To analyze clinical features associated to mortality in oncological patients with unplanned admission to the Intensive Care Unit (ICU), and to determine whether such risk factors differ between patients with solid tumors and those with hematological malignancies.
DesignAn observational study was carried out.
SettingA total of 123 Intensive Care Units across Spain.
PatientsAll cancer patients with unscheduled admission due to acute illness related to the background oncological disease.
InterventionsNone.
Main variablesDemographic parameters, severity scores and clinical condition were assessed, and mortality was analyzed. Multivariate binary logistic regression analysis was performed.
ResultsA total of 482 patients were included: solid cancer (n=311) and hematological malignancy (n=171). Multivariate regression analysis showed the factors independently associated to ICU mortality to be the APACHE II score (OR 1.102; 95% CI 1.064–1.143), medical admission (OR 3.587; 95% CI 1.327–9.701), lung cancer (OR 2.98; 95% CI 1.48–5.99) and mechanical ventilation after the first 24h of ICU stay (OR 2.27; 95% CI 1.09–4.73), whereas no need for mechanical ventilation was identified as a protective factor (OR 0.15; 95% CI 0.09–0.28). In solid cancer patients, the APACHE II score, medical admission, antibiotics in the previous 48h and lung cancer were identified as independent mortality indicators, while no need for mechanical ventilation was identified as a protective factor. In the multivariate analysis, the APACHE II score and mechanical ventilation after 24h of ICU stay were independently associated to mortality in hematological cancer patients, while no need for mechanical ventilation was identified as a protective factor. Neutropenia was not identified as an independent mortality predictor in either the total cohort or in the two subgroups.
ConclusionsThe risk factors associated to mortality did not differ significantly between patients with solid cancers and those with hematological malignancies. Delayed intubation in patients requiring mechanical ventilation might be associated to ICU mortality.
Determinar las características clínicas asociadas con la mortalidad en pacientes oncológicos ingresados de forma no programada en la UCI. También evaluamos si estos factores de riesgos difieren en los pacientes con neoplasias hematológicas o tumores sólidos.
DiseñoEstudio observacional.
ÁmbitoCiento veintitrés Unidades de Cuidados Intensivos en España.
PacientesTodos los pacientes con cáncer ingresados de forma no programada debido a una enfermedad aguda asociada con la enfermedad oncológica.
IntervencionesNinguna.
Variables principalesLas variables analizadas fueron los datos demográficos, escalas pronósticas de gravedad y el estado clínico del paciente. Se analizó la mortalidad y los factores relacionados con ésta. Se aplicó un análisis de regresión logística binaria multivariante.
ResultadosSe incluyó a un total de 482 pacientes: con tumores sólidos (n=331) y con neoplasias hematológicas (n=171). En el análisis de regresión multivariante, los factores asociados de manera independiente con la mortalidad en la UCI fueron la puntuación APACHE II (OR 1,102; IC del 95% 1,064-1,143), el ingreso médico (OR 3,587; IC del 95% 1,327-9,701), el cáncer de pulmón (OR 2,98, IC del 95% 1,48-5,99) y la ventilación mecánica tras las primeras 24h de ingreso en la UCI (OR 2,27; IC del 95% 1,09-4,73), mientras que la no necesidad de ventilación mecánica fue un factor protector (OR 0,15; IC del 95% 0,09-0,28). En el caso de los tumores sólidos, la puntuación APACHE II, el ingreso médico, la administración de antibióticos en las 48 h previas y el cáncer de pulmón fueron variables independientes relacionadas con la mortalidad, y la no necesidad de ventilación mecánica se identificó como un factor protector. En el análisis multivariante, la puntuación APACHE II y la ventilación mecánica al cabo de 24h desde el ingreso en la UCI se asociaron de manera independiente con mortalidad en pacientes con neoplasias hematológicas, mientras que la ausencia de necesidad de ventilación mecánica se consideró como un factor protector. La neutropenia no se identificó con un factor independiente de predicción de mortalidad en la cohorte total de los dos subgrupos.
ConclusionesLos factores de riesgo asociados a mortalidad no diferente significativamente en pacientes con tumores sólidos o neoplasias hemáticas. El retraso de la intubación en los pacientes que requieren ventilación mecánica podría estar asociado con la mortalidad en la UCI.
Not unfrequently, oncological patients need admission to the ICU. A retrospective multicenter Dutch study showed that 6.4% of cancer patients required ICU admission, revealing that the majority of these admissions took place after surgical procedures.1 In another retrospective study, 5.2% of the patients required ICU admission within the first 2 years of cancer diagnosis.2
The majority of the oncological patients are admitted for immediate postoperative care and commonly present a low mortality rate.3 Moreover, in the last decade, the number of unscheduled admissions to the ICU by acute medical conditions related to the cancer has risen considerably worldwide. Improvements in short- and long-term survival rates of these cancer patients have been documented explaining this widespread reality.4 The advent of new targeted therapies and the enhancement of supportive care justify this increment in ICU admissions even in patients with advanced diseases.
Despite these progresses, death rates of oncology patients in the ICU remain substantially high. Therefore, the identification of prognostic factors in critically ill patients is essential. The understanding of factors associated with poor outcome in this high-risk population may assist physicians, patients, and their relatives in deciding treatment options and their intensity.
In the ICU, patients with hematologic malignancies have higher mortality rates than solid cancer patients.5 However, literature is equivocal whether risk factors for mortality differ in patients with solid or hematological malignancies.6,7 In fact, these two populations have been considered significantly different.8 The presence of neutropenia has been associated with a dismal prognosis in cancer and many clinicians are reluctant to admit patients with severe neutropenia in the ICU. However, if neutropenia influences the outcomes of cancer patients in the ICU and whether this influence differs between solid and hematología malignancies is an ongoing debate.9–11
The aims of this study are to identify the risk factors for mortality of oncological patients admitted to the ICU and to perform specific analyses for solid cancers and for hematological malignancy patients in order to determine if these factors are different for the two populations.
MethodsProspective observational study carried out in Spanish ICUs using the ENVIN (National Nosocomial Infection Surveillance Study; Estudio Nacional de Vigilancia de Infección Nosocomial in Spanish) registry. It is an observational, prospective and multicenter (national) project that was started in 1994 by the Study Group of Infectious Diseases and Sepsis (GTEIS) of SEMICYUC. It is performed yearly since April 1st to June 30th. Its objectives have been described in detail elsewhere.12 Data entry is done through a webpage (http://hws.vhebron.net/envin-helics/). The ENVIN registry has been approved by several local and regional Clinical Research Ethics Committees and the specific authorization of patients for data collection is not required, as it is recognized as a Registry of national Interest for the National Health System (year 2014).
In 2018, an extension of cancer patient data was carried out associating a new database called “ONCOENVIN database”. Adult patients (≥18 years) with a clinically confirmed hematologic or solid malignancy admitted to any of the participating ICUs for more than 24h during the three months of the ENVIN registry were included in this study. In the present manuscript, we report exclusively those patients with an unplanned admission due to an acute medical or surgical condition related to the cancer. We excluded patients who were admitted to the ICU for acute conditions not related to their oncological disease (i.e. trauma, acute coronary syndrome, …) and patients admitted after elective surgery.
Variables collected at ICU admission were age, gender, severity of illness assessed by APACHE II score in the first 24h in the ICU, underlying comorbidities, history of surgery within 30 days prior to admission, use of antibiotics in the previous 48h, type of cancer, year of diagnosis, hospital size (less than 200 beds, 200–500, and more than 500 beds), cancer treatments (no treatment, neoadjuvant chemotherapy, adjuvant chemotherapy, first-line and second-line chemotherapy, symptomatic treatment, chemotherapy for hematological malignancy, allogeneic bone marrow transplantation, and autologous bone marrow transplantation), and length of hospital stay before ICU admission. Solid cancers were grouped into nine categories (see footnotes in Table 4 for details). Hematologic malignancies were categorized as: acute leukemia, chronic leukemia, lymphoma, multiple myeloma, and others. Based on their primary reason for admission to the ICU, patients were categorized in the following groups: sepsis/septic shock following Sepsis-3 definitions, acute respiratory failure, renal failure, coma, hemorrhagic shock, severe metabolic disturbances, or others.
During the ICU stay, details regarding the need for invasive mechanical ventilation, renal replacement therapy, development of neutropenia (neutrophils <500/mm3), development of ICU-acquired infection (catheter-related bloodstream infection, ventilator-associated pneumonia, pulmonary aspergillosis), administration of chemotherapy in the ICU, and tumor lysis syndrome13 were collected daily. Diagnosis of pulmonary aspergillosis required host risk factors, suggestive signs of fungal infection on CT scan as well as isolation of Aspergillus spp. in respiratory culture or Galactomannan antigen detection in serum or bronchoalveolar lavage with a significative optical density index.14 All patients were followed up until death or ICU discharge.
Statistical analysisA descriptive analysis was conducted. Categorical variables were summarized with frequencies and percentages, while quantitative variables were described with mean and standard deviation or median (interquartile range) as appropriate. To compare survivors vs non-survivors of the three groups (total cohort, patients with solid malignancy, and patients with hematological malignancy) a bivariate analysis was performed. Chi-square test or Fisher exact test were used according to application conditions for the categorical variables and Mann–Whitney U test was used for quantitative variables. For every group, the significant and marginally significant variables (p<0.1) obtained in the bivariate analysis and the variables considered clinically relevant, were introduced in a multivariate binary logistic regression analysis in order to assess the factors related to death in the ICU. We considered the “Mechanical ventilation in the first 24h of ICU admission” category as the reference and it was compared with the two others (“No mechanical ventilation” and “Mechanical ventilation after 24h of ICU admission”). Variables without statistical significance in the model were subsequently manually removed in a backward step-by-step procedure, until the best possible model was obtained, showing adjusted odds ratio with their 95% confidence intervals and p-values for each of the final variables. Calibration and discrimination power of the model were assessed with Hosmer–Lemeshow test and area under the curve (AUC) respectively. In all analyses, p-values less than 0.05 were considered as statistically significant.
ResultsDuring the study period, 123 Spanish ICUs included oncological patients in the registry. Overall, 2557 cancer patients were admitted to the participating ICUs. Of them, 1506 were scheduled post-operative care, 567 required ICU admission for acute conditions not related to their oncological disease, and 484 patients had an unplanned ICU admission for an acute medical or surgical illness related to a solid or a hematological malignancy. Two of these 484 patients were excluded from the analysis for incomplete data. Therefore, 482 patients comprise the study group of this research. The diagnosis of cancer had been made in 120 patients (24.9%) in the year 2017 or from January to June 2018 in 287 patients (59.5%).
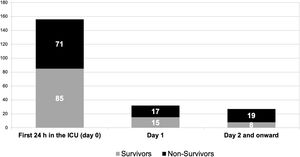
Table 1 depicts the comparison between those patients who were discharged alive from the ICU and those who died in the Unit (mortality rate 29.5%). Of note, age was not statistically different in those who died compared to those who were discharged alive from the ICU. The most common indications for ICU admission were sepsis (n=180) and respiratory insufficiency (n=179). Length of hospital stay before ICU admission was significantly shorter in patients who survived. Hospital bed size did not affect mortality in the total cohort or in the two subgroups. Overall, 215 patients (44.6%) required invasive mechanical ventilation, 156 in the first 24h in the ICU. The overall mortality rate was 49.8% among patients receiving invasive mechanical ventilation. Mortality rate was greater (p test of Fisher=0.0478) in those patients on mechanical ventilation in the first 24h compared to those intubated on day two and onwards (45.5% vs 61%). By multivariate logistic regression analysis, factors independently associated with mortality were APACHE II, medical admission, lung cancer, and mechanical ventilation after 24h of ICU admission whereas no need of mechanical ventilation was a protective factor (Table 2). Fig. 1 shows the number of deaths for the different subgroups of patients depending on the day of invasive mechanical ventilation onset. The demographics data and clinical features of those patients intubated in the first 24h in the ICU (n=156; mortality rate 45.5%) compared with those intubated on day 2 and onward (n=59; mortality rate 61%) is shown in Table 3.
Comparison between survivors and non-survivors in the total cohort.
| Survivors(n=340) | Non-survivors(n=142) | p | |
|---|---|---|---|
| Mean age (yr.) median, IQR | 63 (53–70) | 64 (54–71) | 0.28 |
| Gender (female) n (%) | 106 (31.2) | 51 (35.9) | 0.31 |
| APACHE II median, IQR | 17 (12–22) | 23 (18–28) | <0.001 |
| Medical admission | 268 (78.8) | 127 (89.4) | 0.006 |
| Length of hospital stay before ICU admission | 1 (0–7) | 3 (0–15) | <0.001 |
| Underlying conditions | |||
| COPD | 37 (10.9) | 17 (12) | 0.73 |
| Cirrhosis | 5 (1.5) | 3 (2.1) | 0.61 |
| Diabetes mellitus | 55 (19.4) | 23 (16.2) | 0.40 |
| Chronic renal insufficiency | 34 (10) | 13 (9.2) | 0.77 |
| Hypoalbuminemia* | 55 (16.2) | 30 (21.1) | 0.19 |
| Neutropenia at ICU admission | 66 (19.4) | 23 (16.2) | 0.41 |
| Surgery in the previous 30 days | 72 (21.2) | 15 (10.6) | 0.006 |
| Antibiotics in the previous 48h | 157 (46.2) | 88 (62) | 0.002 |
| Type of cancer | |||
| Solid cancer (except lung) | 180 (52.9) | 51 (35.9) | 0.002 |
| Lung | 48 (14.1) | 32 (22.5) | |
| Hematological | 112 (32.9) | 59 (41.5) | |
| Status of malignancy | |||
| No treatment | 94 (27.6) | 38 (26.8) | 0.045 |
| Neoadjuvant chemotherapy | 29 (8.5) | 11 (7.7) | |
| Adjuvant chemotherapy | 41 (12.1) | 6 (7.2) | |
| First line chemotherapy | 44 (12.2) | 24 (16.9) | |
| Second and subsequent lines | 37 (10.9) | 15 (10.6) | |
| Chemotherapy for acute hematological malignancy | 31 (9.1) | 19 (13.4) | |
| HSCT | 16 (1.8) | 9 (4.9) | |
| Others | 35 (10.3) | 10 (7) | |
| Cause of admission | |||
| Respiratory failure | 113 (33.2) | 66 (46.5) | 0.01 |
| Sepsis | 131 (38.5) | 49 (34.5) | |
| Other** | 96 (28.2) | 27 (19) | |
| Mechanical ventilation | 108 (31.8) | 107 (75.4) | <0.001 |
| Onset of mechanical ventilation | |||
| No mechanical ventilation | 232 (65.4) | 35 (24.6) | <0.001 |
| Mechanical ventilation in the first 24h of admission | 85 (25) | 71 (50) | |
| Mechanical ventilation after 24h of admission | 23 (6.8) | 36 (25.4) | |
| Renal replacement therapy | 15 (4.4) | 28 (19.7) | <0.001 |
| Total parenteral nutrition | 45 (13.2) | 23 (16.2) | 0.39 |
| ECMO | 1 (0.3) | 1 (0.7) | 0.52 |
| Complications in the ICU | |||
| Primary bacteremia | 6 (1.8) | 2 (1.4) | 1.000 |
| VAP | 6 (1.8) | 7 (4.9) | 0.051 |
| Pulmonary aspergillosis | 3 (0.9) | 8 (5.6) | 0.016 |
| Neutropenia developed in the ICU | 58 (17.1) | 29 (20.4) | 0.386 |
| Tumor lysis syndrome | 6 (1.8) | 11 (7.7) | 0.001 |
IQR: interquartile range; COPD: chronic obstructive pulmonary disease; ECMO: extracorporeal membrane oxygenation; HSCT: hematopoietic stem cell transplantation; VAP: ventilator-associated pneumonia.
Logistic regression analyses.
| AdjustedOR (95% CI) | p | |
|---|---|---|
| Total cohort | ||
| APACHE II score | 1.10 (1.06–1.14) | <0.001 |
| Medical admission | 3.59 (1.33–9.70) | 0.012 |
| Type of cancer | ||
| Solid cancer (except lung) | 1 | |
| Lung | 2.98 (1.48–5.99) | 0.002 |
| Hematological | 1.58 (0.88–2.83) | 0.12 |
| Mechanical ventilation | ||
| Mechanical ventilation in the first 24h of admission | 1 | |
| Mechanical ventilation after 24h of admission | 2.27 (1.09–4.73) | 0.028 |
| No mechanical ventilation | 0.15 (0.09–0.28) | <0.001 |
| Patients with solid malignancy | ||
| APACHE II score | 1.123 (1.07–1.178) | <0.001 |
| Medical admission | 5.37 (1.71–16.81) | 0.004 |
| Antibiotics in the previous 48h | 2.36 (1.21–4.62) | 0.012 |
| Lung cancer | 2.88 (1.42–5.83) | 0.003 |
| Mechanical ventilation | ||
| Mechanical ventilation in the first 24h of admission | 1 | |
| Mechanical ventilation after 24h of admission | 1.18 (0.41–3.37) | 0.76 |
| No mechanical ventilation | 0.17 (0.08–0.35) | <0.001 |
| Patients with hematological malignancy | ||
| APACHE II score | 1.08 (1.02–1.14) | <0.001 |
| Mechanical ventilation | ||
| Mechanical ventilation in the first 24h of admission | 1 | |
| Mechanical ventilation after 24h of admission | 4.36 (1.41–13.46) | <0.01 |
| No mechanical ventilation | 0.14 (0.05–0.35) | <0.001 |
ICU mortality for the different subgroups of patients with cancer depending on the day of invasive mechanical ventilation initiation.
In patients intubated on day 2 and onward, the distribution of survivors/non-survivors is as follows: day 2: 4/6; day 3: 3/4; day 4: 1/4; day 5: 0/2; day 6 and onward: 0/3.
Patients’ characteristics of those with invasive mechanical ventilation on day 1 of ICU admission compared with those with invasive mechanical ventilation after 24h in the ICU (day 2 and onward).
| MV within first 24h of admission(n=156) | MV after 24h of admission(n=59) | p | |
|---|---|---|---|
| Mean age (yr.) median, IQR | 62 [53–71] | 58 [48–66] | 0.012 |
| Gender (female) n (%) | 51 (32.7%) | 20 (33.9%) | 0.867 |
| APACHE II median, IQR | 22 [16–27] | 19 [15–24] | 0.045 |
| Medical admission | 120 (76.9%) | 55 (93.2%) | 0.006 |
| Length of hospital stay before ICU admission | 5 [2–17] | 10 [3–23] | 0.154 |
| Underlying conditions | |||
| COPD | 19 (12.2%) | 8 (13.6%) | 0.785 |
| Cirrhosis | 3 (1.9%) | 1 (1.7%) | 1.000 |
| Diabetes mellitus | 29 (18.6%) | 9 (15.3%) | 0.567 |
| Chronic renal insufficiency | 16 (10.3%) | 6 (10.2%) | 0.985 |
| Hypoalbuminemia* | 31 (19.9%) | 13 (22.0%) | 0.726 |
| Neutropenia at ICU admission | 28 (17.9%) | 15 (25.4%) | 0.221 |
| Surgery in the previous 30 days | 36 (23.1%) | 9 (15.3%) | 0.208 |
| Antibiotics in the previous 48h | 72 (46.2%) | 41 (69.5%) | 0.002 |
| Type of cancer | |||
| Solid cancer (except lung) | 84 (53.8%) | 22 (37.3%) | 0.001 |
| Lung | 27 (17.3%) | 4 (6.8%) | |
| Hematological | 45 (28.8%) | 33 (55.9%) | |
| Status of malignancy | |||
| No treatment | 50 (32.1%) | 11 (18.6%) | 0.106 |
| Neoadjuvant chemotherapy | 10 (6.4%) | 6 (10.2%) | |
| Adjuvant chemotherapy | 14 (9.0%) | 2 (3.4%) | |
| First line chemotherapy | 25 (16.0%) | 12 (20.3%) | |
| Second and subsequent lines | 16 (10.3%) | 3 (5.1%) | |
| Chemotherapy for acute hematological malignancy | 14 (9.0%) | 10 (16.9%) | |
| HSCT | 5 (3.2%) | 5 (8.5%) | |
| Others | 22 (14.1%) | 10 (17%) | |
| Cause of admission | |||
| Respiratory failure | 63 (40.4%) | 33 (55.9%) | 0.105 |
| Sepsis | 51 (32.7%) | 16 (27.1%) | |
| Other | 42 (26.9%) | 10 (16.9%) | |
| Mechanical ventilation | – | – | |
| Renal replacement therapy | 1 (0.6%) | 0 (0.0%) | 1.000 |
| Total parenteral nutrition | 30 (19.2%) | 13 (22.0%) | 0.647 |
| ECMO | 1 (0.6%) | 1 (1.7%) | 0.474 |
| Complications in the ICU | |||
| Primary bacteremia | 5 (3.2%) | 2 (3.4%) | 1.000 |
| VAP | 9 (5.8%) | 4 (6.8%) | 0.647 |
| Pulmonary aspergillosis | 8 (5.1%) | 3 (5.2%) | 1.000 |
| Neutropenia developed in the ICU | 22 (14.1%) | 15 (25.4%) | 0.050 |
| Tumor lysis syndrome | 4 (2.6%) | 7 (11.9%) | 0.011 |
IQR: interquartile range; COPD: chronic obstructive pulmonary disease; ECMO: extracorporeal membrane oxygenation; HSCT: hematopoietic stem cell transplantation; VAP: ventilator-associated pneumonia.
To better understand whether these risk factors differ between patients with solid cancer (n=311) and hematological malignancies (n=171), we analyzed these two cohorts separately. Patients with hematological cancer were younger [61 years (51–70) vs 64 years (55–71); p=0.046] and with higher APACHE II score [20 (15–25) vs 17 (12–23); p=0.007] than those with solid cancer. Length of hospital stay before ICU admission was significantly shorter in patients with solid tumor [1 day (0–4) vs 4 days (0–16); p<0.001]. Length of ICU stay was not statistically different in both groups: 5 days3–9 for subjects with solid cancer vs 6 days4–11 for hematological patients (p=0.056).
Neutropenia at admission to the ICU was significantly more common in hematological patients than in solid tumors (36.8% vs 9.9%; p<0.0001). The rate of patients requiring invasive mechanical ventilation was similar in these two groups: 45.6%. vs 44%. Chemotherapy was more frequently administered in the ICU in hematological than in solid tumor patients (15.8% vs 2.25%; p<0.001). Mortality was not statistically different in these two groups of patients: 51.8% vs 36.4% (p=0.072).
Table 4 shows the comparison between survivors and non-survivors in patients with solid cancer. The commonest solid malignancy was lung cancer (25.7%) followed by colon (14.8%) and urologic (13.8%) cancers. Mortality was significantly higher in patients with lung cancer than in patients with other solid malignancies (40% vs 22%; p=0.0017). Urological and gynecological cancers presented the lowest mortality rate (16.6 and 18.7%, respectively). Only 7 patients received chemotherapy in the ICU (4 survived). The multivariate logistic regression analysis identified five factors as independently associated with mortality and another (no need of mechanical ventilation) was a protective variable (Table 2).
Comparison between survivors and non-survivors in solid cancer patients.
| Survivors(n=228) | Non-survivors(n=83) | p | |
|---|---|---|---|
| Mean age (yr.) median, IQR | 63 (54.5–71) | 65 (57–73) | 0.10 |
| Gender (female) n (%) | 70 (30.7) | 30 (36.1) | 0.415 |
| APACHE II median, IQR | 16 (12–21) | 23 (18–28) | <0.001 |
| Medical admission | 162 (71.1) | 71 (85.5) | 0.009 |
| Length of hospital stay before ICU admission | 0.5 (0–4) | 2 (0–8) | <0.001 |
| Underlying conditions | |||
| COPD | 29 (12.7) | 12 (14.5) | 0.68 |
| Cirrhosis | 2 (0.9) | 2 (2.4) | 0.28 |
| Diabetes mellitus | 45 (19.7) | 17 (20.5) | 0.40 |
| Chronic renal insufficiency | 24 (10.5) | 9 (10.8) | 0.92 |
| Hypoalbuminemia | 40 (17.5) | 18 (21.7) | 0.41 |
| Neutropenia at ICU admission | 27 (11.8) | 4 (4.8) | 0.067 |
| Previous surgery | 66 (28.9) | 12 (14.5) | 0.009 |
| Antibiotics in the previous 48h | 86 (37.7) | 42 (50.6) | 0.041 |
| Type of cancer | |||
| Solid cancer (except lung)* | 180 (78.9) | 51 (61.4) | 0.002 |
| Lung | 48 (21.2) | 32 (38.6) | |
| Status of malignancy | |||
| No treatment | 82 (36) | 30 (36.1) | 0.102 |
| Neoadjuvant chemotherapy | 26 (11.4) | 7 (8.4) | |
| Adjuvant chemotherapy | 35 (15.4) | 6 (7.2) | |
| First line chemotherapy | 26 (10.9) | 15 (18.1) | |
| Second and subsequent lines | 28 (12.3) | 11 (13.3) | |
| Others | 41 (17.2) | 14 (16.8) | |
| Cause of admission | |||
| Respiratory failure | 66 (28.9) | 41 (49.4) | 0.004 |
| Sepsis | 88 (38.6) | 23 (27.7) | |
| Other** | 74 (32.5) | 19 (22.9) | |
| Mechanical ventilation | 79 (34.6) | 58 (69.9) | <0.001 |
| Onset of mechanical ventilation | |||
| No mechanical ventilation | 149 (65.4) | 25 (30.1) | <0.001 |
| Mechanical ventilation in the first 24h of admission | 64 (28.1) | 47 (56.6) | |
| Mechanical ventilation after 24h of admission | 15 (6.6) | 11 (13.1) | |
| Renal replacement therapy | 10 (4,4) | 9 (10.8) | 0.03 |
| Total parenteral nutrition | 33 (14.5) | 12 (14.5) | 1 |
| ECMO | 0 (0) | 1 (1.2) | 0.1 |
| Complications in the ICU | |||
| Primary bacteremia | 6 (1.8) | 2 (2.4) | 0.91 |
| VAP | 6 (1.8) | 7 (4.9) | 0.051 |
| Pulmonary aspergillosis | 1 (0.4) | 5 (6) | 0.01 |
| Neutropenia developed in the ICU | 25 (11) | 4 (4.8) | 0.099 |
| Tumor lysis syndrome | 2 (0.9) | 2 (2.4) | 0.289 |
IQR: interquartile range; COPD: chronic obstructive pulmonary disease; ECMO: extracorporeal membrane oxygenation.
Lymphoma was the commonest hematological malignant disease in our series and the great majority of hematological patients had a medical cause of ICU admission (Table 5). Twenty-seven patients received chemotherapy in the ICU (mortality rate 33%). As expected, allogenic HSCT (hematopoietic stem cell transplantation) had the highest mortality rate (58.3%). In the multivariate analysis, only APACHE II and mechanical ventilation after 24h of ICU admission were independently associated with mortality while no need of mechanical ventilation was a protective factor (Table 2). As in the previous analyses, neutropenia was not included in the final model.
Hematological malignancies: Comparison between survivors and non-survivors.
| Survivors(n=112) | Non-survivors(n=59) | p | |
|---|---|---|---|
| Mean age (yr.) median, IQR | 62 (51–70) | 62 (52–69) | 0.91 |
| Gender (female) n (%) | 36 (32.1) | 21 (35.6) | 0.65 |
| APACHE II median, IQR | 19 (13–23) | 22 (19–27) | <0.001 |
| Medical admission | 106 (94.4) | 56 (94.9) | 0.94 |
| Length of hospital stay before ICU admission | 3 (0–14) | 7 (1–18) | 0.14 |
| Underlying conditions | |||
| COPD | 8 (7.1) | 5 (8.5) | 0.75 |
| Cirrhosis | 3 (2.7) | 1 (1.7) | 0.69 |
| Diabetes mellitus | 21 (18.8) | 6 (10.2) | 0.14 |
| Chronic renal insufficiency | 24 (10.5) | 9 (10.8) | 0.92 |
| Neutropenia at ICU admission | 39 (34.8) | 24 (40.7) | 0.45 |
| Previous surgery | 6 (5.4) | 3 (5.1) | 0.94 |
| Type of cancer | |||
| Acute leukemia | 36 (32.1) | 24 (40.7) | 0.174 |
| Lymphoma | 45 (40.2) | 26 (40.1) | |
| Other | 31 (27.7) | 9 (15.3) | |
| Status of malignancy | |||
| No treatment | 12 (10.7) | 8 (13.6) | 0.239 |
| Chemotherapy | 86 (76.8) | 42 (71.2) | |
| Allogenic HSCT | 5 (4.5) | 7 (11.9) | |
| Autologous HSCT | 9 (8) | 2 (3.4) | |
| Cause of admission | |||
| Respiratory failure | 47 (42) | 25 (42.4) | 0.57 |
| Sepsis | 43 (38.4) | 26 (44.1) | |
| Other* | 22 (19.6) | 8 (13.6) | |
| Mechanical ventilation | 29 (25.9) | 49 (83.1) | <0.001 |
| Onset of mechanical ventilation | |||
| No mechanical ventilation | 83 (74.1) | 10 (16.9) | <0.001 |
| Mechanical ventilation in the first 24h of admission | 21 (18.8) | 24 (40.7) | |
| Mechanical ventilation after 24h of admission | 8 (7.1) | 25 (42.4) | |
| Renal replacement therapy | 5 (4.5) | 19 (32.2) | <0.001 |
| Total parenteral nutrition | 12 (10.7) | 11 (18.6) | 0.149 |
| ECMO | 1 (0.9) | 0 (0) | 0.467 |
| Complications in the ICU | |||
| Primary bacteremia | 6 (1.8) | 2 (3.4) | 0.56 |
| VAP | 1 (0.9) | 3 (5.1) | 0.085 |
| Pulmonary aspergillosis | 2 (1.8) | 3 (5.1) | 0.205 |
| Neutropenia developed in the ICU | 33 (29.5) | 25 (42.4) | 0.099 |
| Tumor lysis syndrome | 4 (3.6) | 9 (15.3) | 0.006 |
IQR: interquartile range; COPD: chronic obstructive pulmonary disease; ECMO: extracorporeal membrane oxygenation; HSCT: hematopoietic stem cell transplantation.
* Other causes of admission: hemorrhagic shock: 3; coma: 7; renal failure: 4; metabolic disturbances: 3; others: 13.
This prospective and multicenter study has identified several risk factors associated with mortality in cancer patients admitted to the ICU. Clinical features associated with mortality do not significantly differ in solid cancer and in hematological malignancies. It must be highlighted that the initiation of mechanical ventilation after 24h of ICU admission was linked with higher ICU mortality and this effect was also manifest in hematological patients. On the contrary, no need of mechanical ventilation was a protective variable in the entire cohort and in both subgroups (solid and hematological cancers). The poor prognosis in the ICU of lung cancer and medical admissions have been confirmed in this study.
The identification of factors associated with mortality will aide physicians to identify cancer patients who are likely to benefit from ICU care, the use of supportive treatments and the time of their initiation. The majority of the information on the prognosis of patients with cancer patients who are admitted to the ICU derives from retrospective analyses of large databases or from studies carried out in cancer specialized ICUs.
Approximately, two-thirds of our patients had been previously diagnosed with a solid tumor and the remainings had a malignant hematological disease. This proportion of hematological patients is higher than what has been reported by others,4,8 probably reflecting the improvement of the prognosis of these patients. In agreement with previous investigations, respiratory failure and sepsis are the most common reasons for admission.
In our series, medical cancer patients have 3.5 times higher risk of ICU mortality compared with surgical admissions. In a systematic review,15 medical cancer patients had an increased risk of ICU mortality between two- to fourfold compared to surgical patients. Of note, medical admission was not a variable associated with mortality in hematological patients. This can be explained by the fact that less than 5% of these patients had a surgical reason for ICU admission. As expected, severity of illness measured by APACHE II score is associated with greater risks of mortality as generally occurs in previous studies.15 In our data, each point of increment contributes to a 10% increase in the risk of death.
Lung cancer is the commonest tumor type admitted to the ICU and the one with the poorest outcome.15 Lung cancer patients may benefit less from ICU admission than other types of cancers. Importantly, a recent manuscript has demonstrated that from 2011 to 2019, adjusted mortality in cancer patients requiring ICU admission decreased by 9.2% with lung cancer patients having the lowest reduction.16
The impact of cancer stage on mortality has been long debated with conflicting results. Diverse studies suggest that advanced or metastatic cancer was associated with higher ICU or hospital mortality.7,17,18 However, very scarce information is available about the impact on the outcome depending on the type of chemotherapy that is administered before ICU admission. Notably, in our data, the type of chemotherapy received, including second line chemotherapy did not influence the ICU mortality. In addition, administration of chemotherapy in the ICU does not impact on ICU mortality although the long-term prognosis is dismal.19 In comparison to hematological patients, chemotherapy was unfrequently administered to patients with solid tumors.20
We found that neither neutropenia at admission to the ICU nor its development during the ICU stay increases mortality. It is important to point out that we defined severe neutropenia as a neutrophil count below 500/mm3. A recent meta-analysis on individual data that considered neutropenia as a neutrophil count below 1000/mm3 concluded that neutropenia was independently associated with mortality.11
Mechanical ventilation has been identified as an independent predictor of mortality by previous studies.6,8,9,21,22 However, very few information is available about the impact on prognosis of delayed intubation. Inconsistent data have been published regarding the harm or benefit of noninvasive mechanical ventilation (NIV) in these patients. Others have documented that the use of NIV is associated with increased mortality because it delays endotracheal intubation and mechanical ventilation.23 A recent multicenter study concluded that the need of invasive mechanical ventilation in immunocompromised patients (85% of them with cancer) after NIV or high flow nasal cannula (HFNC) failure, was associated with mortality with higher likelihoods of mortality in case of NIV or HFNC failure.24 Conversely, cancer patients undergoing initial invasive MV had an increased ICU and hospital mortality.25 This discrepancy may in part be explained by differences in the case mix, admission criteria, and treatment protocols.
Our data demonstrate that no intubation in the ICU was an independent protective factor for mortality, observing that mechanical ventilation onset beyond the first day in ICU increased the risk of a fatal outcome compared to those who were intubated in the first 24h. In other words, the use of prolonged periods to avoid intubation might not be considered the standard of care since this delay is associated with an increased probability of death. In our experience, patients intubated after 24h in the ICU are younger, with lower APACHE II score, mostly medical patients and with hematological malignancy in comparison with those intubated in the first day. We cannot rule out that in some cases, delayed intubation may have been explained by a poor prognosis of these patients since mechanical ventilation it is recognized as an independent predictor of mortality.
We acknowledge several limitations of this study. First, hospital or long-term mortalities were not recorded in our database admitting their importance in cancer patients. Second, since the use of NIV, HFNC or the reason for intubation were not recorded we cannot explore whether these interventions might have been associated with a higher mortality. Third, failure of organs was not monitored throughout the length of ICU stay. Finally, as this is an observational study, management of patients was not standardized and different treatment protocols were used in the participating units.
Some strengths of our research should also be highlighted. This is a prospective, multicenter study with a relatively large number of patients enrolled, in polyvalent ICUs across Spain and therefore reflecting the real-life situations. All the clinical predictors identified as independently associated with mortality are easily available and may help to identify cancer patients who may not benefit from intensive care or the use of aggressive therapies.
In summary, identifying the determinants of outcomes in critically ill patients with cancer is crucial to improve the use of the ICU avoiding unnecessary advanced life support. The long-held belief about the worse prognosis of cancer patients with neutropenia in the ICU is not supported by our data. Similarly, the type of chemotherapy that the patient is receiving does not influence the short-term outcome. Although the intubation of a critically ill cancer patient is frequently a stressful decision, our data suggest that it should not be delayed because it worsens the patient chance of survival. The prognosis of lung cancer requiring ICU admission is worse than in any other type of cancer including hematological malignancies. All this information may be of aid for clinicians involved in critically ill cancer patient management but larger studies with a longer follow-up are warranted to more precisely define the patient who will benefit from ICU admission optimizing the use of ICU resources.
FundingNone declared.
Conflicts of interestThe authors report no conflicts of interest. JGM and PO are the project coordinators, they designed the study protocol and contacted the researchers. SM has performed statistical analysis. JGM and MLCB have written the contents of the manuscript. All researchers have participated in the inclusion of cases and have reviewed the version of the manuscript.