en España.
IntervenciónNinguna.
Pacientes y métodosPacientes consecutivos mayores de 16 años sometidos a cirugía no cardiaca con ingreso durante un periodo de 7 días del mes de abril de 2011.
Variables de interés principalTasa de ingreso en la UCI, factores asociados con ingreso en la UCI y mortalidad hospitalaria, analizadas mediante regresión logística y regresión fraccional polinómica.
ResultadosDe 5.412 pacientes, 677 (12,5%) fueron ingresados en la UCI tras la cirugía. La odds ratio ajustada (intervalo de confianza [IC] del 95%) de ingreso en la UCI fue de 1,1 (0,8-1,4) para 65-74 años, 0,7 (0,5-1) para 75-85 años y de 0,4 (0,2-0,8) para más de 85 años, respectivamente. La edad, el grado ASA, el grado de la cirugía (menor, intermedia, mayor), la cirugía urgente, la especialidad quirúrgica, la cirugía laparoscópica y la enfermedad metastásica fueron factores independientes de ingreso en la UCI. El riesgo global ajustado de mortalidad fue de 1,4 (IC 95%: 0,9-2,2). El grado ASA, cirugía urgente, especialidad quirúrgica y diabetes fueron predictores de mortalidad hospitalaria.
ConclusionesEn los hospitales españoles, los pacientes ancianos (más de 80 años) son menos propensos a ser ingresados en la UCI tras cirugía no cardiaca. En esta cohorte, la edad y la mortalidad hospitalaria no se asociaron significativamente.
More than 310 million surgical procedures are performed worldwide every year1 but there are few data describing subsets of populations that may be at particularly high risk of post-operative mortality. Post-operative intensive care admission may improve outcomes, especially in high-risk patients.2,3 The ageing population is a global concern, but particularly in Spain, where the life expectancy is amongst the highest in the world, and one third of the population is aged 60 years.4 The ageing of the population will place increasing demands on healthcare services including intensive care resources.
Very elderly patients (over 80 or 85 years) represent a high-risk population due to their frailty and associated morbidity.5 In this population, the criteria for ICU admission are at times controversial, both ethically and economically. The likelihood that elderly patients are admitted to intensive care after surgery may be not the same as younger age groups (65–85 years).6,7 Recently, the percentages of ICU admissions and treatment days attributable to the very elderly have been reported to increase after cardiac surgery, but not after non-cardiac surgery.8 The findings of studies exploring the benefits of post-operative intensive care admission for elderly patients are inconsistent.9–11
In 2011, seventy-one per cent of ICU beds in Spain were dependent of the Services of Intensive Care Medicine as a primary speciality, and most of them were polyvalent (medical, surgical and coronary).12 In Spain, universal health coverage is provided and delivery of intensive care is near the European average (10.3 and 11.5 ICU beds per 100.000 inhabitants, respectively).12,13 However, a higher rate of post-operative ICU admission after non-cardiac surgery compared to the European average has been reported (12.5% vs 8%, respectively).14 The aim of this analysis was to determine the impact of age as an independent factor of ICU admission after non-cardiac surgery in Spain using data from the European Surgical Outcome Study (EuSOS).14 Secondary objectives were to determine, in the elderly after non-cardiac surgery, factors associated with ICU admission and hospital mortality.
Patients and methodsThis was an observational cohort study of the Spanish subset of the EuSOS (NCT01203605). The study was conducted in accordance with the strengthening the reporting of observational studies in epidemiology (STROBE) statement (www.strobe-statement.org). Ethical approval for EuSOS (Ethical Committee N° 10/H0605/72) was provided by the Ethics Committee of Queen Mary University of London (London, United Kingdom) and all Spanish hospitals participants obtained approval from the local ethics committee from the primary European coordinating centre. After contacting the primary European coordinating centre, both surgical and critical care dataset of the 61 Spanish centres participating in the EuSOS were obtained completed and confirmed.
EuSOS sample size and study methodology is described in detail in the original article.14 In short, the cohort study was conducted for 7 days in the month of April 2011. During this period, all patients over 16 years undergoing non-cardiac surgery were consecutively included. Patients undergoing outpatient surgery, obstetrical procedures and neurosurgery were excluded. A paper questionnaire for each patient and the data were entered anonymously in an electronic registry. A critical care case record form was used to capture data describing the first admission (defined as planned or unplanned) to critical care for any individual patient at any time during the follow-up period. In the EuSOS, intensive care unit (ICU) was defined as a facility routinely capable of admitting patients who require invasive ventilation overnight and post-anaesthetic care unit (PACU) as a dedicated facility for the care of all patients following surgery under anaesthesia regardless of organ support. The main objective of the study was hospital mortality and patients were followed for up to 60 days after hospital admission. Patients were categorised according to demographic data that included age, sex, smoking, American Society of Anaesthesiologists (ASA) score, the urgency and extent of surgery and comorbidities. A total of 45,666 patients treated at 366 centres in 28 European countries were included. The Spanish cohort consisted of 5412 adult patients from sixty-one hospitals (70% university hospitals), and the average number of patients included per hospital was of 89. The primary endpoint was admission to intensive care. Secondary outcomes measures were factors associated with ICU admission, hospital length of stay and hospital mortality.
Statistical analysisA descriptive analysis of the Spanish subset of the EuSOS, including demographic and surgical characteristics, was carried out. Because we wanted to focus on the elderly patients, instead of dividing the sample into quartiles or quintiles by age, we stratified into three age groups following World Health Organisation's (WHO) definition of young (less than 65 years), young elderly (aged 65–85 years) and old elderly (over 85 years).15 We then subdivided the young elderly into two subgroups (65–74 and 75–85 years) and compared the four categories in terms of ICU admission adjusted to demographic and surgical variables. To avoid prejudicial findings, and for sensitivity analysis, we repeated the analysis dividing all patients into quartiles of age and also compared the four groups in the same terms.
Main predictors were age differences of ICU admission and mortality, adjusted by other demographic and surgical variables as potential confounders, and were tested by means of a chi squared and Kruskal–Wallis test. A logistic model was fitted to relate age with ICU admission, outcomes and mortality. As age relationship was not linear, it was introduced in the logistic model as categorical with less than 65 years group as reference. A multivariable model was built adding the demographic and surgical variables.
The fitted step age function could fit data less than the continuous variable, moreover when cut points are arbitrary. A better way to analyse the shape of the relation of age with mortality and ICU admission is adjusting a more flexible model such as fractional polynomial regression.16 Fractional polynomials increase the flexibility afforded by the family of conventional polynomial models (linear or quadratic). Up to a (−3.3) fractional polynomial analysis was tested and the model with lowest deviance was finally selected. This flexible method enhances the predict ability of variables and improves the performance of the relationship.17 In order to assess stability of selected polynomial, a 100 bootstrap sample was drawn and applied the closed-test procedure to determine the most appropriate fractional polynomial.
Data are presented as percentages for binary data, mean (±standard deviation) and median with interquartile range (IQR) (25th–75th percentile) for continuous data, or odds ratio (OR) and 95% confidence interval (CI). Statistical significance was set at P<0.05. Analyses were performed using STATA 13.1 (StataCorp, USA).
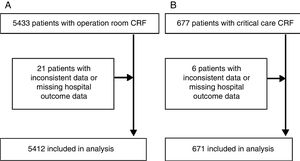
ResultsThe Spanish subset of EuSOS consisted of 5433 patients, of which 5412 were included for analysis (Fig. 1). The average number of patients included per hospital and the percentage of university hospitals in Spain was similar than the European cohort (89 versus 83 patients per hospital and 70% vs 68% of university hospitals, respectively).
Mean age of the Spanish subset of EuSOS was of 58±18 years (range 16–102 years). Following the WHO's definition, 3207 patients (59%) were included in the younger group (less than 65 years), 1074 (19.8%) were 65–74 years, 963 (17.7%) were 75–85 years and 189 (3.5%) were over 85 years. Table 1 shows the demographic and surgical characteristics among age categories, as well as PACU and hospital length of stay. The length of stay in the PACU varied in the different age groups, with a median of 120min (IQR 74–210). Older patients had longer stays in the PACU than younger counterparts (P<0.001).
Demographic and surgical characteristics among age categories.
| <65 years (n=3195) | 65–74 years (n=1069) | 75–85 years (n=959) | >85 years (n=189) | Total (n=5412) | P value | |
|---|---|---|---|---|---|---|
| Men | 1590 (49.8) | 472 (44.1) | 499 (52.0) | 126 (66.7) | 2687 (49.6%) | <0.001 |
| Smoker | 974 (30.5) | 133 (12.4) | 73 (7.6) | 7 (3.7) | 1187 (21.9%) | <0.001 |
| ASA score | ||||||
| I | 1043 (32.64%) | 48 (4.5%) | 11 (1.1%) | 2 (1.1%) | 1104 (20.4%) | <0.001 |
| II | 1624 (50.8%) | 600 (56.1%) | 410 (42.7%) | 49 (25.9%) | 2683 (49.6%) | |
| III | 462 (14.5%) | 378 (35.4%) | 440 (45.9%) | 108 (57.1%) | 1388 (25.6%) | |
| IV | 62 (1.9%) | 40 (3.7%) | 96 (10%) | 29 (15.3%) | 227 (4.2%) | |
| V | 4 (0.1%) | 3 (0.3%) | 2 (0.2%) | 1 (0.5%) | 10 (0.2%) | |
| Comorbidities | ||||||
| Cirrhosis | 54 (1.7%) | 17 (1.6%) | 10 (1.0%) | 2 (1.1%) | 83 (1.5%) | 0.502 |
| CHF | 30 (0.9%) | 39 (3.6%) | 76 (7.9%) | 23 (12.2%) | 168 (3.1%) | <0.001 |
| COPD | 261 (8.1%) | 159 (14.9%) | 161 (16.8%) | 31 (16.4%) | 612 (11.3%) | <0.001 |
| CAD | 97 (3.0%) | 128 (12%) | 161 (16.8%) | 33 (17.5%) | 419 (7.7%) | <0.001 |
| Diabetes (insulin) | 85 (2.7%) | 69 (6.4%) | 90 (9.4%) | 10 (5.3%) | 254 (4.7%) | <0.001 |
| Diabetes (no insulin) | 177 (5.5%) | 147 (13.7%) | 188 (19.6%) | 34 (18%) | 546 (10.1%) | <0.001 |
| Metastatic disease | 119 (3.7%) | 62 (5.8%) | 41 (4.3%) | 6 (3.2%) | 228 (4.2%) | 0.028 |
| Stroke | 55 (1.7%) | 67 (6.3%) | 101 (10.5%) | 20 (10.6%) | 243 (4.5%) | <0.001 |
| Grade of surgery | ||||||
| Minor | 629 (19.7%) | 169 (15.8%) | 129 (13.4%) | 23 (12.2%) | 950 (17.5%) | <0.001 |
| Intermediate | 1652 (51.7%) | 481 (45%) | 445 (46.4%) | 109 (57.7%) | 2687 (49.6%) | |
| Major | 914 (28.6%) | 419 (39.2%) | 385 (40.1%) | 57 (30.2%) | 1775 (32.8%) | |
| Urgency of surgery | ||||||
| Elective | 2636 (82.5%) | 929 (86.9%) | 754 (78.6%) | 117 (61.9%) | 4436 (82%) | <0.001 |
| Urgent | 491 (15.4%) | 128 (12%) | 180 (18.8%) | 65 (34.4%) | 864 (16%) | |
| Emergent | 68 (2.1%) | 12 (1.1%) | 25 (2.6%) | 7 (3.7%) | 112 (2.1%) | |
| Surgical speciality | ||||||
| Orthopaedics | 766 (24%) | 268 (25.1%) | 312 (32.5%) | 80 (42.3%) | 1426 (26.3%) | <0.001 |
| Breast | 111 (3.5%) | 32 (3%) | 17 (1.8%) | 3 (1.6%) | 163 (3%) | |
| Gynaecology | 338 (10.6%) | 52 (4.9%) | 46 (4.8%) | 7 (3.7%) | 443 (8.2%) | |
| Vascular | 122 (3.8%) | 58 (5.4%) | 81 (8.4%) | 24 (12.7%) | 285 (5.3%) | |
| Upper GI | 129 (4.0%) | 60 (5.6%) | 44 (4.6%) | 6 (3.2%) | 239 (4.4%) | |
| Lower GI | 381 (11.9%) | 125 (11.7%) | 137 (14.3%) | 22 (11.6%) | 665 (12.3%) | |
| Hepato-biliary | 185 (5.8%) | 74 (6.9%) | 48 (5.0%) | 6 (3.2%) | 313 (5.8%) | |
| Plastic | 164 (5.1%) | 32 (3%) | 28 (2.9%) | 7 (3.7%) | 231 (4.3%) | |
| Urology | 272 (8.5%) | 202 (18.9%) | 131 (13.6%) | 18 (9.5%) | 623 (11.5%) | |
| Kidney | 30 (0.9%) | 15 (1.4%) | 4 (.04%) | 1 (0.5%) | 50 (0.9%) | |
| Head and neck | 506 (15.8%) | 85 (7.9%) | 50 (5.2%) | 7 (3.7%) | 648 (12%) | |
| Other | 191 (6%) | 66 (6.2%) | 61 (6.3%) | 8 (4.2%) | 326 (6.0%) | |
| Laparoscopic surgery | 461 (14.4%) | 135 (12.6%) | 71 (7.4%) | 8 (4.2%) | 675 (12.5%) | <0.001 |
| PACU LOS (min) | 115 (70; 185) | 130 (80; 240) | 140 (80; 250) | 140 (90; 240) | 120 (74; 210) | <0.001 |
| Hospital LOS (days) | 8 (5; 16) | 8 (5; 17) | 9 (5; 17) | 12 (9; 21) | 8.5 (5; 17) | 0.340 |
Data are number (percentage column) or median [interquartile range, (IQR)]. Chi-squared test or Kruskal–Wallis P values are shown respectively. ASA=American Society of Anesthesiologists. CHF: congestive heart failure. COPD: chronic obstructive pulmonary disease. CAD: coronary artery disease. GI: gastrointestinal. PACU: post-anaesthetic care unit. LOS: length of stay. P values test the homogeneity of variable distribution (means or percentages) among age groups.
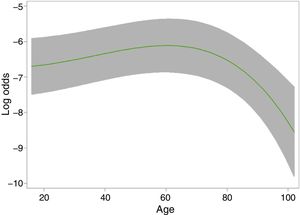
A total of 677 patients (12.5%) were admitted to an ICU postoperatively. Taking as reference the younger group (patients less than 65 years), adjusted OR for ICU admission were 1.1 (95% CI 0.8–1.4) for patients aged 65–74 years, 0.7 (95% CI 0.5–1) for patients aged 75–85 years and 0.4 (95% CI 0.2–0.8) for patients over 85 years, respectively. Fig. 2 shows the relation shape of age with ICU admission through the fractional polynomial regression analysis. As the relationship was not linear, a single coefficient cannot be provided and a plot of age versus combination component described earlier was presented. Differences from this component measured at two different ages are the log odds ratio from one age related to other. ICU admission showed a linear increase up to around 80 years, with a significant decrease in the probability of admission in subsequent years. In multivariable logistic regression analysis, independent risk factors for ICU admission were age, ASA, grade and urgency of surgery, surgical speciality and laparoscopic surgery (Table 2). Among the comorbidities of patients, metastatic disease was the only predictor of ICU admission. When patients were divided into age group by quartile rather than by arbitrary age categories, no differences were found respect the first model multivariable analysis.
Adjusted logistic regression for intensive care unit (ICU) admission.
| ICU admission | Crude OR (95% CI) | Adjusted OR (95% CI) | P value | |
|---|---|---|---|---|
| Age | ||||
| <65 years | 339 (10.6) | 1 | 1 | 0.004 |
| 65–74 years | 181 (16.8) | 1.72 (1.41–2.09) | 1.08 (0.84–1.39) | |
| 75–85 years | 140 (14.5) | 1.41 (1.14–1.75) | 0.73 (0.55–0.97) | |
| >85 years | 17 (9.0) | 0.84 (0.50–1.40) | 0.41 (0.22–0.77) | |
| ASA score | ||||
| I | 40 (3.6) | 1 | 1 | <0.001 |
| II | 249 (9.3) | 2.77 (1.96–3.91) | 1.99 (1.36–2.91) | |
| III | 284 (20.4) | 6.99 (4.95–9.88) | 3.30 (2.19–4.98) | |
| IV | 96 (42.1) | 19.65 (12.99–29.74) | 8.99 (5.23–15.45) | |
| V | 8 (72.7) | 63.72 (15.84–255.75) | 10.02 (1.56–64.42) | |
| Grade of surgery | ||||
| Minor | 12 (1.3) | 1 | 1 | <0.001 |
| Intermediate | 122 (4.5) | 3.65 (2.01–6.65) | 3.76 (2.05–6.91) | |
| Major | 543 (30.5) | 34.09 (19.12–60.75) | 30.93 (17.10–55.95) | |
| Urgency of surgery | ||||
| Elective | 507 (11.4) | 1 | 1 | <0.001 |
| Urgent | 117 (13.5) | 1.21 (0.98–1.51) | 1.06 (0.80–1.40) | |
| Emergency | 53 (46.9) | 6.78 (4.62–9.94) | 4.22 (2.44–7.29) | |
| Surgical speciality | ||||
| Orthopaedics | 71 (4.9) | 1 | 1 | <0.001 |
| Breast | 17 (10.4) | 2.22 (1.27–3.88) | 3.18 (1.71–5.91) | |
| Gynaecology | 26 (5.9) | 1.19 (0.75–1.89) | 1.98 (1.19–3.32) | |
| Vascular | 78 (27.3) | 7.19 (5.05–10.24) | 5.48 (3.59–8.32) | |
| Upper gastrointestinal | 76 (31.8) | 8.90 (6.20–12.78) | 7.39 (4.85–11.33) | |
| Lower gastrointestinal | 131 (19.7) | 4.64 (3.41–6.30) | 4.22 (2.99–6.05) | |
| Hepato-biliary | 64 (20.4) | 4.91 (3.41–7.06) | 5.54 (3.55–8.67) | |
| Plastic | 11 (4.7) | 0.95 (0.50–1.83) | 2.76 (1.36–5.63) | |
| Urology | 63 (10.1) | 2.15 (1.51–3.06) | 2.74 (1.83–4.08) | |
| Kidney | 18 (36) | 10.74 (5.75–20.05) | 4.83 (2.36–9.89) | |
| Head and Neck | 55 (8.5) | 1.77 (1.23–2.55) | 3.49 (2.32–5.25) | |
| Other | 62 (19) | 4.48 (3.11–6.46) | 5.29 (3.45; 8.10) | |
| Metastasic disease | 86 (37.4) | 4.66 (3.52–6.18) | 2.28 (1.61–3.23) | <0.001 |
| Laparoscopic surgery | 84 (12.4%) | 0.99 (0.77–1.26) | 0.68 (0.50; 0.92) | 0.012 |
Data are number (percentage column) and OR (odds ratio) adjusted for other variables in the table and CI (confidence interval). ASA=American Society of Anaesthesiologists.
Most patients (77%) who were admitted to an ICU after surgery were regarded as requiring routine postoperative care. In the fractional polynomial regression analysis, a significant decrease in the probability of admission from 80 years on was observed in the planned ICU admission group but not in the unplanned. Acute abdomen, septic and hypovolemic shock were the most frequent causes of unplanned postoperative ICU admissions (Table 3). When we analysed the different causes of ICU admission by age groups, no significant differences were found except for arrhythmia, which represented a more frequent cause of unplanned ICU admission in the population aged 65–84 years (P=0.025).
Causes of Intensive Care Unit admission among age categories.
| <65 years (n=337) | 65–74 years (n=180) | 75–85 years (n=137) | >85 years (n=17) | Total (n=671) | P value | |
|---|---|---|---|---|---|---|
| Routine care | 265 (78.6%) | 142 (78.9%) | 99 (72.3%) | 12 (70.6%) | 518 (77.2%) | 0.390 |
| Acute abdomen | 36 (10.7%) | 23 (12.8%) | 14 (10.2%) | 3 (17.6%) | 76 (11.3%) | 0.715 |
| Arrhythmia | 2 (0.6%) | 6 (3.3%) | 4 (2.9%) | 1 (5.9%) | 13 (1.9%) | 0.025 |
| Coma | 5 (1.5%) | 0 (0%) | 3 (2.2%) | 1 (5.9%) | 9 (1.3%) | 0.064 |
| Hypovolemic shock | 24 (7.1%) | 10 (5.6%) | 11 (8.0%) | 2 (11.8%) | 47 (7%) | 0.706 |
| Liver failure | 5 (1.5%) | 0 (0%) | 1 (0.7%) | 0 (0%) | 6 (0.9%) | 0.360 |
| Pancreatitis | 1 (0.3%) | 2 (1.1%) | 0 (0%) | 0 (0%) | 3 (0.4%) | 0.350 |
| Septic shock | 20 (5.9%) | 15 (8.3%) | 11 (8.0%) | 2 (11.8%) | 48 (7.1%) | 0.608 |
Data are number (percentage column). Chi squared P values are shown.
The Spanish subset of EuSOS reported a hospital mortality of 3.8%, similar to the European average (4%) (P=0.455). The global risk-adjusted mortality (by age, ASA, cirrhosis, metastatic disease, category, type and emergency surgery) was 1.39 (95% CI 0.89–2.18), with no differences from the reference country in the EuSOS (P=0.15). In the adjusted model for hospital and patient characteristics, no differences in hospital mortality were found among Spanish hospitals with and OR of 1.41 (95% CI 0.90–2.21) (P=0.13). Notably, and in contrast to the European cohort, age was not a predictor of hospital mortality. When we analysed mortality upon age groups, 3.4% was found in the group of less than 65 years, 3.8% in patients aged 65–74 years, 4.9% in patients aged 75–85 years and 4.2% in patients over 85 years (P=0.220). Adjusted OR for hospital mortality was 1.1 (95% CI 0.7–1.7) for patients aged 65–74 years, 1.3 (95% CI 0.9–2.1) for patients aged 75–85 years and 1.0 (95% CI 0.5–2.4) for patients over 85 years, respectively. Modelling the “age” category as a continuous rather than a categorical one, no correlation with hospital mortality was found either. Multivariable regression analysis identified ASA, urgent or emergency surgery, surgical speciality and insulin-dependent diabetes as predictors of hospital mortality (Table 4). Unlike the European cohort, grade of surgery (P=0.806), liver cirrhosis (P=0.336) and metastatic disease (P=0.086) were neither associated with a higher mortality in the Spanish subset of EuSOS. Among patients admitted to the ICU, mortality was higher in unplanned admissions (6.4% vs 18.2%, P=0.001). Most patients who died had not previously been admitted to the ICU (144 of 208 deceased patients had never been previously admitted to an ICU).
Adjusted logistic regression for hospital mortality.
| Hospital mortality | Crude OR (95% CI) | Adjusted OR (95% CI) | P value | |
|---|---|---|---|---|
| ASA score | ||||
| I | 45 (4.0%) | 1 | 1 | <0.001 |
| II | 70 (2.6%) | 0.61 (0.42–0.90) | 0.59 (0.39–0.90) | |
| III | 53 (3.8%) | 0.93 (0.62–1.40) | 0.71 (0.42–1.20) | |
| IV | 32 (14.0%) | 3.86 (2.39–6.23) | 2.20 (1.14–4.26) | |
| V | 8 (72.7%) | 54.91 (13.75–219.36) | 17.81 (3.80–83.59) | |
| Urgency of surgery | ||||
| Elective | 139 (3.1%) | 1 | 1 | <0.001 |
| Urgent | 48 (5.5%) | 1.85 (1.32–2.59) | 1.44 (0.99–2.09) | |
| Emergency | 21 (18.6%) | 6.82 (4.09–11.39) | 3.31 (1.77–6.19) | |
| Surgical speciality | ||||
| Orthopaedics | 36 (2.5%) | 1 | 1 | <0.001 |
| Breast | 4 (2.4%) | 0.97 (0.34–2.76) | 1.30 (0.45–3.75) | |
| Gynaecology | 26 (5.9%) | 2.41 (1.44–4.03) | 3.29 (1.88–5.76) | |
| Vascular | 20 (7.0%) | 2.91 (1.66–5.11) | 1.78 (0.95–3.33) | |
| Upper gastrointestinal | 20 (8.4%) | 3.53 (2.00–6.20) | 3.45 (1.88–6.33) | |
| Lower gastrointestinal | 33 (5%) | 2.02 (1.25–3.26) | 1.57 (0.94–2.64) | |
| Hepato-biliary | 14 (4.5%) | 1.81 (0.96–3.39) | 1.91 (0.96–3.80) | |
| Plastic | 5 (2.2%) | 0.85 (0.33–2.20) | 0.96 (0.37–2.51) | |
| Urology | 20 (3.2%) | 1.28 (0.74–2.23) | 1.46 (0.81–2.62) | |
| Kidney | 1 (2%) | 0.79 (0.11–5.87) | 0.70 (0.09–5.51) | |
| Head and neck | 17 (2.6%) | 1.04 (0.58–1.87) | 1.24 (0.68–2.27) | |
| Other | 9 (2.8%) | 1.10 (0.52–2.30) | 1.04 (0.48–2.26) | |
| Diabetes insulin-dependent | 22 (8.7%) | 1.02 (0.64–1.61) | 2.08 (1.22–3.53) | 0.007 |
Data are number (percentage column) and OR (odds ratio) and CI (confidence interval). ASA=American Society of Anaesthesiologists.
A comparison of the general characteristics of patients in the EuSOS and the Spanish subset is shown in Table 5.
Characteristics of the Spanish and the EuSOS cohorts.
| EuSOS Spain (n=5433) | EuSOS (n=46,539) | P value | |
|---|---|---|---|
| Age (years) | 58.4±17.8 | 56.7±18.5 | <0.001 |
| Men | 2699 (49.7%) | 22,618 (48.6%) | 0.126 |
| Smoker | 1192 (21.9%) | 9261 (19.9%) | <0.001 |
| ASA score | |||
| I | 1112 (20.5%) | 11,642 (25%) | <0.001 |
| II | 2690 (49.5%) | 21,582 (46.4%) | <0.001 |
| III | 1392 (25.6%) | 11,574 (24.9%) | 0.257 |
| IV | 228 (4.2%) | 1559 (3.3%) | <0.001 |
| V | 11 (0.2%) | 90 (0.4%) | <0.001 |
| Comorbidities | |||
| Cirrhosis | 83 (1.5%) | 512 (1.1%) | 0.010 |
| CHF | 169 (3.1%) | 2141 (4.6%) | <0.001 |
| COPD | 615 (11.3%) | 5166 (11.1%) | 0.656 |
| CAD | 420 (7.7%) | 6283 (13.5%) | <0.001 |
| Diabetes (no insulin) | 548 (10.1%) | 2094 (4.5%) | <0.001 |
| Diabetes (insulin) | 255 (4.7%) | 3490 (7.5%) | <0.001 |
| Metastatic disease | 230 (4.2%) | 2187 (4.7%) | <0.001 |
| Stroke | 244 (4.5%) | 2001 (4.3%) | 0.511 |
| Grade of surgery | |||
| Minor | 950 (17.5%) | 12,054 (25.9%) | <0.001 |
| Intermediate | 2701 (49.7%) | 22,246 (47.8%) | 0.008 |
| Major | 1782 (32.8%) | 12,193 (26.2%) | <0.001 |
| Urgency of surgery | |||
| Elective | 4453 (82%) | 35,044 (75.3%) | <0.001 |
| Urgent | 597 (16%) | 8935 (19.2%) | <0.001 |
| Emergent | 113 (2.1%) | 2560 (5.5%) | <0.001 |
| Surgical speciality | |||
| Orthopaedics | 1431 (26.4%) | 12,193 (26.2%) | <0.001 |
| Breast | 163 (3.0%) | 1489 (3.2%) | |
| Gynaecology | 443 (8.2%) | 3956 (8.5%) | |
| Vascular | 286 (5.3%) | 2373 (5.1%) | |
| Upper GI | 239 (4.4%) | 2234 (4.8%) | |
| Lower GI | 666 (12.3%) | 4980 (10.7%) | |
| Hepatobiliary | 313 (5.8%) | 2234 (4.8%) | |
| Plastic | 232 (4.3%) | 2420 (5.2%) | |
| Urology | 623 (11.5%) | 4887 (10.5%) | |
| Kidney | 50 (0.9%) | 465 (1%) | |
| Head and neck | 648 (11.9%) | 5631 (12.1%) | |
| Other | 326 (6.0%) | 3444 (7.4%) | |
| Hospital stay (days) | 3 (1.0–7.0) | 3.0 (1.0–7.0) | >0.99 |
| ICU admission | 679 (12.5%) | 3723 (8%) | <0.001 |
| ICU stay (days) | 1.0 (0.9–2.1) | 1.2 (0.9–3.6) | 1.000 |
| Hospital Mortality | 208 (3.8%) | 1855 (4%) | 0.455 |
Data are number (percentage column) or median [interquantile range, (IQR)]. Chi-squared test or Kruskall–Wallis P values are shown respectively. ASA=American Society of Anesthesiologists. CHF: congestive heart failure. COPD: chronic obstructive pulmonary disease. CAD: coronary artery disease. GI: gastrointestinal.
The main finding of this study was that elderly were less likely to be admitted to intensive care after surgery than younger patients. Interestingly, there was no significant association between age and mortality.
Despite being considered a high-risk population, the likelihood of ICU admission was not greater in our elderly patients. The role of PACUs as providers of postoperative intensive care could represent a possible explanation to this negative finding. Our elderly had higher PACU stay than younger patients, suggesting that a more prolonged PACU LOS could account for a lower ICU admission. Lowest rate of ICU admission has been reported in countries where PACUs act as high-dependency units.18 However, both our overall median PACU LOS and patients remaining more than 12h were much lower than the ones reported in the Swedish subset of the EuSOS (120 vs 175min and 3.6 vs 6.6%, respectively).18 Perioperative care facilities obtained once for each participating hospital did not include PACU opening hours. Definition of PACU as was stated in the main EuSOS paper could include different models depending upon countries and this could have lead to some inaccuracy when defining resources. It is likely that in Spain most PACUs do not actually provide continued 24h assistance, but are rather recovery areas with opening hours parallel to surgical schedule, a fact that could explain the higher overall ICU requirement.
Another explanation of why elderly patients were less admitted to the ICU could have been non-written age limitation. Although intensive care use in the very elderly has been questioned for their unfavourable results,6,7 age alone seems to be a poor indicator of the possible value to be gained from an ICU admission.19 The ELDICUS study was the first to demonstrate a greater survival benefit from ICU admission, surprisingly not in younger patients but older patients.20 Recent guidelines suggest basing the decision to admit an elderly (>80yr) patient to an ICU on the patient's comorbidities, severity of illness, prehospital functional status, and patient preferences with regard to life-sustaining treatment, not on their chronological age.21 In our series, 42.3% of patients over 85 years were from a single surgical speciality (orthopaedics). Hip fractures usually account for almost half of all surgical volume in this population and patients and are not routinely admitted to ICU after surgery.
The EuSOS did not include data on resuscitation orders or use of palliative surgery for disseminated malignant diseases. For these patients with a poor prognosis, postoperative admission to critical care might have been deemed inappropriate and may have influenced decisions to potentially underuse ICU care in older patients. However, our data suggest that these cases are few in number (only 4.2% of patients had malignancy) and was more frequent in patients aged 65–74 years (Table 1). Among the comorbidities of patients, metastatic disease was the only predictor of ICU admission. Bos et al.22 have reported low elective cancer surgery mortality rates, with ICU and hospital mortalities of 1% and 5%, respectively. Recent guidelines suggest that ICU access of cancer patients should be decided on the basis of their severity of illness and long-term prognosis, rather than on the basis of the presence of a malignancy or metastasis.21
Finally, other institutional factors, like differences in hospitals structures or quality of ward-care based, could have also influenced surgeons to treat their patients outside the ICU.23 EuSOS dataset did neither include staffing on surgical wards, which could also impact on ICU admission. Greater use of ICU does not improve clinical outcomes for certain medical conditions, suggesting that equivalent care can be delivered elsewhere in the hospital.24
In our study, age was not a predictor of hospital mortality, which itself was associated with other known risk factors such as ASA score, urgency of surgery and surgical speciality. According to various studies, elderly patients are at increased risk of short-term postoperative mortality.14,18,25,26 However, the role of age in the accumulation of morbidities can be a greater predictor of mortality than chronological age.27–31 Our older patients were those with higher ASA scores, a fact that might suggest a greater existence of preoperative comorbidities. Yet, the ASA classification has been criticised for including a significant component of subjective clinical judgement and other index have been validated as a predictor of perioperative outcomes after acute surgical care.27,32 Urgency of surgery could also be a much better predictor of mortality than chronological age.33 Not surprisingly, similarly to previous national's results,34 mortality of patients undergoing urgent and emergency surgery was 5.5% and 18.6%, respectively, contrasting with 3.1% mortality in elective surgery. According to the literature,33,35 our patients’ need for urgent surgery increased with age. However, the global percentage of urgent or emergent surgery in the Spanish cohort (18%) was lower than in the EuSOS (24.7%).14
Strengths and limitations of the study should be commented on. The sample size and the number of participating hospitals seem broad enough to reflect national practice. In this regard, homogeneity in hospital mortality between different hospitals is noteworthy. Given that 30% of hospitals were not university hospitals, this suggests that postoperative care in Spain is relatively standardised, with no significant territorial differences depending on the type and size of the hospital. The effects attributed to age in our report could be due to other factors. The main limitations of our study are we did not measure patients’ frailty or postoperative complications. Frailty is not synonymous with being elderly and the use of preoperative specific frailty scales, or even some biomarkers, might be useful in predicting surgical outcomes.36–38 Likewise our study did not include complications following surgery, which probably accounted for unmeasured confounding results. Age significantly affects the risk for perioperative complications after non-cardiac surgery and surgical complications are a frequent cause of postoperative death.39,40 In our study, most patients who died had not previously been admitted to the ICU (144 of 208 deceased patients had never been previously admitted to an ICU). This could be attributed to the so-called “failure to rescue”, case-fatality rates after complications that are highly correlated with surgical mortality.41 A significant number of complications appear beyond the first 48h of the intervention, so patients admitted to an ICU could remain at risk of developing complications following ICU discharge. Research is required to identify patients in non-critical care areas at risk of deterioration. Finally, we did not perform a long-term follow up of our patients. Although differences on long-term mortality seem unlikely related to planned postoperative ICU admission, a five-fold overall increase in postoperative one-year mortality compared to 30-day mortality has been described,18 suggesting that the unseen differences in hospital mortality between age groups could turn out positive in long-term mortality.
In summary, this study shows that age significantly affects the likelihood of postoperative intensive care provision after non-cardiac surgery. Elderly patients (over 80 years) were at lower risk for ICU admission. However, this lower rate of ICU admission did not affect hospital mortality, which was independent of age strata. The role of PACUs or ward-care based may be associated with age and affect outcomes after surgery. Further studies are needed to clarify the safest and effective postoperative care pathway for elderly population.
Authors’ contributionsMdN analysed and interpreted the data. She made several drafts of the manuscript text body, the tables and figures and revised these several times critically. SPH did the statistical analyses, the tables and the figures. JCMG, CA and RP revised the manuscript critically. CA and RP made a major contribution to the design and interpretation of the data. All authors read and approved the final manuscript.
Financial support and sponsorshipEuSOS was funded by the European Society of Intensive Care Medicine and the European Society of Anaesthesiology.
Conflicts of interestRP holds research grants, and has given lectures and/or performed consultancy work for Nestle Health Sciences, BBraun, Medtronic, and Edwards Lifesciences, and is a member of the Associate editorial board of the British Journal of Anaesthesia. All other authors certify that there is no conflict of interest with any financial organisation regarding the material discussed in the manuscript.
Presented in part at 2017 Euroanesthesia Congress (Geneva, 3–5 June 2017).
The authors thank Marta Pulido, MD, for editing the manuscript and editorial assistance.