Provision of aid (POA) became effective in June 2021 after the Organic Law 3/2021 (LORE) of 24 March1 on the Regulation of Euthanasia was passed in Spain. This law regulates not only euthanasia, but also physician-assisted suicide in certain situations defined by this law as euthanasia context: incurable disease and/or unbearable suffering.
This law introduces the new individual right to decide the moment of death by requesting POA. Also, this law tries to juggle the right to live, physical and moral integrity, the right of human dignity, individual freedom, and the patient's autonomy.
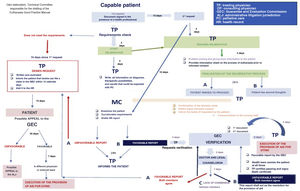
Two different options are included in this law: euthanasia or physician-assisted suicide. The definitions of euthanasia and physician-assisted suicide are detailed in the Figure 1. From now on it will be the patient and the patient alone who shall decide what kind of care he/she wants, the treating physician, where he/she will receive such care, and ultimately when. The entire process is backed by a protocol implemented by 3 doctors and 1 legal counselor who study the case to elucidate possible conflicts of interest, and make sure that the law is observed at all times6 (Fig. 1).
The passing of the LORE1 and its implementation has been received differently by health professionals and society in general. For some this law was long needed. For others, it questions personal and moral values and is, therefore, perceived as a threat. Changes are always difficult to digest and need social debate in the professional setting too. The existing cultural, ideologic or religious differences give different meaning to life and death for each and every one of us. Therefore, life and death are often seen from the standpoint of believes and individual values, and not from a neutral stance.
A study claims that 18% of intensivists have already received some kind of request for POA at one time or another at the ICU setting7. Obviously, such POA triggers reflection and doubt: is euthanasia a medical act/duty? Can doctors refuse to accept the will of the patient on moral grounds? Which possible end-of-life scenarios can occur? Is euthanasia an alternative to palliative care?
And ultimately…is it even ethical to provide POA?
Our duty as doctors is not only to cure, but also to help those who can’t be cured or who are suffering. Also, their dignity and autonomy should be observed from the point of view of good medical practice by providing a so-called good death without suffering or pain2. If medical aid to contribute to the process of dying when no other aid (whether clinical, social or spiritual) can alleviate constant and intolerable pain for a person, this would not only be considered morally acceptable, but as a true act of compassion. In other words, it would be the ultimate professional and personal sacrifice for the suffering patient, which then would make euthanasia totally understandable as a true “medical act”3.
A paragraph has been deleted here…
Conflict appears when the right of the patient confronts the right of the health professional to oppose this law4. Conscientious objection is contemplated and regulated by the law and should be observed too. However, this law does not contemplate the possibility of institutional conscientious objection in no way or form.
In some situations where POA has been requested, different end-of-life scenarios can “coexist” (Table 1). Therefore, even when POA has been requested, other life-related situations like palliative care, therapeutic adequation or the indication of palliative of terminal sedation should not be avoided or postponed5,9.
End-of-life scenarios.10
| Adequation or limitation of life-sustaining treatment | Withdrawing, avoiding increasing or starting treatment when life prognosis is limited, or treatment is considered futile by the health team. This decision is often made by the latter. |
| Treatment rejection or consent denial | In this case it is the patient who refuses to receive treatment (although indicated), thus enacting his right to decide freely after having received all the information required on the clinical options available.This rejection can involve the possibility that the patient jeopardizes his health and is anticipated by Law 41/2002 of 14 November regulating Patient Autonomy and Rights and Obligations regarding Clinical Information and Documentation of information and clinical documentation10. |
| Palliative sedation or sedation in agony | It is the deliberate reduction of the patient's conscience once information has been provided (whether the patient or his/her representative if unable to make decisions) through the administration of the drugs indicated and the doses indicated to avoid the unbearable suffering caused by one or more refractory symptoms.When the patient is in his/her final days or hours of life we call this sedation in agony. |
| Provision of aid (POA) for dying | Provision of substances that will eventually lead to the death of the person who is under unbearable suffering in a euthanasia setting. It can occur in 2 different ways:“Euthanasia” is intentionally causing the death of a person who is suffering an unbearable pain that causes him/her major disability or limited life expectancy, and intolerable suffering after repeated express petition by him/her all within a medical context.“Physician-assisted suicide”. It refers to the medical attention provided to facilitate suicide upon a patient's express petition in the situation described above for euthanasia. As a result to this, the necessary drugs will be provided by the doctor and administered by the patient himself/herself. |
When our patients are not competent anymore decisions need to be made surrogately at the ICU setting. In these cases, our obligation is to enable people to be able to make decisions while taking into consideration that the more complex the decision the more competence will be required. Regarding POA, the only possible scenarios would be 1) a patient who has already signed his/her Last Will and Testament (LWT) document and is incapacitated to make own decisions, and 2) a patient who has been admitted to the ICU, and requests POA. If the requirements set forth by the law are met, our duty shall be to respect the patient's last will and proceed with the POA request.
The intensivist shall do his share in cases of POA with a will to donate organs. It can happen that intensivist involved in the process of POA donation, all of a sudden, becomes the organ donation coordinator too. Also, in these cases, ICU admission prior to donation with involvement from other intensivists can be an option. Intensivists shall not take a stance regarding POA and only act in their capacity of organ transplant coordinators. Here, despite his involvement in the final process, the intensivist-coordinator can be reluctant to comply or be morally impaired to do so. This underscoores that the moral distress of the health professionals involved also needs to be taken seriously.
Ethics also calls upon us regarding euthanasia the same way ethical conflicts did during the pandemic8. Therefore, the implementation of artificial intelligence, also with euthanasia, with dilemmas of corporate and organization ethics involved, and our own response as intensivists with a high level of skills and expertise, both human and technical, should also empower us in the field of bioethics. Therefore, we should be trained in end-of-life scenarios to meet the new ethical needs at hand, and those of people themselves in the most rigorous and excellent way by leaving professional prejudices, suspicions, conflicts of interest, and defensive medicine behind for the sake of those we treat and the society we are part of as health professionals.
Regarding euthanasia, our duty should also be acting according to ethics and the kind of professionalism that society and patients alike expect from us.
Conflicts of interestNone whatsoever.