To describe the morbimortality associated to the development of acute kidney injury (AKI) defined by the pediatric adaptation of the RIFLE criteria in a Pediatric Intensive Care Unit (PICU).
DesignA retrospective cohort study was carried out.
SettingChildren admitted to a PICU in a tertiary care hospital.
Patients or participantsA total of 320 children admitted to a tertiary care hospital PICU during the year 2011. Neonates and renal transplant patients were excluded.
Primary endpointsAKI was defined and classified according to the pediatric adaptation to the RIFLE criteria. PICU and hospital stays, use of mechanical ventilation and mortality were used to evaluate morbimortality.
ResultsA total of 315 children met the inclusion criteria, with a median age of 19 months (range 6–72). Of these patients, 128 presented AKI (73 reached the Risk category and 55 reached the injury and failure categories). Children with AKI presented a longer PICU stay (6.0 [4.0–12.5] vs 3.5 [2.0–7.0] days) and hospital stay (17 [10–32] vs 10 [7–15] days), and a greater need for mechanical ventilation (61.7 vs 36.9%). The development of AKI was an independent factor of morbidity, associated with a longer PICU and hospital stay, and with a need for longer mechanical ventilation, with a proportional relationship between increasing morbidity and the severity of AKI.
ConclusionThe development of AKI in critically ill children is associated with increased morbimortality, which is proportional to the severity of renal injury.
Analizar la morbimortalidad asociada a daño renal agudo (DRA) definido por los criterios RIFLE adaptados a Pediatría en los niños que ingresan en la Unidad de Cuidados Intensivos Pediátricos (UCIP).
DiseñoEstudio retrospectivo de cohorte.
ÁmbitoUCIP de un hospital terciario.
Pacientes o participantesTrescientos veinte niños ingresados en la UCIP en el año 2011. Se excluyeron los neonatos y los trasplantados renales.
Variables principalesEl DRA fue definido con los criterios RIFLE adaptados a Pediatría. Para la valoración de la morbimortalidad se utilizó la duración de las estancias en la UCIP y en el hospital, la necesidad de ventilación mecánica y la mortalidad.
ResultadosSe estudiaron 315 niños, con una mediana de edad de 19 meses (6-72). Presentaron DRA 128 niños (40,6%) (73 en la categoría de Risk [riesgo] y 55 en las categorías Injury [daño] y Failure [fallo]). Los niños con DRA presentaron mayor mortalidad (11,7%) que el resto de pacientes (0,5%), una estancia más prolongada en UCIP (6,0 [4,0-12,5] frente a 3,5 [2,0-7,0] días) y en el hospital (17 (10-32) frente a 10 (7-15] días) y más niños precisaron ventilación mecánica (61,7 frente a 36,9%). El desarrollo de DRA fue un factor independiente de morbilidad, asociado a una mayor estancia en UCIP y hospitalaria y a una ventilación mecánica más prolongada, incrementándose esta morbilidad de forma paralela a la gravedad del daño renal.
ConclusiónEl desarrollo de DRA en niños en estado crítico se asocia a un incremento en la morbimortalidad, que es directamente proporcional a la magnitud de la gravedad del daño renal.
Acute kidney injury (AKI) in the pediatric patient is an important problem, particularly in critically ill subjects requiring admission to the Pediatric Intensive Care Unit (PICU).
AKI is a clinical syndrome characterized by a loss or sudden decrease in kidney function, with or without associated oligoanuria, and with nonspecific clinical manifestations that can include water–electrolyte imbalances.1
The incidence and severity of AKI vary greatly due to the lack of universally accepted diagnostic criteria.1,2 Indeed, there are as many as 30 different definitions of AKI. This helps explain the enormous differences in the reported incidence of AKI in the PICU (2.5–24%),3 and makes it difficult to establish comparisons of the incidence and morbidity associated to AKI.4,5
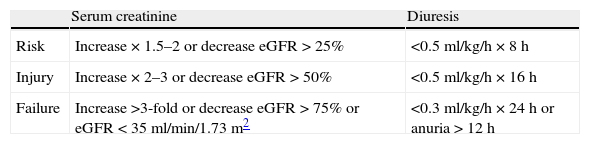
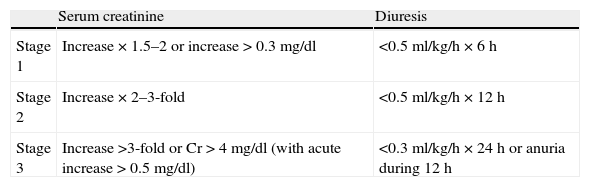
In recent years there have been improvements in the standardization of the diagnosis of AKI in the pediatric patient, with adoption of the pRIFLE criteria as main definition6 (Table 1). These criteria imply a slight modification of the RIFLE criteria described for adult patients.7 Application of the posterior AKIN criteria8 (Table 2) has revealed no relevant differences with respect to the pRIFLE criteria.5
RIFLE criteria of acute kidney injury adapted to pediatric patients.
| Serum creatinine | Diuresis | |
| Risk | Increase×1.5–2 or decrease eGFR>25% | <0.5ml/kg/h×8h |
| Injury | Increase×2–3 or decrease eGFR>50% | <0.5ml/kg/h×16h |
| Failure | Increase >3-fold or decrease eGFR>75% or eGFR<35ml/min/1.73m2 | <0.3ml/kg/h×24h or anuria>12h |
eGFR: estimated glomerular filtration rate.
In adult patients, on adopting both the RIFLE criteria and the posterior AKIN criteria,9–13 a relationship has been established between the development of AKI and patient morbidity–mortality, the latter being directly proportional to the severity of kidney injury.
However, in the pediatric patient, this relationship has not been consistently demonstrated, probably because of the few studies carried out to date and the small sample sizes involved.
The main aim of this study was to evaluate morbidity–mortality among children admitted to the PICU who develop AKI as defined and classified by the pRIFLE criteria.
Material and methodsA retrospective, observational cohort study was carried out, based on the review of case histories and including all patients over one month of age and under 15 years of age admitted to the PICU of Gregorio Marañón University General Hospital (Madrid, Spain) during the year 2011. We excluded newborn infants and patients admitted in the postoperative period of kidney transplantation. The study was approved by the Clinical Research Ethics Committee of the hospital.
The following variables were collected: age, gender, weight and reason for admission (grouped as the postoperative period of heart surgery, decompensation of heart disease unrelated to surgery, the postoperative period of other types of surgery, acute respiratory failure, and others).
As morbidity indicators, we considered the need for invasive mechanical ventilation and its duration, the duration of stay both in the PICU and in hospital, and mortality.
We also documented extracorporeal membrane oxygenation (ECMO) and renal replacement therapy (peritoneal dialysis or continuous renal replacement therapy), including the day of admission corresponding to the start of each technique, and its duration.
Renal function was assessed on the basis of repeated blood creatinine measurements and diuresis.
Kidney injury was defined and categorized using the pediatric adaptation of the RIFLE criteria (Table 1). The glomerular filtration rate was estimated from the Schwartz formula: eGFR=K×height (cm)/creatinine concentration (mg/dl). The K value depends on the age: 0.45 in patients ≤12 months, 0.55 in those between 1 and 12 years, 0.57 in females >of 12 years and 0.70 in males >12 years. We used the first three severity categories of the RIFLE, obviating categories L and E because they refer to the end outcome rather than to an acute change. Severe AKI was considered in those situations meeting the criteria of categories I or F of the pRIFLE classification.
In the absence of a basal creatinine value with which to evaluate the evolutive changes for the categorization of AKI, we proceeded as follows: if the patient had a creatinine value in the 6 months prior to admission we used that value, provided it had not been obtained in the first month of life; and if no known creatinine value was available, we made use of the recent reference values for infants and children.14,15
Likewise, we recorded the time of kidney injury and its duration. Early AKI was defined as AKI developing in the first 72h after admission to the PICU (representing AKI probably related to the cause of admission), while late AKI was taken to be AKI manifesting after that time (and possibly more related to complications of the initial disease or of prolonged admission to the PICU). Prerenal injury was considered when the condition resolved in under 72h, while prolonged kidney injury was considered if it persisted for 72h or longer.16,17
In order to assess morbidity, we analyzed the need for mechanical ventilation and its duration, the duration of admission to the PICU and of admission to hospital, and patient mortality. Prolonged admission to the PICU was defined as a stay of over 12 days,18,19 while prolonged hospital admission was defined as a stay of over 28 days. In turn, prolonged mechanical ventilation was taken to represent mechanical ventilation during more than 7 days.
The patients that died were excluded from the analysis of the duration of stay and of mechanical ventilation. The five children with mechanical ventilation for more than 42 days were assigned a value of 1000h.
The data were processed using the SPSS® version 18.0 statistical package. The normal distribution of the quantitative variables was assessed using the Kolmogorov–Smirnov test. The data are reported as medians (P25–P75) and frequencies and percentages. Comparison of the qualitative variables was carried out using the chi-squared test and the Fisher exact test where required, while the quantitative variables were compared with the Mann–Whitney U test.
The association of AKI to patient morbidity–mortality was explored by univariate and multivariate logistic regression analysis, constructing models adjusted for age, diagnosis and duration of mechanical ventilation, while models adjusted for age and diagnosis were used in the analysis of the duration of mechanical ventilation.
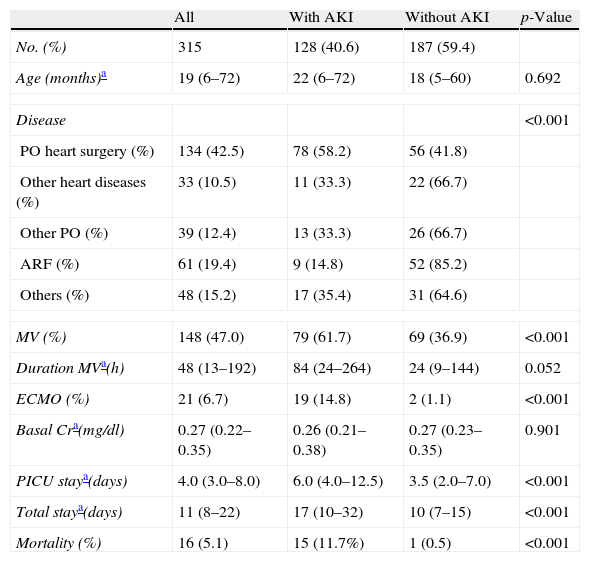
ResultsDuring the study period, a total of 320 patients over one month of age were admitted to the PICU. Of these, 5 were excluded because they had undergone kidney transplantation, thereby leaving 315 patients for inclusion in the study. The demographic characteristics are shown in Table 3.
Basal characteristics of the study population.
| All | With AKI | Without AKI | p-Value | |
| No. (%) | 315 | 128 (40.6) | 187 (59.4) | |
| Age (months)a | 19 (6–72) | 22 (6–72) | 18 (5–60) | 0.692 |
| Disease | <0.001 | |||
| PO heart surgery (%) | 134 (42.5) | 78 (58.2) | 56 (41.8) | |
| Other heart diseases (%) | 33 (10.5) | 11 (33.3) | 22 (66.7) | |
| Other PO (%) | 39 (12.4) | 13 (33.3) | 26 (66.7) | |
| ARF (%) | 61 (19.4) | 9 (14.8) | 52 (85.2) | |
| Others (%) | 48 (15.2) | 17 (35.4) | 31 (64.6) | |
| MV (%) | 148 (47.0) | 79 (61.7) | 69 (36.9) | <0.001 |
| Duration MVa(h) | 48 (13–192) | 84 (24–264) | 24 (9–144) | 0.052 |
| ECMO (%) | 21 (6.7) | 19 (14.8) | 2 (1.1) | <0.001 |
| Basal Cra(mg/dl) | 0.27 (0.22–0.35) | 0.26 (0.21–0.38) | 0.27 (0.23–0.35) | 0.901 |
| PICU staya(days) | 4.0 (3.0–8.0) | 6.0 (4.0–12.5) | 3.5 (2.0–7.0) | <0.001 |
| Total staya(days) | 11 (8–22) | 17 (10–32) | 10 (7–15) | <0.001 |
| Mortality (%) | 16 (5.1) | 15 (11.7%) | 1 (0.5) | <0.001 |
Cr: creatinine; AKI: acute kidney injury; ECMO: extracorporeal membrane oxygenation; PO: postoperative period; ARF: acute respiratory failure; PICU: Pediatric Intensive Care Unit; MV: mechanical ventilation.
The postoperative period of heart surgery was the most common cause of admission to the PICU (134 children, 42.5%). As can be seen in Table 3, a total of 148 children (47%) required mechanical ventilation, with a duration of 48h (13–192). The duration of stay in the PICU was 4 days (3–8), while the total duration of hospital stay was 11 days (8–22). Fifty-nine children (18.7%) had no known basal creatinine value, and in these cases we used a reference creatinine value adjusted for age.
Of the 315 children, 40.6% (128 children) suffered AKI at some point during admission, and of these 107 (83.6%) developed early AKI.
In relation to the diagnosis, AKI was more frequent in children subjected to heart surgery, being recorded in 78 of them (58.2%) (this representing 60.9% of the total cases of AKI) (Table 3).
The patients with AKI required mechanical ventilation significantly more often (61.7%) than the rest of the children admitted to the PICU, and the duration of mechanical ventilation was also longer. Likewise, there was a greater need for extracorporeal membrane oxygenation in the children with AKI (Table 3).
The children who developed AKI presented a significantly longer stay both in the PICU and in hospital, and also showed a higher mortality rate (Table 3).
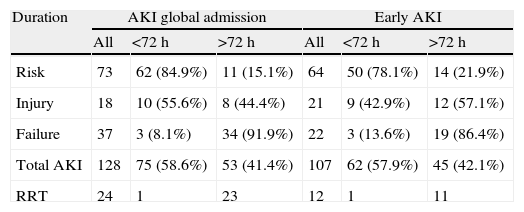
Table 4 categorizes AKI according to onset, severity and duration. A total of 58.6% of the patients presented prerenal AKI. An association was found between the severity and duration of AKI – a larger number of mild cases being found in prerenal AKI, while the more severe categories were associated to a longer duration of AKI (Table 4).
Distribution of acute kidney injury according to severity, start and duration.
| Duration | AKI global admission | Early AKI | ||||
| All | <72h | >72h | All | <72h | >72h | |
| Risk | 73 | 62 (84.9%) | 11 (15.1%) | 64 | 50 (78.1%) | 14 (21.9%) |
| Injury | 18 | 10 (55.6%) | 8 (44.4%) | 21 | 9 (42.9%) | 12 (57.1%) |
| Failure | 37 | 3 (8.1%) | 34 (91.9%) | 22 | 3 (13.6%) | 19 (86.4%) |
| Total AKI | 128 | 75 (58.6%) | 53 (41.4%) | 107 | 62 (57.9%) | 45 (42.1%) |
| RRT | 24 | 1 | 23 | 12 | 1 | 11 |
AKI: acute kidney injury; RRT: use of renal replacement therapy.
AKI global admission: presence of AKI at any time during admission. Early AKI: start within first 72h of admission.
Twenty-one children without early AKI developed AKI at a later point (prerenal in 13 and after >72h in 8 cases).
The criterion oliguria was found in very few patients: one patient with uremic hemolytic syndrome who developed anuria from admission together with creatinine 4.09mg/dl (both criteria of Failure being met) and two children with severe cardiac dysfunction requiring treatment with extracorporeal membrane oxygenation, followed by renal replacement therapy. Another 20 children in which renal replacement therapy was indicated due to water overload with altered creatinine levels and glomerular filtration met the oliguria criterion, though once renal replacement therapy had already started.
Twenty-four children (18.7% of the total patients with AKI) required renal replacement therapy (continuous renal replacement therapy in 23 cases and peritoneal dialysis in one patient). The mortality rate among the patients with severe AKI (Injury or Failure) was 23.7%–this being far higher than the mortality rate among those with mild AKI (Risk) (2.7%) or the children without AKI (0.5%) (p<0.001).
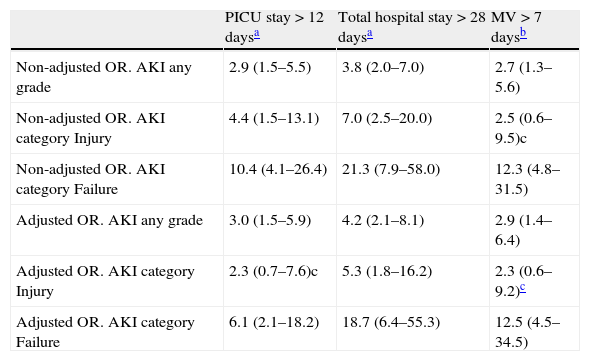
A very significant association was observed between AKI and a prolonged stay in the PICU and in hospital, and the need for prolonged mechanical ventilation. This association was found to be independent of the age and disease condition of the patients, after controlling for these variables in the multivariate logistic regression analysis (Table 5). Furthermore, a parallel increase in morbidity–mortality was recorded with increasing severity of AKI (Table 5).
Association between morbidity and the development of acute kidney injury of any grade or in its severe forms (categories Injury and Failure).
| PICU stay>12 daysa | Total hospital stay>28 daysa | MV>7 daysb | |
| Non-adjusted OR. AKI any grade | 2.9 (1.5–5.5) | 3.8 (2.0–7.0) | 2.7 (1.3–5.6) |
| Non-adjusted OR. AKI category Injury | 4.4 (1.5–13.1) | 7.0 (2.5–20.0) | 2.5 (0.6–9.5)c |
| Non-adjusted OR. AKI category Failure | 10.4 (4.1–26.4) | 21.3 (7.9–58.0) | 12.3 (4.8–31.5) |
| Adjusted OR. AKI any grade | 3.0 (1.5–5.9) | 4.2 (2.1–8.1) | 2.9 (1.4–6.4) |
| Adjusted OR. AKI category Injury | 2.3 (0.7–7.6)c | 5.3 (1.8–16.2) | 2.3 (0.6–9.2)c |
| Adjusted OR. AKI category Failure | 6.1 (2.1–18.2) | 18.7 (6.4–55.3) | 12.5 (4.5–34.5) |
AKI: acute kidney injury; OR: odds ratio; PICU: Pediatric Intensive Care Unit; MV: mechanical ventilation.
Logistic regression analysis, odds ratio (95% CI).
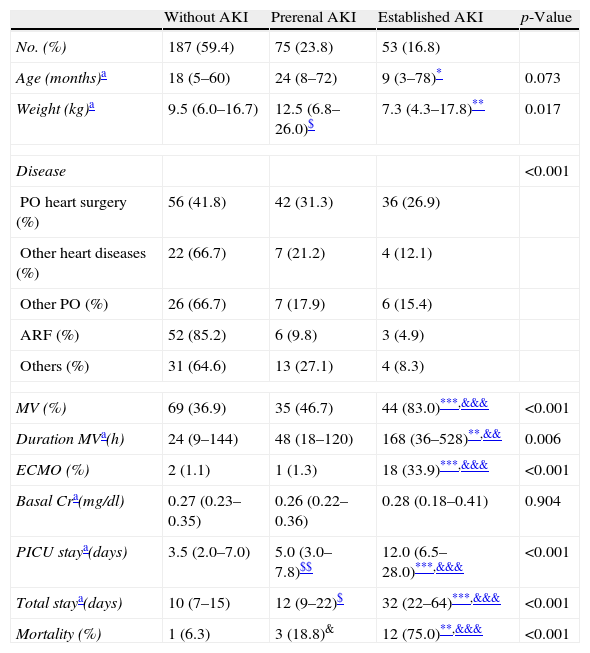
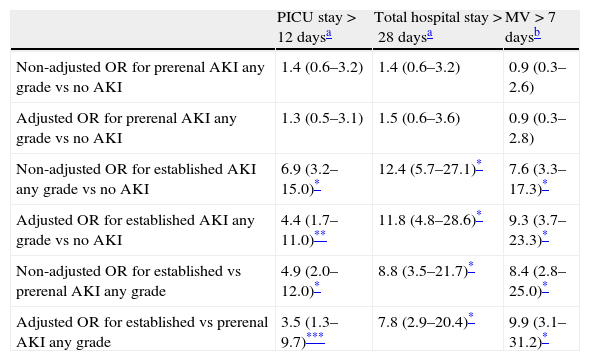
We subsequently conducted a separate study of the children with prerenal AKI versus those with more prolonged AKI (Table 6). The patients with prerenal AKI had a longer stay in the PICU and in hospital than those without AKI, though the use and duration of mechanical ventilation did not differ. As can be seen in Table 6, the children with established AKI were younger and had greater morbidity–mortality than the children without AKI or those with prerenal AKI. A very significant association was observed between established AKI and a prolonged stay in the PICU and in hospital, and the need for prolonged mechanical ventilation, that was moreover independent of patient age or disease condition (Table 7). No such association could be established for the children with prerenal AKI.
Basal characteristics and morbidity according to the presence of prerenal or established acute kidney injury.
| Without AKI | Prerenal AKI | Established AKI | p-Value | |
| No. (%) | 187 (59.4) | 75 (23.8) | 53 (16.8) | |
| Age (months)a | 18 (5–60) | 24 (8–72) | 9 (3–78)* | 0.073 |
| Weight (kg)a | 9.5 (6.0–16.7) | 12.5 (6.8–26.0)$ | 7.3 (4.3–17.8)** | 0.017 |
| Disease | <0.001 | |||
| PO heart surgery (%) | 56 (41.8) | 42 (31.3) | 36 (26.9) | |
| Other heart diseases (%) | 22 (66.7) | 7 (21.2) | 4 (12.1) | |
| Other PO (%) | 26 (66.7) | 7 (17.9) | 6 (15.4) | |
| ARF (%) | 52 (85.2) | 6 (9.8) | 3 (4.9) | |
| Others (%) | 31 (64.6) | 13 (27.1) | 4 (8.3) | |
| MV (%) | 69 (36.9) | 35 (46.7) | 44 (83.0)***,&&& | <0.001 |
| Duration MVa(h) | 24 (9–144) | 48 (18–120) | 168 (36–528)**,&& | 0.006 |
| ECMO (%) | 2 (1.1) | 1 (1.3) | 18 (33.9)***,&&& | <0.001 |
| Basal Cra(mg/dl) | 0.27 (0.23–0.35) | 0.26 (0.22–0.36) | 0.28 (0.18–0.41) | 0.904 |
| PICU staya(days) | 3.5 (2.0–7.0) | 5.0 (3.0–7.8)$$ | 12.0 (6.5–28.0)***,&&& | <0.001 |
| Total staya(days) | 10 (7–15) | 12 (9–22)$ | 32 (22–64)***,&&& | <0.001 |
| Mortality (%) | 1 (6.3) | 3 (18.8)& | 12 (75.0)**,&&& | <0.001 |
Cr: creatinine; AKI: acute kidney injury; ECMO: extracorporeal membrane oxygenation; PO: postoperative period; ARF: acute respiratory failure; PICU: Pediatric Intensive Care Unit; MV: mechanical ventilation.
Association between morbidity and the development of prerenal and established acute kidney injury of any grade.
| PICU stay>12 daysa | Total hospital stay>28 daysa | MV>7 daysb | |
| Non-adjusted OR for prerenal AKI any grade vs no AKI | 1.4 (0.6–3.2) | 1.4 (0.6–3.2) | 0.9 (0.3–2.6) |
| Adjusted OR for prerenal AKI any grade vs no AKI | 1.3 (0.5–3.1) | 1.5 (0.6–3.6) | 0.9 (0.3–2.8) |
| Non-adjusted OR for established AKI any grade vs no AKI | 6.9 (3.2–15.0)* | 12.4 (5.7–27.1)* | 7.6 (3.3–17.3)* |
| Adjusted OR for established AKI any grade vs no AKI | 4.4 (1.7–11.0)** | 11.8 (4.8–28.6)* | 9.3 (3.7–23.3)* |
| Non-adjusted OR for established vs prerenal AKI any grade | 4.9 (2.0–12.0)* | 8.8 (3.5–21.7)* | 8.4 (2.8–25.0)* |
| Adjusted OR for established vs prerenal AKI any grade | 3.5 (1.3–9.7)*** | 7.8 (2.9–20.4)* | 9.9 (3.1–31.2)* |
AKI: acute kidney injury; OR: odds ratio; PICU: Pediatric Intensive Care Unit; MV: mechanical ventilation.
Logistic regression analysis, odds ratio (95% CI).
The results of our study indicate a close association between the development of AKI and morbidity–mortality among children admitted to the PICU. Likewise, morbidity–mortality risk is seen to increase with the severity of AKI.
Few studies have examined the repercussion of AKI in children.5 A recent systematic review5 has reported a lack of concordance among the data published by the different studies–this in part being due to heterogeneous application of the criteria of AKI, differences in the inclusion and exclusion criteria used, and variability in the type of patients studied.20–25
The use of homogeneous and common criteria for the definition of AKI in the pediatric population should allow adequate comparison of the results obtained by different studies. The pRIFLE criteria could be used for this purpose, but their heterogeneous application in the different studies published to date remains an obstacle in this respect.5
In our study we included all critical children requiring admission to the PICU, independently of the type of disease condition involved or of whether admission was decided on an emergency basis or was scheduled. This approach affords a better idea of the magnitude of the problem posed by the development of AKI upon morbidity–mortality in the general pediatric population.
Another limitation of the published studies is the variability of the method used to determine the reference serum creatinine value when creatinine is not known. Some publications even fail to specify this value.25–28 In our series many patients had previous creatinine values, and in the rest of the cases we used recently published reference values.14,15
The oliguria criterion has not been used in the main studies on AKI in children.22–24,29 In our study the oliguria criterion was met in few cases. A probable influencing factor in this sense is the fact that a given diuresis value (ml/kg/h) used to define oliguria becomes an increasingly strict criterion as the patient weight or size decreases, since the water supply received by the child in relation to body weight increases notoriously as the patient size decreases. An evaluation in ml/m2 body surface or ml/1.73m2, i.e., adjusting for body size, would probably resolve this problem. The evaluation of oliguria can also be influenced by the difficulty in quantifying diuresis in non-catheterized children, particularly when carried out on a retrospective basis. Furthermore, the use of diuretics is a common practice in children admitted to the PICU, influenced by the large percentage of patients with heart disease (53% in our series), and this can also contribute to lesser compliance with the oliguria criterion.
Of the 12 published studies attempting to relate the development of AKI to morbidity–mortality, only two contribute sufficient information to confirm that the measures used to define the presence of kidney injury reflect correct application of the pRIFLE criteria.6,20
Several studies have reported a relationship between the existence of AKI and patient mortality,20,21,29 in coincidence with our own findings. Of the four articles analyzing mortality in relation to severity according to the pRIFLE classification,17,20,21,29 only two reported a significant correlation.21,29 Such differences are probably due to the small sample sizes of the published studies and the low incidence of mortality in the PICU.
The increased morbidity associated to AKI, assessed as a longer stay in the PICU, longer admission to hospital, and a longer duration of mechanical ventilation, has been confirmed by studies in both adults9,10,12,13 and children.6,20–22,27,29,30 Studies in adults moreover have reported increasing risk with increasing AKI severity based on the RIFLE criteria. Our own data coincide with these observations. However, this association had not been previously reported in the series in children.
On the other hand, we have separately analyzed the children with prerenal AKI and those with established AKI, with the aim of examining the effect of temporary dysfunction versus established AKI upon patient morbidity. As expected, we found that children with established AKI suffered greater morbidity than those with prerenal AKI. Furthermore, we observed an independent relationship between established AKI and the studied morbidity parameters. The absence of this association in the children with prerenal AKI may have been influenced by the fact that the studied morbidity criteria were met in only a few of these patients (5 were subjected to mechanical ventilation during over 7 days, 10 had a PICU stay of over 12 days, and 10 were admitted to hospital for more than 28 days).
Given the important morbidity–mortality associated to the development of AKI in critical children, the early adoption of measures designed to reduce the incidence and/or severity of AKI could help improve the outcome of these patients.
Our study has a number of limitations: (1) its retrospective, single-center design; (2) the small number of patients included; (3) the fact that the basal eGFR of part of the patients had to be extrapolated from reference creatinine values adjusted for age; and (4) the fact that the oliguria criterion could not be adequately assessed in all the patients, since not all the children were catheterized.
ConclusionsThe development of AKI in children admitted to the PICU is associated to increased morbidity–mortality. The categorization of AKI based on the pRIFLE criteria, and the use of well established definitions and criteria, allow adequate identification of the associated morbidity–mortality risk, and can contribute to the early detection of those patients at risk of suffering AKI, with the adoption of measures designed to reduce the incidence and severity of the syndrome.
Conflicts of interestThe authors declare that they have no conflicts of interest.
The authors express their gratitude to all the staff members of the Pediatric Intensive Care Unit of Gregorio Marañón University General Hospital.
Please cite this article as: Gómez Polo JC, Alcaraz Romero AJ, Gil-Ruíz Gil-Esparza MA, López-Herce Cid J, García San Prudencio M, Fernández Lafever SN, et al. Morbimortalidad asociada al daño renal agudo en pacientes ingresados en unidades de cuidados intensivos pediátricos. Med Intensiva. 2014;38:430–437.