In 1348, a pandemic known as Black Death devastated humanity and changed social, economic and geopolitical world order, as is the current case with SARS-CoV-2 coronavirus. The doctor of the Nasrid Kingdom of Granada, Ibn-Jatima from Almeria, wrote “Treatise on the Plague”, in which it may be found epidemiological and clinical similarities between both plagues. In the context of Greco-Arab medicine, he discovered respiratory and contact contagion of Pestis and attributed its physiopathology to a lack of pulmonary cooling of the innate heat, generated in the heart and carried by the blood humor. The process described was equivalent to the oxygen transport system. Furthermore, it was supposed to generate toxic residues, such as free radicals, leading to an irreversible multiple organ failure (MOF), considered a mortality factor as in Covid-19. Due to its similitude, it would be the first antecedent of the MOF physiopathological concept, a finding that enriches the scientific and historical heritage of our clinical specialty.
En el año 1348 una pandemia de la llamada Peste Negra asoló la humanidad y cambió el orden social, económico y geopolítico del mundo, tal como sucede actualmente con la causada por el coronavirus SARS-CoV-2. El médico del reino nazarí de Granada, Ibn-Jatima de Almería, escribió un “Tratado sobre la peste” en el cual se encuentran semejanzas epidemiológicas y clínicas entre ambas plagas. Así, dentro del contexto de la medicina greco-árabe, descubrió el contagio respiratorio y por contacto de la peste y atribuyó su fisiopatología a una insuficiente refrigeración pulmonar del calor innato generado en el corazón y vehiculizado por el humor sanguíneo, equivalente al sistema de trasporte de oxígeno, lo cual generaba residuos tóxicos, como los radicales libres, que abocaba a un fallo de múltiples órganos (FMO) irreversible, factor de mortalidad como en la Covid-19. Por su similitud, sería el primer antecedente conocido del concepto fisiopatológico de FMO, hallazgo que enriquece nuestro patrimonio científico-histórico de la especialidad.
Since its appearance in 2020, the current SARS-CoV-2 coronavirus pandemic has generated worldwide alarm due to its broad range of repercussions — medical, scientific, demographic, social, economic, political and cultural. In this still opening stage of the XXI century, economists, sociologists, physicians, investigators, politicians, philosophers, historians and intellectuals, etc., unanimously agree1–4 that this is the pandemic that has changed the world.5 The same was affirmed by the great historian Ibn Jaldun (1332–1402) six centuries ago regarding the plague epidemic that struck Humanity in 13486:
“[…] The terrible plague that was unleashed upon Mankind, in both the East and the West, laying waste countries and depriving us of part of our generation. Its wave destroyed many of the achievements of civilization. It surprised and weakened dynasties that were already in decline, shortening their reign and moving them closer to their end and final destruction. The demographic loss lowered the level of civilization. Towns and homes became vacant, cities were depopulated, and dynasties and tribes were weakened. The face of the inhabited world changed”.
This observation by Ibn Jaldun is not surprising, since the bubonic plague caused by the bacterium Yersinia pestis was the worst human demographic catastrophe ever known, and one of the greatest cataclysms in History. It was also known as the Black Death, because of the multiple necrotic ulcers and bleeding of the skin suffered by the affected individuals, giving the impression of the entire body covered with dark or black plaques. This terrible disease invaded Europe, Asia and Africa, wreaking havoc on all three continents. The pandemic in Europe lasted from 1347 to 1350, and in those three years its caused the death of approximately 25 million people – approximately one-third of the total population – and of about 40 million on the other two continents.7–9
In addition to this coincidence in the general analysis of the global situation created by the two pandemics, other similarities can be found in their epidemiology, and particularly in the physiopathological conception of the disease. The present article seeks to show that Ibn Jatima may be regarded as a pioneer in the notion or conception of multiorgan failure (MOF) – a syndrome that currently constitutes a leading presence among the disease conditions typically seen in intensive care medicine – with a view to contributing to our scientific and historical perspective of the specialty and acknowledging the legacy in Medicine left by Al-Andalus.
COVID-19 and the plague: common points of both pandemicsWith regard to the epidemiological aspects, many of the measures that are currently considered to be essential for controlling the spread of SARS-CoV-2, such as isolation of the infected individuals or lock-down of the population, had already been discovered and advocated in Spain many centuries ago – specifically in the times of Al-Andalus (711–1492), during the mentioned plague of the XIV century. This was done by three physicians of the Nasrid Kingdom of Granada (1238–1492), the last Muslim stronghold on the Iberian Peninsula: Ibn al Jatib, Ibn Saquri, and mainly our personage, Ibn Jatima.
Ibn Jatima came into contact with the pandemic in Almería, his home city. There he treated many of its inhabitants, and in 1349 he wrote a text entitled: Tahsil garad al-qasid fi-tafsil al-moral al-wafid (“Al-Tahsil”) or Achievement of the proposed objective in clarifying the disease of the plague (more briefly: A treatise on the plague), based on the study of the ancient authors and particularly on his own practice and observations in the field. In this work, which has recently been translated into Spanish by Prof. Arvide Cambra,10 and whose contents and structure are shown in Table 1, Ibn Jatima was ahead of his time in many of the scientific advances and discoveries that later would take place in the XIX and XX centuries in epidemiological and microbiological theory — notoriously in those aspects referred to transmission of the disease.
Structure and contents of A treatise on the plague, by Ibn Jatima.
| Structure | Content |
|---|---|
| Subject I | About the nature of the plague |
| Subject II | About the general and specific causes of the plague |
| Subject III | About the geographic determinants of the plague |
| Subject IV | About contagion of the plague |
| Subject V | About how to protect against and prevent the plague |
| Subject VI | About treatment of the plague |
| Subject VII | About the specifications of Islamic law regarding the plague and other epidemics |
| Subject VIII | About the meaning of the hadith “Prohibition to go to or leave plague-affected territory” |
| Subject IX | About the meaning of the saying from the one sent from God: “There is no contagion or ill omen” |
| Subject X | About joining of the two hadiths |
In effect, Ibn Jatima speaks of “vapors or mists infected with minute organisms” that invade the body of the individual, causing illness, and which are transmitted from one individual to another through the air we breathe and through contact with diseased persons11:
“And in the same way that harm comes from the breath of the patients when they breathe, it also comes from the vapors that arise from their bodies, even if not under their influence or susceptible to them, and from the use of their clothing and beds where they spend the time of the illness, if they wear long gowns or in the presence of persistent inhalation. Science and experience are a witness to all this. […] The purpose of forbidding (contact) is to instruct in the care of those who are healthy in order to prevent them from becoming ill, through the power of Almighty god, when the patients are brought before them, as is commonly done”.
Ibn Jatima made this lucid statement at a time when the rest of his Muslim colleagues and those in the Christian kingdoms of Spain, Italy or France regarded the plague as a punishment from God, or the consequence of a fatal astrological alignment or the intentional poisoning of food.12 In addition, Ibn Jatima conducted such a precise epidemiological investigation that he was able to locate the exact place in the city where the epidemic started – the poorest area in Almería – and identified the first affected family (“patient zero”). Furthermore, and in the same case as COVID-19, he established the origin of the pandemic in being China13:
“I am convinced, from what certain merchants arriving in Almería explain, that the illness started in the country of Kitai, which in the language of the Persians means China, as I have been informed by some people coming from Samarkand, and who constitute a reliable source”.
The clinical manifestations of SARS-CoV-2 range from asymptomatic infection to severe respiratory failure. In 10%–20% of all seriously ill patients, respiratory failure progresses towards acute respiratory distress syndrome (ARDS) between 8–14 days after onset of the disease,14 and this in turn is associated to a high mortality rate in the Intensive Care Unit (ICU).15 As the disease progresses, patients may suffer complications that result in MOF,16 which constitutes an independent in-hospital mortality factor.17 It is in this clinical context of MOF of pulmonary origin where we again observed a link between these two pandemics separated by centuries. Although the contributions of Ibn Jatima to epidemiology are recognized, little has been mentioned to date about the originality of his theory on the physiopathology of the plague and the conceptual similarity – within Galen’s humoral medicine – with the initial description of MOF.
Medicine in the times of Ibn JatimaIbn Jatima was born in Almería in 1324 and died in 1369 in that same city. Few bibliographical data are available. He was a reputed writer and scientist, though he only held positions as a secretary and a reciter of the Koran in the mosque of Almería — these being regarded as secondary social positions at that time.18 Ibn Jatima was one of the most important intellectuals of Al-Andalus in the XIV century due to his works in medicine, history and poetry — the latter being an experimental interest anticipating surrealism and Dadaism.19 He was much appreciated by the leading intellectuals of his time, and with whom he had excellent ties, including the erudite from Granada, Ibn al Jatib,20 who was a close friend. Ibn Jatima became known by and frequented the literary gatherings of the Nasrid aristocracy in Granada, where the erudite public admired him for his intelligence and knowledge, and particularly for his personal charm and kindness.
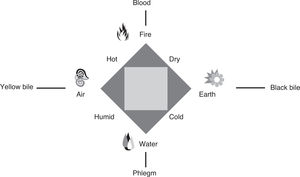
In order to relate the physiopathology of the plague as described by Ibn Jatima to that of MOF, we first must briefly consider the theoretical framework of medieval Arab Medicine in Al-Andalus, constructed upon the Greek legacy of Corpus Hippocraticumand Galen. The doctrine of natural body structure is based on the quaternary division of the Universe and the human body: the world in which humans live, and from which they are nurtured, is composed of four core “elements”, namely air, fire, water and earth, in variable proportions. These elements in turn each have a pair of the four natural “qualities”: heat, cold, humidity and dryness, where they are organized according to a combinatory dynamic of binary oppositions. Thus, earth is cold and dry, water is cold and humid, fire is hot and dry, and air is hot and humid.
The abovementioned four cosmic elements in turn are associated to four secondary elements or “humors”. A humor is understood to be a more or less viscous fluid that remains unchanged in all the natural transformations of human physiology.21 There are four basic humors: blood (haima), phlegm (phlegma), yellow bile (xanthe chole) and black bile (melaina chole), respectively derived from air, water, fire and earth (Fig. 1). The variable mixing of the four humors gives rise to the different organic fluids, in which one humor predominates over the rest.
The humors, as the basis of life, are mobilized by “forces or faculties” that need to be activated by “spirits or powers” for the “organs or members” to function. The heart is the noblest of organs in that it vehiculizes nurturing blood and generates and distributes “innate or natural heat” to the entire body. Accordingly, it is regarded as the motor of all the phenomena essential for life, the essence of animal strength and of spiritual strength. Likewise, this heat or warmth is the primary agent of the substantial transformations (metabolism or “digestion”) that constitute the vital processes of the higher animal species, but which needs to be cooled by the inhaled air and to act with moderation upon the peripheral organs in a regulated manner — since the heat required for nutritional functions, for example, is not the same as that required for sensory functions.
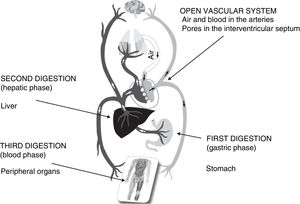
Food, which is the origin of the humors, undergoes transformation — a digestion or “cooking” process comprising three phases22: a “gastric phase” where the waste is composed of excrements; a “hepatic phase” in which waste is represented by urine and the two forms of bile; and a “blood phase” in which the waste consists of perspiration, dense vapor produced by the body, dirt, hair and “similar things”. The cardiovascular system is open, with blood originating in the liver from the food that has undergone first digestion in the stomach. As such, blood does not circulate; it only undergoes centrifugal displacement through the veins and arteries, ending in the bones, muscles and internal organs, where it provides nutrients and the mentioned innate heat. The lungs in turn supply air (“pneuma”) to the left ventricle, which cools the blood that has arrived from the pulmonary veins and fills the right ventricle — since interventricular communication (“pores”) allows the blood (arterial and venous) to mix with the air in the left ventricle (Fig. 2), before being distributed throughout the body.23,24 The arteries consequently contain air and blood, and transport innate heat and vital spirit. The vapors, generated as a sub-product of innate heat, are expelled in the pulmonary vein during systole, and are finally exhaled through the respiratory airway.25
Health is the result of a harmonious and proportionate combination of humors (“crasis”), without excess or deficit, inherent to each individual (i.e., personal “idiosyncrasy”). In turn, disease is the consequence of an inadequate combination (“dyscrasia”) of humors. This notion is the guiding principle of medical practice, since the art of Medicine consists of keeping the humors in balance as an expression of health, either through prior measures intended to preserve this balance, or through treatments designed to restore it when the balance is lost or perturbed. The objective of humoral theory is to neutralize or evacuate the harmful humor in order to restore the normal or balanced profile.
Physiopathology of the plague: the first description of multiorgan failureFrom the point of view of Ibn Jatima, what alterations take place in the body, and why is the plague such a serious and almost always fatal disease? It certainly is a “fever”, but he points out that it is not like others: it is a very particular kind of fever. What is especially interesting here is that Ibn Jatima is aware that he is witnessing a new clinical phenomenon, that he is facing a “strange” fever, he explains, with a special origin and behavior26:
“He knows that these fevers of the plague are not like other fevers, but are in some way different”.
In contrast to other fevers, where “the heat first emerges from the place of outbreak of the fever”, whether a corrupted humor, a tumor, a principal body organ, etc., and then “invades the heart through the arteries” and “subsequently spreads from the heart to the rest of the body”, the fever seen in the plague runs in the opposite physiological direction, and this amazing particularity is precisely what in the words of Ibn Jatima explains the extreme seriousness of the disorder27:
“With regard to the kind of fever this is, I have seen that it is a rare fever that proves harmful for the natural actions and that reaches the heart to then spread from the heart to invade the entire body”.
In modern Medicine, the cardiocirculatory and respiratory apparatuses interact to conform the physiological system whereby oxygen is administered to the cells — this being equivalent in medieval Medicine to the physiological system that supplies innate heat to the body organs. The focal point is the same: innate heat spreads throughout the body and, in the same way as oxygen (O2), constitutes the driving force of the vital functions28:
“The heart is the origin and source of heat. In the case of animals, the heart is like the stove or energy source from which innate heat expands and spreads to all the organs through the arteries that arise from the left ventricle”.
But this heat needs the lungs (a “respirator” in his words) to adjust the temperature, cool down and eliminate the “smoke emanations” associated with its distribution28:
“When the chest expands and air is inhaled, the lungs open and air enters them from the exterior. The air is transported through the trachea and its branches, reaching the venous artery of the heart (the aorta) that arises from the left ventricle. And the air that has been refined in the small respiratory branches balances the heat of the heart, cooling it, mitigating boiling of the heat and preserving the natural temperament of the heart. When the chest contracts, the lungs close and the air that had entered upon expanding emerges again. Then, with this air, all the smoke emanations that had accumulated within emerge as well – smoke vapors caused and stimulated by the heat”.
Since this combined and harmonious system depends on the proper functioning of all the parts of the human body, its breakdown inevitably results in death. From this very physiological initial perspective, Ibn Jatima established his physiopathological conception of MOF in the context of the plague. Latin authors contemporary of Ibn Jatima, especially Jacme d’Agramont, a professor at the Medical School in Lleida, had described that the inhaled corrupt air entered the heart and caused rotting of the blood which then reached other limbs through the arteries — the pathogenic mechanism common to pandemics.7 However, these authors did not consider the plague as a separate and singular entity, and did not develop a different physiopathological model of the disease.
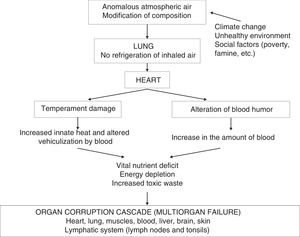
The reasoning was structured upon a causal concatenation of Subjects IV–VI. Firstly, there is a loss of the moderating function of the lungs upon innate heat29:
“However, this function of the lungs and the respiratory apparatus does not balance and regulate the heat of the heart with any kind of air but with natural air that has not been and cannot be corrupted, since the alteration of its nature producing putrefaction and corruption – especially if the alteration takes place within the substance – would not satisfy regulation of the heat from the heart and its cooling, or emergence of the smoke emanations from the heart”.[…] When the alteration of the air produced in this event only damage the temperament of the heart by lightening its heat in first place, and by increasing the amount of its blood in second place – exceeding the innate heat regimen through this increase […]”.
Thus, the first failure is referred to the lungs due to dysfunction in regulating the temperature of the inhaled air. However, since the lung and heart conform an inter-related system, both organs are affected29:
“If the putrefied vapors of the patients that emerge with their breaths upon breathing reach the heart and lungs through inhalation of the breathed air, these [the vapors] adhere to both [the heart and lung] through adjustment between their place of emergence and entrance, and there an effect occurs according to their nature – acting through corruption and putrefaction, that is, corrupting and rotting them”.
Then, as a consequence of this respiratory perturbation, corruption of the temperament of the heart occurs, originating anomalous (“strange”) and excessive innate heat, and also an increase in blood humor. These perturbations adversely affect nutrition of all parts of the body, which receive very altered heat, with fatal consequences30:
“In contrast, with their corruption, the vital flows related to the heart would be corrupted, and the innate heat of the heart would be drawn from its natural temperament or humor to the limit of strange heat. As a result, the humor of the heart would turn bad and the humors of the body would become corrupted, since the strange heat would not adequately perform the functions of innate heat in the body. Likewise, the smoke emanations would dominate and eliminate the vital flows, their strength would be corrupted as well, and the natural human composition would break down”.
Lastly, because of this internal perturbation, “toxic” waste and residues would be generated and swept towards the organs, which have less defensive capacity, causing irreversible damage to them. Thus, we here have a mechanism of injury at a distance mediated by humoral factors generated by the generalized reduction of energy supply and depletion of vital nutrients in multiple organs. Ibn Jatima then explains which are these weakened organs and how they become diseased: the lymph nodes and the tonsils (lymphatic system), lungs and pleura, muscles, liver, brain and skin. He also clearly underscores that two or more of these organs may be affected31:
“If the defensive strength faces an organ that is weak and susceptible to the influence of internal organs, the waste will be expelled towards that weakened organ {here he cites the aforementioned organs}. […] It is possible that it (the waste) becomes displaced towards two or more organs depending on the amount of humor and the suitability of the place in relation to susceptibility and reception”.
Thus, although Ibn Jatima details the three clinical forms of presentation of the plague according to the most affected “member” – “buboes”, “hemoptoic sputum” or “skin ulcer” – he does not attribute the death of the patient to a concrete organ but to a general inflammatory disorder32:
“If that heat had remained with its boil, without being regulated and balanced through cooling by the air on breathing, then the heat would have inflamed and burned the body humors, destroying its humidity and causing death”.
This description is a remote antecedent of the concept of multiorgan dysfunction syndrome (MODS), presented according to the medical physiological postulates in place at the time (Fig. 3).
En 1973, Tilney et al. were the first to describe a clinical syndrome characterized by the progressive and sequential failure of multiple body organs, occurring in the postoperative period of patients subjected to ruptured abdominal aorta repair.33 Posteriorly, further cases were published in association to different disease conditions such as sepsis, polytraumatisms, major burns, the postoperative period of major surgery, etc., in other words, involving critical patients after acute injury.34 The sequence generally comprised circulatory failure, followed soon by respiratory failure and later by liver, renal, gastrointestinal and metabolic failure, mediated by a broad range of humoral factors manifesting through an exaggerated and uncontrolled systemic inflammatory response. At present it is defined as “the presence of functional alterations of two or more interdependent organs in critical patients where homeostasis cannot be maintained without therapeutic measures”.35 With regard to these therapeutic measures, and since the first organ to suffer is the heart – as it is the “recipient” of the natural heat and the nutrient source of all the organs – its care is crucial36:
“When this idea takes hold and is clear to you, then perhaps it will seem very evident that the care of this disease should be related to the issue of the heart, with support of its strength and, if possible, improvement of its damaged temperament”.
If we understand the physiopathological theory of the plague as described by Ibn Jatima, it is easy to comprehend the treatment cornerstones he describes and reasons. The central element is initial failure of the heart, which spreads an anomalous innate heat to the entire body and generates an increased and toxic blood humor that produces harmful waste and corrupts the rest of the body organs, leading to final organ failure in cascade and death. For this reason, we must try to eliminate the morbid humor (blood). But this humor cannot be removed like phlegm or yellow or black bile, forcing its evacuation through a natural orifice or by administering purging, emetic or sneeze-inducing medicines. Emergency bleeding is required — this not being an empirical practice but an indication with a physiopathological basis.
The drawing of blood must be abundant (at least “one pound”), almost to the limit of fainting according to the strength and age of the patient, for we must also ensure “disintoxication” of the humor, freeing it from the harmful waste. However, for phlebotomy to be effective, there are two prior requirements. The first is to previously increase myocardial contractility36:
“All this must be done after the patient has taken something to help the strength of the heart and mitigate the impulsiveness of the blood, such as for example apple syrup mixed with honey-vinegar syrup, or alternatively grape syrup (arrope) or verjus (agraz), or also lemon syrup and wood-sorrel diluted in rose syrup”.
The second requirement is to perform phlebotomy within the correct time window. From the first lines of his treatise, Ibn Jatima explains that if there is any chance of curing the plague, it is only in the early stage of the disease, before it develops fully and invades the entire body (4–7 days). Only early treatment can improve the prognosis37:
“It is advisable to be quick in treating the disease, before it moves from its place; […] We have no more accessible and successful treatment than to let the blood come out through a perforation of the veins, especially at the start of the illness, before the heat spreads through the body, fever takes a hold, and the terrible symptoms appear”.
Ibn Jatima then addresses symptomatic treatment, which he regards as merely palliative.38 Of note is the meticulous and exhaustive attention he pays to the remedies for each of the clinical manifestations, in particular those that are most bothersome or painful, in order to alleviate the suffering of the patient. As an example, in the case of diarrhea, he explains the following39:
“We have explained remedies such as these that have two effects, since the aim is to stop the diarrhea in this illness, as it enhances the disease and the torture and suffering of the patient due to the virulence and malignancy of the wastes and residues. For this reason, from the start we should avoid them in the intestine as far as possible with the medicines and confront the diarrhea, repressing its strength and addressing its virulence until constipation gradually occurs”.
This suggests that Ibn Jatima was an excellent clinician, with profound knowledge of the pharmacological resources at the time, and who practiced on the ethical principle of caring for his patients even if this meant placing his own life at risk. And with the intellectual instruments of his era: “according to what science has contributed, experience has witnessed, and effort and practice have confirmed”.26
The current definition and general conceptual postulates of MODS can be applied to the physiopathological interpretation of Ibn Jatima in the scientific context of his time, because they share the following features: (1) his interpretation comprises a different model of body response to the disease; (2) the approach is systemic; (3) homeostasis is altered; (4) the vital nutrient transport system (innate heat versus O2) is deficient and useless; (5) there are lesions at a distance (humoral mediators) vehiculized through the blood; (6) the irreversible organ damage is secondary to anomalous metabolism (toxic waste versus cytokines, free radicals) as a consequence of the above; (7) death is caused by general – not focal – perturbation; (8) the process is critical (high mortality), because the identified risk is maximum; (9) treatment has specific objectives guided by the physiopathology; and (10) treatment must be started early (the crucial time window) in order to have any chance of curing the patient. Furthermore, Ibn Jatima did not obviate the use of symptomatic treatment to alleviate patient suffering.
This study shows that the physiopathological concept of multiorgan failure – so valuable in contemporary intensive care medicine – had been intuited and anticipated by Ibn Jatima in the XIV century, evidencing a notorious clarity of vision as relevant as his theory about contagion, and underscores the merit of his scientific thinking. This pathogenic model of the plague remains useful today in the context of the SARS-CoV-2 pandemic, despite the 7 centuries that have gone by since then. It moreover illustrates that Medicine in Al-Andalus, even in a period of clear geopolitical decline, retained the capacity to innovate up to the very end.40,41
ConclusionsIbn Jatima described the clinical forms of the bubonic plague as a consequence of corruption of the temperament of the heart, which implies diffusion through the body of excessive and anomalous innate heat not adequately cooled by the lungs, and of an also excessive and pathological blood humor. As a consequence of this, toxic waste and residues are generated that cause a chain of alterations in other organs. This situation could well be considered as MOF with a final fatal outcome — a physiopathological interpretation that predates the current concept of MODS by centuries.
Financial supportThe present study has received no funding of any kind.
Conflicts of interestThe author declares that he has no conflicts of interest.
Thanks are due to Dr. Manuel Rodríguez-Carvajal and to Dr. Enrique Pino-Moya for their review of the original manuscript, and their valuable corrections and suggestions. Thanks are also due to Dr. Manuel Rodríguez-Rodríguez for his contribution to improvements in style, and to José María Rodríguez-Rodríguez for help in designing the figures.
Please cite this article as: Herrera Carranza M. A propósito de pandemias: Ibn Jatima de Almería anticipa el concepto fisiopatológico de fallo multiorgánico en el siglo XIV. Med Intensiva. 2021;45:362–370.