To analyze mortality and resource consumption in patients with long stays in pediatric intensive care units (PICUs).
DesignA retrospective, descriptive case series study.
ScopeMedical-surgical PICU in a third level hospital.
PatientsData were collected from patients with a stay of 28 days or more in PICU between 2006 and 2010. Of the 2118 patients assisted in this period, 83 (3.9%) required prolonged stay.
Study variablesMorbidity–mortality and resource consumption among patients with prolonged stay in the PICU.
ResultsMortality was higher in patients with a long stay (22.9%) than in the rest of the patients (2%) (p<0.001). In 52.6% of these patients, death occurred after withdrawal of treatment or after not starting resuscitation measures. Patients with prolonged stay showed a high incidence of nosocomial infection (96.3%) and an important consumption of healthcare resources (97.6% required conventional mechanical ventilation, 90.2% required transfusion of blood products, 86.7% required intravenous vasoactive drugs and 22.9% required extracorporeal membrane oxygenation [ECMO]).
ConclusionsCritical children with prolonged stay in the PICU show important morbidity and mortality, and an important consumption of healthcare resources. The adoption of specific measures permitting early identification of patients at risk of prolonged stay is needed in order to adapt therapeutic measures and available resources, and to improve treatment efficiency.
Analizar la mortalidad y el consumo de recursos de los niños con ingreso prolongado en unidades de cuidados intensivos pediátricos (UCIP).
DiseñoEstudio descriptivo retrospectivo de una serie de casos.
ÁmbitoUCIP médico-quirúrgica de un hospital de tercer nivel.
PacientesSe recogieron los datos de los pacientes ingresados durante 28 o más días en la UCIP entre 2006 y 2010. De los 2.118 pacientes ingresados entre 2006 y 2010, 83 (3,9%) requirieron ingreso prolongado.
Variables de interésSe analizaron la morbimortalidad y el consumo de recursos por los pacientes con ingreso prolongado.
ResultadosLa mortalidad de los pacientes con ingreso prolongado fue mayor (22,9%) que la del resto de los pacientes (2%) (p<0,001). En un 52,6% de estos pacientes el fallecimiento se produjo tras la limitación del esfuerzo terapéutico o por no iniciar medidas de reanimación. Los pacientes con ingreso prolongado presentaron una elevada incidencia de infección nosocomial (96,3%) y un elevado consumo de los recursos asistenciales (el 97,6% precisó ventilación mecánica; el 90,2%, transfusión de hemoderivados; el 86,7% fármacos vasoactivos intravenosos, y el 22,9%, oxigenación por membrana extracorpórea (ECMO)).
ConclusionesLos niños en estado crítico con ingreso prolongado en la UCIP tienen una elevada morbimortalidad y requieren un elevado consumo de recursos asistenciales. Son necesarias medidas específicas que permitan identificar precozmente a los pacientes susceptibles de presentar ingreso prolongado para adecuar las medidas terapéuticas y los recursos disponibles y mejorar la eficiencia del tratamiento.
In the last few decades technological advances and the development of new treatments have led to a decrease in mortality in pediatric intensive care units (PICUs). However, these improvements in turn have led to the appearance of a new patient profile in these units, namely subjects who remain admitted to the PICU for very prolonged periods of time.
Such scientific–technological progress has given rise not only to a greater presence of patients in life-threatening situations for prolonged periods of time but also to an increasing number of patients in intensive care who are dependent upon a given type of technology or medical care which for different reasons cannot be provided outside these units.1
Patients with prolonged admission constitute a minority group, though as a result of their prolonged stay and their illnesses, they often consume an important amount of healthcare resources, with increased morbidity and mortality.2–4
The early identification of these patients could allow improved channeling of sociosanitary resources, thereby ensuring improved care and better utilization of the available resources.5–9
The present study analyzes the characteristics and evolution of the patients admitted for over 28 days to a PICU, and examines the mortality and the healthcare resource consumption generated by these patients.
Patients and methodsA retrospective descriptive study was made, based on a review of the clinical histories of all patients admitted to the PICU for 28 days or more during the period between January 2006 and March 2010.
Our PICU belongs to a third-level hospital with a recruitment population of approximately 700,000 in the Community of Madrid (Spain), and which moreover constitutes a national reference center in heart surgery. The PICU is an 11-bed medical-surgical unit with a heart surgery program and extracorporeal membrane oxygenation (ECMO).
The following data were collected on all patients: age, sex, diagnosis, presence of congenital anomalies and congenital heart disease, date and reason for admission, origin, existence of previous cardiorespiratory arrest, and type of surgery performed in the case of postsurgery patients. Severity scores were not recorded, since these are not systematically registered in our PICU.
As variables related to treatment, we registered the type of assisted ventilation (invasive mechanical ventilation, high-frequency ventilation, noninvasive ventilation, high-flow oxygen therapy) and its duration, the continuous perfusion of vasoactive drugs and its duration, extrarenal filtration techniques (specifying whether peritoneal dialysis or continuous venovenous extrarenal filtration was used) and their duration, treatment and duration of ECMO and/or ventricular assist procedures, other techniques (central venous catheterization, arterial catheterization, tracheostomy, gastrostomy and bladder catheterization), and the incidence and location of nosocomial infections. We likewise documented mortality, the causes of death, whether the patients were receiving vasoactive drugs, mechanical ventilation or ECMO at the time of death, and whether there had been limitation of therapeutic effort or a decision not to resuscitate. In the surviving patients we registered the destination at discharge from the PICU.
The data were analyzed using the SPSS version 15.0 statistical package for MS Windows. The χ2 test was applied for the analysis of qualitative variables related to mortality, while the Student t-test was used to analyze the differences in the means or duration of the different treatments between deceased patients and survivors.
ResultsDuring the study period we recorded a total of 2118 admissions to the PICU; of these, 83 (3.9%) involved a stay of 28 days or more. The prolonged stays accounted for 36.1% of the global stay in the PICU. The mean duration of stay in the patients with prolonged admission was 55.6±30.1 days (median 45 days, range 28–179 days)—the mean stay in the PICU for the total series being 6 days (range 0–179 days).
A total of 65.1% of the patients with prolonged admission were males, with a median age of 5 months (range 0–217 months); 65.1% were under 12 months of age. In turn, 81.9% presented congenital anomalies, and 73.5% of the total patients with prolonged admission were diagnosed with congenital heart disease.
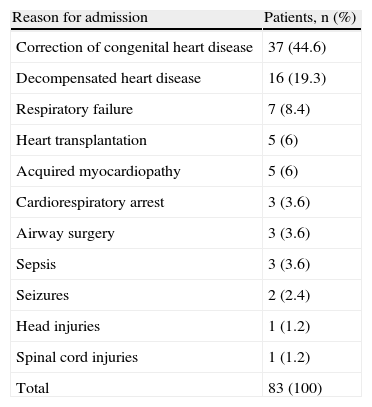
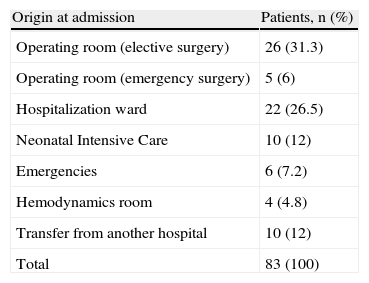
Table 1 shows the diagnoses of the patients with prolonged admission. A total of 75.9% of the patients with prolonged admission suffered heart disease (the reason for admission being its surgical correction, heart transplantation or heart failure). In turn, 37.3% of the admissions were from the operating room (heart surgery in 92.7%) (Table 2). A percentage of the patients admitted after the correction of congenital heart disease were admitted not from the operating room but from other areas (neonatal ICU, hospitalization ward or hemodynamics room). The most frequent heart diseases in the studied group of patients were left ventricle hypoplasia (14 patients), Shone syndrome (10 patients), major vessel transpositioning (8 patients) and lung atresia (7 patients). Other pathologies were less common.
Diagnoses of the patients with prolonged admission to the PICU.
| Reason for admission | Patients, n (%) |
| Correction of congenital heart disease | 37 (44.6) |
| Decompensated heart disease | 16 (19.3) |
| Respiratory failure | 7 (8.4) |
| Heart transplantation | 5 (6) |
| Acquired myocardiopathy | 5 (6) |
| Cardiorespiratory arrest | 3 (3.6) |
| Airway surgery | 3 (3.6) |
| Sepsis | 3 (3.6) |
| Seizures | 2 (2.4) |
| Head injuries | 1 (1.2) |
| Spinal cord injuries | 1 (1.2) |
| Total | 83 (100) |
Origin at admission of the patients with prolonged admission to the PICU.
| Origin at admission | Patients, n (%) |
| Operating room (elective surgery) | 26 (31.3) |
| Operating room (emergency surgery) | 5 (6) |
| Hospitalization ward | 22 (26.5) |
| Neonatal Intensive Care | 10 (12) |
| Emergencies | 6 (7.2) |
| Hemodynamics room | 4 (4.8) |
| Transfer from another hospital | 10 (12) |
| Total | 83 (100) |
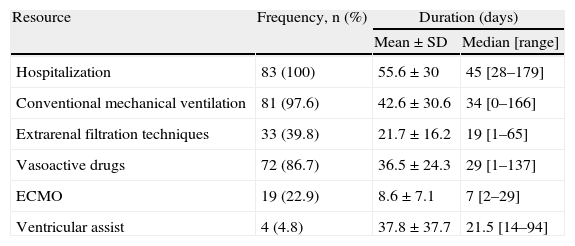
Table 3 summarizes the healthcare resources used among the children with prolonged admission to the PICU. A full 97.6% of the patients required invasive mechanical ventilation, 12% required high-frequency ventilation, and 65% required noninvasive ventilation. In turn, 33 patients (39.8%) required extrarenal filtration techniques: in all these cases venovenous hemodiafiltration was performed, with added peritoneal dialysis in 8 patients (9.6%).
Resources used by the patients with prolonged admission to the PICU.
| Resource | Frequency, n (%) | Duration (days) | |
| Mean±SD | Median [range] | ||
| Hospitalization | 83 (100) | 55.6±30 | 45 [28–179] |
| Conventional mechanical ventilation | 81 (97.6) | 42.6±30.6 | 34 [0–166] |
| Extrarenal filtration techniques | 33 (39.8) | 21.7±16.2 | 19 [1–65] |
| Vasoactive drugs | 72 (86.7) | 36.5±24.3 | 29 [1–137] |
| ECMO | 19 (22.9) | 8.6±7.1 | 7 [2–29] |
| Ventricular assist | 4 (4.8) | 37.8±37.7 | 21.5 [14–94] |
SD: standard deviation.
A total of 86.8% of the patients required inotropic drugs in continuous perfusion (adrenalin in 75.9%), 22.9% were subjected to ECMO, and 4.8% required mechanical ventricular assistance. A total of 24.1% of the patients underwent heart transplantation (15 of them after admission to the PICU).
Bladder catheterization was carried out in 94.9% of the cases, with central venous accesses and arterial catheters in 92.8% and 92.6%, respectively. In turn, 90.2% of the patients required blood product transfusions during admission.
Three patients (3.6%) presented a tracheostomy and four a (4.8%) gastrostomy at the time of admission to the PICU. During their stay, another 13 patients (15.7%) underwent tracheostomy and 9 (10.8%) gastrostomy.
MorbidityInfection was suspected in 32.1% of the patients at the time of admission to the PICU; the percentage corresponding to infections of nosocomial origin could not be established. A total of 96.3% of the patients suffered at least one nosocomial infection during admission—the most frequent condition being pneumonia (72%), followed by urinary infections (34.6%) and catheter-related infections (28.4%).
MortalityA total of 19 of the 83 patients with prolonged admission died. Mortality among the children with prolonged admission was significantly greater (22.9%) than in the rest of the patients (2%) (p<0.001). The most frequent causes of death were withdrawal or limitation of therapeutic effort (42.1%) and the non-adoption of resuscitation measures (10.5%). A total of 8.4% of the patients with prolonged admission had suffered cardiorespiratory arrest (CRA) before admission to the PICU, and 35.4% suffered CRA during their stay.
At the time of death, all the patients were subjected to mechanical ventilation (conventional mechanical ventilation in 89.5%, noninvasive ventilation in 5.3%, and high-frequency ventilation in 5.3%,); 89.5% were receiving vasoactive drugs in continuous perfusion; and 26.7% were subjected to ECMO.
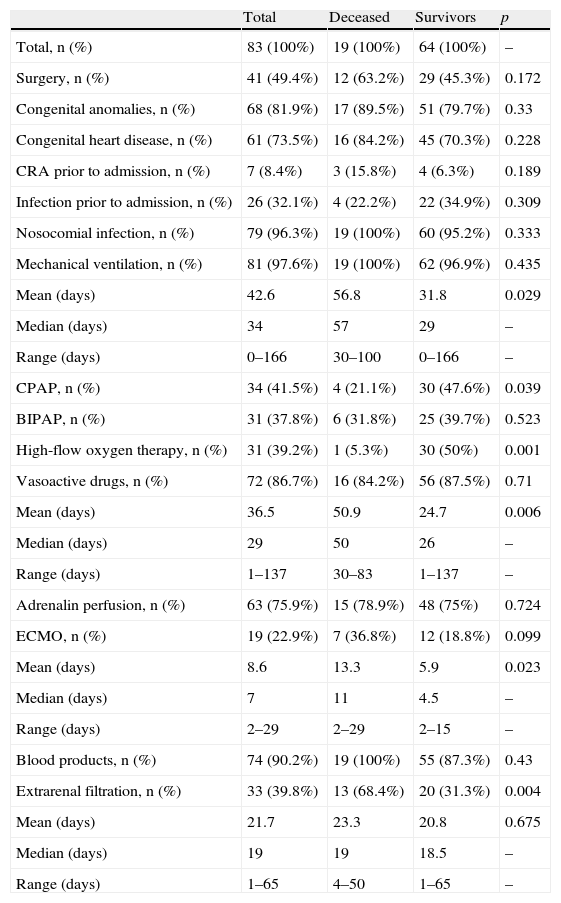
There was no difference in mortality between patients under one year of age (23.3%) and the older children (22.6%). Table 4 depicts the relation of other variables to mortality. Although congenital heart disease, admission after surgery, ECMO, continuous extrarenal filtration techniques (CEFT), and blood product transfusions were more frequent in the patients who died, the differences only reached statistical significance in the case of CEFT. The patients who died presented a comparatively longer duration of mechanical ventilation, inotropic drug treatment and ECMO (Table 4).
Comparison of deceased patients and survivors.
| Total | Deceased | Survivors | p | |
| Total, n (%) | 83 (100%) | 19 (100%) | 64 (100%) | – |
| Surgery, n (%) | 41 (49.4%) | 12 (63.2%) | 29 (45.3%) | 0.172 |
| Congenital anomalies, n (%) | 68 (81.9%) | 17 (89.5%) | 51 (79.7%) | 0.33 |
| Congenital heart disease, n (%) | 61 (73.5%) | 16 (84.2%) | 45 (70.3%) | 0.228 |
| CRA prior to admission, n (%) | 7 (8.4%) | 3 (15.8%) | 4 (6.3%) | 0.189 |
| Infection prior to admission, n (%) | 26 (32.1%) | 4 (22.2%) | 22 (34.9%) | 0.309 |
| Nosocomial infection, n (%) | 79 (96.3%) | 19 (100%) | 60 (95.2%) | 0.333 |
| Mechanical ventilation, n (%) | 81 (97.6%) | 19 (100%) | 62 (96.9%) | 0.435 |
| Mean (days) | 42.6 | 56.8 | 31.8 | 0.029 |
| Median (days) | 34 | 57 | 29 | – |
| Range (days) | 0–166 | 30–100 | 0–166 | – |
| CPAP, n (%) | 34 (41.5%) | 4 (21.1%) | 30 (47.6%) | 0.039 |
| BIPAP, n (%) | 31 (37.8%) | 6 (31.8%) | 25 (39.7%) | 0.523 |
| High-flow oxygen therapy, n (%) | 31 (39.2%) | 1 (5.3%) | 30 (50%) | 0.001 |
| Vasoactive drugs, n (%) | 72 (86.7%) | 16 (84.2%) | 56 (87.5%) | 0.71 |
| Mean (days) | 36.5 | 50.9 | 24.7 | 0.006 |
| Median (days) | 29 | 50 | 26 | – |
| Range (days) | 1–137 | 30–83 | 1–137 | – |
| Adrenalin perfusion, n (%) | 63 (75.9%) | 15 (78.9%) | 48 (75%) | 0.724 |
| ECMO, n (%) | 19 (22.9%) | 7 (36.8%) | 12 (18.8%) | 0.099 |
| Mean (days) | 8.6 | 13.3 | 5.9 | 0.023 |
| Median (days) | 7 | 11 | 4.5 | – |
| Range (days) | 2–29 | 2–29 | 2–15 | – |
| Blood products, n (%) | 74 (90.2%) | 19 (100%) | 55 (87.3%) | 0.43 |
| Extrarenal filtration, n (%) | 33 (39.8%) | 13 (68.4%) | 20 (31.3%) | 0.004 |
| Mean (days) | 21.7 | 23.3 | 20.8 | 0.675 |
| Median (days) | 19 | 19 | 18.5 | – |
| Range (days) | 1–65 | 4–50 | 1–65 | – |
BIPAP: noninvasive bi-level positive airway pressure ventilation; CPAP: continuous positive airway pressure; ECMO: extracorporeal membrane oxygenation; CRA: cardiorespiratory arrest.
The percentages in each column refer to the group of patients described in the column, not to the total.
Discharge of the survivors was to the pediatric ward (89%) or to other intensive care units (4.6%), while one patient (1.5%) was directly discharged home. Three patients (4.6%) were still in the PICU at the end of the study.
DiscussionThe results of our study coincide with those published in other countries, and reveal that patients with prolonged admission to the PICU, while few in number, generate great concern and account for an important percentage of hospital stay.
The epidemiological characteristics of our patients are similar to those described by other authors, with a predominance of males and an important percentage of cases of congenital malformations—particularly heart diseases.1–3,10 In effect, our series shows an important presence of patients with heart disease—this possibly being conditioned by the fact that our PICU is a reference center for disorders of this kind. This also explains why most admissions were from the operating room, other hospitalization areas, or from other centers.
Healthcare resourcesWe have observed important healthcare resource utilization among the patients with prolonged admission, in coincidence with the findings of earlier studies.1,5,11,12
Tracheostomy and gastrostomy can improve management, reduce the complications and improve the quality of life of patients with prolonged admission.13–16 Although early tracheotomy is advocated in adults,17,18 in children the best timing for this technique has not been established. The mean intubation time prior to elective tracheostomy in children subjected to prolonged mechanical ventilation varies from 31 to 51 days, depending on the data source.14,15 In a survey of 63 pediatric intensivists in Canada regarding the use of programmed tracheostomy in children subjected to mechanical ventilation, 51% of the interviewed physicians considered programmed tracheostomy to be underused in children.14 In our study, the procedure was only carried out in 15.8% of the patients.
Nosocomial infectionsWe recorded a high incidence of nosocomial infections,19–21 particularly respiratory infections probably related to the important use of invasive mechanical ventilation, in coincidence with the findings of earlier studies.22.23 Likewise, the prolonged use of central vascular accesses and bladder catheterization favors infection in these locations. Specific measures are therefore needed to reduce the duration of invasive techniques, and to prevent and quickly diagnose and treat nosocomial infectious processes in these patients.5,6,10,11,24–27
Discharge from the PICUMost of our patients were discharged to other hospitalization areas. Patients with prolonged admission to the PICU often remain dependent upon technological systems—fundamentally mechanical ventilation—and so require specific care measures not available in the hospitalization wards.28 This fact often delays discharge from the PICU, despite the achievement of sufficient patient stability.
The creation of intermediate care units or units for technology-dependent patients, with sufficient personnel and specific material resources to safely treat subjects in clinical conditions that are unlikely to change (apart from the development of complications), could allow for more efficient healthcare resource utilization.29,30
Home mechanical ventilation facilitates the out-hospital care of some patients, increasing their quality of life and that of their relatives. However, this option requires the existence of care teams to conduct regular controls and to train the caregivers, and the family in turn must receive sufficient sociosanitary support. The scarcity of these aids often represents an obstacle for discharging patients from the PICU, contributing to further their chronification and institutionalization.28,31,32
MortalityMortality among patients with prolonged admission is much higher than in the rest of the patients admitted to the PICU. In effect, the mortality rate in our series was 10 times greater—in coincidence with the findings of other authors in pediatric patients.2,3,33 It is important to mention that our PICU does not often admit patients for short-duration techniques or procedures—the low associated mortality of which would have contributed to lower our overall mortality figures.
The early identification of patients with a high mortality risk could allow more efficient use of the available resources, attempting to avoid the use of futile invasive procedures.7 Some factors, such as heart diseases, or the need for extrarenal filtration techniques or ECMO, are associated with increased mortality, though in our study most of them showed no statistically significant differences. Nevertheless, it must be taken into account that most of these factors are only indicators or markers of patient severity.
In our study, and in the same way as in other series,3,34,35 the cause of death in almost one-half of the cases was the withdrawal or limitation of therapeutic effort. Despite this fact, in most cases mechanical ventilation or vasoactive drug treatment was maintained up until death. This may be due to the way in which the limitation of therapeutic effort is carried out in our PICU, though it could also imply the excessive prolongation of techniques that may be regarded as futile. It therefore seems necessary to optimize the approach to such patients when death draws near—addressing and planning the measures to be taken, with a view to avoiding inadequate treatment prolongation.3–5,8,34
Considering the retrospective design of our study, it is important to point out that its main limitation is the absence of comparisons between the group of patients with prolonged admission and those without prolonged admission—a situation that precluded a multivariate statistical analysis of the risk factors for prolonged admission.
On the other hand, our PICU has a series of specific characteristics due to the high percentage of patients admitted with congenital heart disease. Other studies involving PICUs with more general patients are therefore needed to confirm the results obtained.
In conclusion, although children subjected to prolonged admission represent a small percentage of the patients seen in the PICU, they suffer important morbidity–mortality, account for much of the occupation of the unit, and involve important healthcare resource utilization. Early identification is required of those patients with a high risk of requiring prolonged admission, in order to establish specific management strategies designed to allow more efficient care and use of the available resources. The creation of intermediate care units for the management of these patients may help reduce resource consumption and increase the quality of the provided healthcare.
Please cite this article as: González-Cortés R, et al. Ingreso prolongado en la unidad de cuidados intensivos pediátricos: mortalidad y consumo de recursos asistenciales. Med Intensiva. 2011;35:417–23.