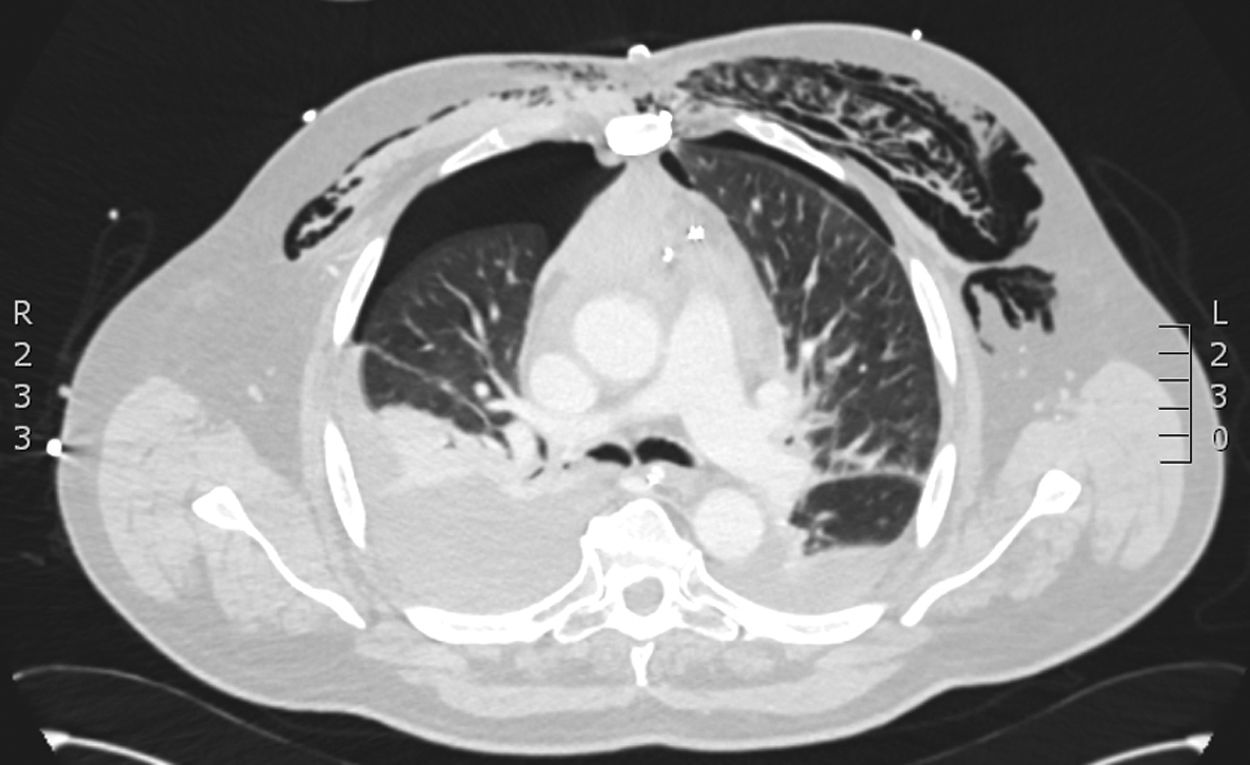
A 71-year-old male in the postoperative period of cardiac surgery presents with respiratory failure, severe hypoxemia, and predominantly left-sided subcutaneous emphysema, requiring re-intubation and 100% FiO2. A chest X-ray could not rule out bilateral pneumothorax. Additionally, he presents with significant hemodynamic instability requiring high doses of norepinephrine, and a distended, tympanic, and painful abdomen on examination, developing hyperlactacidemic acidosis. A CCTA performed confirms the presence of bilateral hydropneumothorax, mediastinal emphysema with involvement of the thoracic wall (Fig. 1), and at abdominal level, a distended bladder with a fluid-air level and atypical intraluminal air consistent with emphysematous cystitis of probable obstructive origin, with the Foley catheter distal end in the membranous urethra (Fig. 2). The Foley catheter was repositioned with the release of abundant gas, and a chest drain was placed. The patient showed progressive improvement with the resolution of emphysematous cystitis on follow-up CCTA.
Conflicts of interestNone declared.
FundingNone declared.