To determine whether extension to holidays and weekends of the protocol for the early proactive detection of severity in hospital (“ICU without walls” project) results in decreased mortality among patients admitted to the ICU during those days.
DesignA quasi-experimental before–after study was carried out.
SettingA level 2 hospital with 210 beds and a polyvalent ICU with 8 beds.
Patients or participantsThe control group involved no “ICU without walls” activity on holidays or weekends and included those patients admitted to the ICU on those days between 1 January 2010 and 30 April 2013. The intervention group in turn extended the “ICU without walls” activity to holidays and weekends, and included those patients admitted on those days between 1 May 2013 and 31 October 2014. Patients arriving from the operating room after scheduled surgery were excluded.
Variables of interestAn analysis was made of the demographic variables (age, gender), origin (emergency room, hospital ward, operating room), type of patient (medical, surgical), reason for admission, comorbidities and SAPS 3 score as a measure of severity upon admission, stay in the ICU and in hospital, and mortality in the ICU and in hospital.
ResultsA total of 389 and 161 patients were included in the control group and intervention group, respectively. There were no differences between the 2 groups except as regards cardiovascular comorbidity (49% in the control group versus 33% in the intervention group; P<.001), severity upon admission (median SAPS 3 score 52 [percentiles 25–75: 42–63) in the control group versus 48 [percentiles 25–75: 40–56] in the intervention group; P=.008) and mortality in the ICU (11% in the control group [95% CI 8–14] versus 3% [95% CI 1–7] in the intervention group; P=.003). In the multivariate analysis, the only 2 factors associated to mortality in the ICU were the SAPS 3 score (OR 1.08; 95% CI 1.06–1.11) and inclusion in the intervention group (OR 0.33; 95% CI 0.12–0.89).
ConclusionsExtension of the “ICU without walls” activity to holidays and weekends results in a decrease in mortality in the ICU.
Estudiar si la ampliación, a festivos y fines de semana, del protocolo de detección proactiva precoz de gravedad en el hospital y actuación de intensivistas en planta convencional y urgencias (actividad «UCI sin paredes») se asocia a una reducción en la mortalidad de los pacientes ingresados en UCI en esos días.
DiseñoEstudio cuasiexperimental before–after.
ÁmbitoHospital de nivel 2 con 210 camas en funcionamiento y UCI polivalente con 8 camas.
Pacientes o participantesEn el grupo control, donde no se realiza la actividad «UCI sin paredes» los fines de semana ni festivos, se incluyeron los pacientes ingresados en la UCI esos días del 1 de enero de 2010 al 30 de abril de 2013. En el grupo intervención se amplió la actividad «UCI sin paredes» a los fines de semana y festivos y se incluyeron los pacientes ingresados esos días del 1 de mayo de 2013 al 31 de octubre de 2014. Se excluyeron los pacientes procedentes de quirófano tras una cirugía programada.
Variables de interésSe analizaron las variables demográficas (edad, sexo), la procedencia (urgencias, planta de hospitalización, quirófano), el tipo de paciente (médico, quirúrgico), el motivo de ingreso, las comorbilidades y el SAPS 3 como puntuación de gravedad al ingreso, estancia en UCI y hospitalaria, además de la mortalidad en la UCI y en el hospital.
ResultadosSe incluyeron en el grupo control 389 pacientes, y 161 en el grupo intervención. No se encontraron diferencias entre ambos grupos, salvo en la comorbilidad cardiovascular (un 49% en el grupo control frente a un 33% en el grupo intervención; p<0,001), en la gravedad al ingreso medida mediante el SAPS 3 (mediana de 52 [percentiles 25–75: 42–63] en el grupo control frente a 48 [percentiles 25–75: 40–56] en el grupo intervención; p=0,008) y en la mortalidad en UCI, que fue de un 11% en el grupo control (IC 95% 8 a 14) frente al 3% (IC 95% 1 a 7) en el grupo intervención (p=0,003). En el análisis multivariable, los 2 únicos factores asociados con la mortalidad en UCI fueron: SAPS 3 (OR 1,08; IC 95% 1,06–1,11) y el pertenecer al grupo intervención (OR 0,33; IC 95% 0,12–0,89).
ConclusionesLa ampliación de la actividad «UCI sin paredes» a los fines de semana y festivos conlleva un descenso en la mortalidad en la UCI.
Patient prognosis, particularly in the case of critically ill individuals, may be influenced by changes in care models occurring during the on-hour and off-hour periods.1–4 In our setting, and although survival in all the periods was greater than predicted by the severity indicators, admission to the Intensive Care Unit (ICU) during the off-hours period (i.e., patients admitted in the course of the night shift of weekdays, weekends and holidays [WE-H]) was found to be independently associated to mortality when compared with the on-hours group (patients admitted in the course of the morning and afternoon shifts of weekdays).5 These findings are consistent with the published literature.1,2 A special feature in our case has been the development of the “ICU without walls” project, which is based on the early detection of patients at risk in hospital but outside the ICU, and allows us to intervene early in conventional wards. A before–after study published by our group showed this activity to offer benefit in terms of patient clinical outcome.6 However, the ICU without walls activity was limited to weekdays and was not carried out on WE-H. In the multivariate analysis, the variables independently associated to hospital mortality were found to be the SAPS 3 score and the fact of belonging to the WE-H subgroup.
These results support the idea that the early detection of potentially seriously ill patients, and their consequent improved survival,6–10 could help explain the lesser mortality observed in the on-hours group, where ICU without walls activity was applied.5
The hypothesis of the present study is that extending the ICU without walls project to WE-H has an impact upon mortality among patients who are admitted during that time interval. The primary objective was to determine whether extension to WE-H of the proactive early detection of severity in hospital and the intervention of intensivists in conventional wards and in the emergency room (ICU without walls activity) is associated to a decrease in mortality among patients admitted to the ICU on those days.
Patients and methodsA quasi-experimental before–after study was conducted in an adult polyvalent medical-surgical ICU with 8 beds belonging to a second-level hospital with 210 beds. An agreement was reached with hospital management to extend the early detection of severity system to WE-H. This did not really imply any change in the personnel present on WE-H in our center; accordingly, we maintained an intensivist on duty and a second intensivist during 8h in the morning shift–with addition of the ICU without walls activity during the intervention period. A description of the working protocol can be found in the study published by Abella et al.5
- -
In the control group (analyzed in the previous study),5 ICU without walls activity was not carried out, and inclusion was made of the patients admitted to the ICU on WE-H from 1 January 2010 to 30 April 2013.
- -
In the intervention group, ICU without walls activity was extended to WE-H, and inclusion was made of the patients admitted to the ICU on WE-H from 1 May 2013 to 31 October 2014.
- -
Patients admitted following scheduled surgery were excluded.
An analysis was made of the patient demographic variables (age, sex), origin (emergency care, hospital ward, operating room), type of patient (medical, surgical), reason for admission, comorbidities (defined as comorbidity reflected in the case history, with the present or past administration of treatment for that chronic disease), the SAPS 3 as severity score upon admission, organ failure during admission to the ICU based on the SOFA score, stay in the ICU and in hospital, and mortality in the ICU and in hospital.
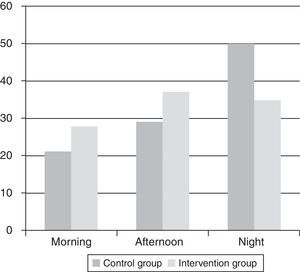
An analysis was also made of the changes in percentage admissions in the course of the morning, afternoon and night shifts, in order to evaluate the effect of extending the ICU without walls activity to WE-H upon the time of patient admission.
The study was approved by the local Ethics Committee. A retrospective analysis of the results was made after implementing the change in management model.
Statistical analysisContinuous variables were reported as the mean or median (percentiles), depending on the type of distribution. The Kolmogorov-Smirnov test was used to assess normality of distribution of the continuous variables, and comparisons were made using the nonparametric Mann–Whitney U-test (for variables with a non-normal distribution) or the Student t-test (for variables with a normal distribution). Categorical variables were compared using the chi-squared test.
A stepwise multivariate logistic regression analysis was made to explore correlations to mortality in the ICU and assess the possible effect of the intervention group upon outcome, entering all the variables that clinically might be related to survival (sex, age, type of patient, origin, comorbidities and SAPS 3 score). Statistical significance was considered for P<0.05 in all cases.
ResultsThe control group comprised 389 patients, while 161 patients were included in the intervention group. There were no differences between the groups in terms of age, sex, origin, type of patient, reason for admission, or organ failure during admission to the ICU (Table 1).
Demographic variables of the two groups.
| Control group (n=389) | Intervention group (n=161) | P-value | |
|---|---|---|---|
| Age in years, median (percentiles 25–75) | 64 (52–76) | 64 (53–75) | 0.82 |
| Sex, n (%) | 0.65 | ||
| Males | 236 (61) | 101 (63) | |
| Females | 153 (39) | 60 (37) | |
| Origin, n (%) | 0.26 | ||
| Emergency room | 283 (73) | 113 (70) | |
| Ward | 49 (13) | 16 (10) | |
| Operating room | 57 (14) | 32 (20) | |
| Type of patient, n (%) | 0.14 | ||
| Medical | 323 (83) | 125 (78) | |
| Surgical | 66 (17) | 36 (22) | |
| Reason for admission, n (%) | 0.08 | ||
| Sepsis | 59 (15) | 20 (12) | |
| Ischemic heart disease | 106 (27) | 53 (33) | |
| Cardiac arrest | 9 (2) | 0 | |
| Other medical reason | 168 (44) | 61 (38) | |
| Postoperative | 47 (12) | 27 (17) | |
| Comorbidities, n (%) | |||
| Cardiovascular | 189 (49) | 53 (33) | <0.001 |
| Respiratory | 84 (22) | 40 (25) | 0.41 |
| Renal | 50 (13) | 16 (10) | 0.34 |
| Hepatic | 19 (5) | 13 (8) | 0.15 |
| Oncological | 51 (13) | 23 (14) | 0.71 |
| Endocrine | 107 (28) | 35 (22) | 0.16 |
| Organ failure developing during stay (SOFA scale) | |||
| Cardiovascular failure, n (%) | 159 (41) | 68 (42) | 0.77 |
| Respiratory failure, n (%) | 184 (47) | 66 (41) | 0.17 |
| Renal failure, n (%) | 99 (25) | 31 (19) | 0.12 |
| SAPS 3, median (percentiles 25–75) | 52 (42–63) | 48 (40–56) | 0.008 |
SAPS 3: simplified acute physiology score; SOFA: sequential organ failure assessment.
Although most of the comorbidities were comparable, there was a statistically significant difference in terms of cardiovascular morbidity (present in 49% of the cases in the control group versus in 33% of the cases in the intervention group) (P<0.001). Significant differences were also observed in terms of severity upon admission as assessed by the SAPS 3 scale, with a median score of 52 (percentiles 25–75: 42–63) in the control group versus 48 (percentiles 25–75: 40–56) in the intervention group (P=0.008) (Table 1). The predicted in-hospital mortality in both groups was 24% and 19%, respectively.
The mean stay in the ICU and in hospital after discharge from the ICU showed no differences between the two groups, with a median stay of three days (percentiles 25–75: 2–4) in the ICU in the control group (P=0.15) versus three days (percentiles 25–75: 2–4) in the intervention group, and with a median stay of four days (percentiles 25–75: 1–9) after discharge from the ICU in the control group versus 5 days (percentiles 25–75: 1–9) in the intervention group (P=0.67).
The mortality rate in the ICU was 11% in the control group (95% confidence interval [95%CI] 8–14) versus 3% in the intervention group (95%CI 1–7) (P=0.003), with an absolute risk reduction of 8% (95%CI 3–12). The difference referred to in-hospital mortality was also statistically significant, with 14% (95%CI 11–18) in the control group versus 6% (95%CI 3–11) in the intervention group (P=0.013), with an absolute risk reduction of 8% (95%CI 2–12).
Variations were observed in the percentage of admissions in the course of the morning, afternoon and night shifts between the two groups. In this regard, an increase in the percentage of admissions was recorded in the morning and afternoon shifts, with a decrease in the night shift, in the intervention group (Fig. 1).
In the multivariate analysis, the only two factors associated to mortality in the ICU were the SAPS 3 score (odds ratio [OR] 1.08; 95%CI 1.06–1.11) and the fact of belonging to the intervention group (OR 0.33; 95%CI 0.12–0.89).
DiscussionIn the present study, although patient survival was greater than predicted by the severity indicators employed, those subjects in the intervention group who were admitted to the ICU on WE-H, following extension of the ICU without walls activity to those days, were seen to have a better prognosis than the patients in the control group admitted to the ICU on WE-H in the absence of ICU without walls activity on those days.
The ICU without walls protocol has been designed for the early detection of patients at risk in the hospital, outside the ICU, and allows us to intervene before the patient suffers organ failure. Such anticipation has been evaluated in different studies,7–13 fundamentally based on the fact that life-threatening situations are usually preceded by detectable and preventable physiopathological alterations. This is particularly notorious in the case of time-dependent illnesses such as for example sepsis, acute coronary syndrome or cardiac arrest.14–17 Specific alarm systems are being developed that combine clinical and laboratory test data, and which offer decision algorithms for initial intervention and the need to inform the ICU.18–21 The worldwide initiative represented by the Surviving Sepsis Campaign has improved adherence to the clinical practice guides, and has resulted in benefits for patients of this kind, with a shortening of hospital stay and even reductions in mortality.22–24
This concept of early action has become so important that the recommendations of the European Resuscitation Council for the management of cardiac arrest include as first link in the “chain of survival” the adoption of measures destined to prevent cardiac arrest through the detection of previously manifesting physiopathological alterations.25
The recent systematic review published by Winters et al.26 reveals that many hospitals have developed rapid response teams with the aim of ensuring early detection and rapid response to situations of clinical worsening in patients admitted to conventional wards. Furthermore, different studies have demonstrated a decrease in cardiac arrest and also in mortality as a result of the introduction of such teams.
This is the case of the study published by Schmidt et al.,13 which described a time relationship between the introduction of a physiological signs monitoring system and diminished mortality in one hospital (from 7.75% to 6.42%; P<0.0001), with an estimated 397 fewer deaths, while in another center the reduction in mortality was from 7.57% to 6.15% (P<0.0001), with an estimated 372 fewer deaths–these results being a consequence of greater reliability in the recording of vital signs and rapidity in decision making.
In the before–after study published by our group, ICU without walls activity resulted in clinical outcome benefits, improved management of the available healthcare resources, and a decrease in mortality among the patients admitted to the ICU during the project implantation period (OR 0.42; 95%CI 0.18–0.98; P=0.04).6
On the other hand, several studies analyzing differences in patient prognosis according to the time of admission to the ICU and even to other hospital areas have reported poorer survival on weekends1–4,27–29 – though other authors have obtained contradictory results.30–33 For this reason, we decided to investigate whether there are differences in mortality in our concrete setting according to the time of day of admission to the ICU. In this regard, we distinguished between an on-hours group (i.e., patients admitted in the course of the morning or afternoon shifts on weekdays) and an off-hours group (patients admitted in the course of the night shift, WE-H), and found admission to the off-hours group to be independently associated to mortality.5 At that point we raised the hypothesis that ICU without walls activity could have a causal relation to increased survival on weekdays, and conducted a subgroup analysis contrasting weekdays versus WE-H where no ICU without walls activity was carried out. We found admission on WE-H to be independently associated to mortality. However, the non-interventional nature of the study did not allow us to demonstrate this hypothesis, and we were only able to support a possible relationship between ICU without walls activity and differences in mortality.
In the present study we compared the prognosis of patients admitted to intensive care in a group lacking ICU without walls activity on WE-H versus another group in which ICU without walls activity was carried out. The groups were comparable except for cardiovascular comorbidity and severity at the time of admission (both being greater in the control group). This could be explained in terms of the purpose of ICU without walls activity, which seeks early identification and management of patients at risk, i.e., intervention is targeted to less critically ill subjects. In addition to the difference in mortality in the univariate analysis, the logistic regression model found the only two factors associated to mortality in the ICU to be the SAPS 3 score (OR 1.08; 95%CI 1.06–1.11) and the fact of belonging to the intervention group (OR 0.33; 95%CI 0.12–0.89). On the other hand, a change was noted in the distribution of admissions according to work shift–with an increase in the percentage of admissions during the morning and afternoon shifts–thereby facilitating better healthcare resource utilization.
As limitations of our study, mention must be made of its single-center nature and the fact that we used the SAPS 3 as a severity indicator at the time of admission to the ICU. In this respect, in populations with a low incidence of organic failure, this scale overestimates predicted mortality, and this could explain the important difference between predicted and real in-hospital mortality.34 The study period in both groups was moreover different, and this could have resulted in minor bias due to greater seasonal mortality and lesser ICU occupation during the summer months. However, there were no differences in mortality in the control group in any of the periods.
What we have found in these studies is that the favorable results are attributable to:
- 1.
Earlier admission to the ICU of certain patients at risk.
- 2.
Improved patient selection (screening) on deciding admission–some patients being amenable to management in conventional wards without having to occupy an ICU bed, thereby contributing to improve the availability of beds in the Unit.
- 3.
The implementation of plans referred to patient care and limitation of life support measures in the ward, with consensus-based decision making, in order to avoid unnecessary admissions to the ICU.
- 4.
Reduction of in-hospital cardiac arrest.
It was not our intention in this study to analyze the underlying causes (undoubtedly of great interest), but only to evaluate the effect of the organizational change made. In order to analyze these factors (as has been done in earlier studies), a larger sample size and the conduction of possibly multicenter trials would be needed.
Extension of ICU without walls activity to WE-H results in a decrease in patient mortality both in the ICU and in hospital.
Conflicts of interestThe authors declare that they have no conflicts of interest.
Please cite this article as: Abella A, Enciso V, Torrejón I, Hermosa C, Mozo T, Molina R, et al. Efecto sobre la mortalidad de la ampliación a los festivos y fines de semana del proyecto «UCI sin paredes». Estudio before–after. Med Intensiva. 2016;40:273–279.