To analyze whether the characteristics of the patients treated by the in-hospital cardiorespiratory arrest team, IHCA and cardiopulmonary resuscitation (CPR) were different in the period before the COVID-19 compared to the pandemic period; also analyzing the differences between COVID+ and COVID− patients.
DesignObservational and retrospective study from January 1st, 2018, to December 31st, 2021.
SettingTertiary hospital.
PatientsAll adult patients over 18 years old requiring attention from the IHCA response team.
InterventionsCPR maneuvers according to the advanced life support guidelines of the European Resuscitation Council published in 2015, as well as the modifications made in the COVID era (2020).
Main variablesDemographic and epidemiological data, activations of the IHCA response team, CA data, hospital and intensive care unit (ICU) length of stay, survival and neurological outcome at hospital discharge.
ResultsA total of 368 patients were analyzed: 173 in the pre-pandemic group and 195 in the pandemic group. The neurological outcome was better in the pre-pandemic group, and COVID+ patients had a longer ICU length of stay. However, no differences in the response time of the CPR team or in CPR duration were found, nor in immediate survival or at hospital discharge, between both groups or between COVID+ and COVID− patients.
ConclusionsChanges in CPR care protocols due to the COVID-19 pandemia did not seem to affect response times from IHCA team neither immediate nor discharge survival.
Analizar las características de los pacientes atendidos por el equipo de atención a la parada cardiorrespiratoria intrahospitalaria (PCIH), las PCIH per se y la reanimación cardiopulmonar (RCP) en el periodo prepandemia por COVID-19 y compararlas con el periodo pandemia, analizando, además, las diferencias entre pacientes COVID+ y COVID−.
DiseñoEstudio observacional y retrospectivo que analiza las activaciones del equipo de PCIH del 1 de enero 2018 al 31 de diciembre 2021.
ÁmbitoHospital de tercer nivel.
PacientesPacientes mayores de 18 años que requirieron asistencia del equipo de atención a la PCIH.
IntervencionesManiobras de RCP según las guías de soporte vital avanzado del European Resuscitation Council publicadas en 2015, así como las modificaciones realizadas en época COVID (2020).
Variables de interés principalesDatos demográficos, epidemiológicos, activaciones del equipo de PCIH, días de estancia en la unidad de cuidados intensivos (UCI) y en la sala de hospitalización, supervivencia y pronóstico neurológico.
Resultados368 pacientes: 173 en el grupo prepandemia y 195 en el grupo pandemia. La recuperación neurológica fue mejor en el grupo prepandemia y la estancia en la UCI fue más prolongada en los pacientes COVID+. Sin embargo, no encontramos diferencias ni en el tiempo de llegada del equipo o en el tiempo de RCP ni en la supervivencia inmediata o al alta hospitalaria entre ambos grupos, ni entre pacientes COVID+ y COVID−.
ConclusionesLos cambios en los protocolos de atención a la parada cardiorrespiratoria debido a la pandemia no parecen haber afectado los tiempos de atención ni la supervivencia inmediata o al alta.
In-hospital cardiac arrest (IHCA) affects approximately 22,000 patients annually in Spain. In Europe, the real incidence of IHCA is uncertain due to many factors, the most important being the lack of universal and comprehensive implementation of registries.1 Incidences between 1.5–2.8 cases per 1000 hospital admissions have been reported.2–4 The associated mortality is high, ranging between 66%–85%, with a significant impact upon short-, middle- and long-term morbidity.5
The characteristics of IHCA differ in many ways from those of out-of-hospital cardiac arrest (CA). One important factor is prevention. In this regard, IHCA is generally preceded by signs and symptoms of clinical deterioration that must be recognized by medical personnel in order to prevent CA. In 1986, our center established the IHCA care team, composed of an anesthesiologist, an internist, a cardiologist and a nurse. It aims to intervene in the event of IHCA occurring in any hospital ward, although it is also activated in situations of clear patient clinical deterioration in order to prevent CA.6 In both scenarios, early patient care is the cornerstone of basic and advanced life support (ALS).7 Early intervention is essential because survival is time-dependent: the longer the delay, the lower the probability of survival.8
The SARS-CoV-2 (Severe Acute Respiratory Syndrome Coronavirus-2) pandemic, declared in March 2020, posed an unprecedented challenge for critical patient care, requiring rapid changes in all protocols.9 The virus mainly affected the respiratory system, generating acute respiratory failure (ARF) and adult respiratory distress syndrome (ARDS) as the main causes of deterioration and IHCA, though cardiovascular causes were also described, with a predominance of non-shockable rhythms.10–12
The European Resuscitation Council (ERC) stated that ALS should never compromise rescuer safety. The most important adaptations of the 2015 ALS guidelines are: minimizing the number of rescuers in contact with the patient; the obligation of donning personal protective equipment (PPE) (at least a screen or goggles, an FFP2 or ideally FFP3 mask, gown and gloves); the avoidance of balloon-mask manual ventilation; and consideration of the use of video laryngoscopy for endotracheal intubation.7–9,14,15
Early studies of IHCA in patients with COVID-19 reported negative results, likely influenced by factors such as fear of infection, use of PPE, nursing overload, and limited resources. This may have affected the response times and, therefore, patient survival.16 In contrast, a 2021 meta-analysis found no significant differences in the return of spontaneous circulation (ROSC) rate, 30-day mortality, or overall mortality compared to the pre-pandemic period. However, it was observed that patients with COVID-19 had higher mortality, both immediately and at discharge.17 The preventive measures implemented may have had an impact on the initiation of resuscitation, length of hospital stay, immediate and discharge survival, and the neurological sequelae.
In Spain, the literature on IHCA before and during the pandemic is scarce. Previous studies, such as those published in 2016 and 2023, found the incidence of CA, survival and the neurological prognosis to be similar to the European and American statistics,4,6 but no specific data compare the pre- and post-pandemic periods. We thus conducted a retrospective study to analyze the activity of the IHCA team at our center, referred to both the team activations and the characteristics of overall cardiac arrest and cardiopulmonary resuscitation (CPR), analyzing the differences before and during the pandemic, as well as between COVID+ and COVID− patients.
Patients and methodsStudy designA retrospective, single-center observational study was carried out in which the activations of the IHCA team were analyzed over four years. The study was approved by the Research Ethics Committee (REC) of our center, with internal code reference number HCB/2021/1075.
The study was conducted at tertiary hospital with a total of 682 conventional hospital beds and 42 ICU beds, which increased exponentially during the pandemic stage. The center has had a multidisciplinary system in place for more than 30 years to manage critical and CA patients outside of the ICUs, operating rooms and emergency departments, which already have their own resuscitation systems. This system is based on a team with trained personnel, the equipment and the infrastructure necessary for initial patient stabilization and the provision of advanced life support, if deemed necessary.
The IHCA care team follows the current ERC guidelines for ALS. During the study period, the team followed the guidelines published in 20157 up until the COVID-19 pandemic, when they complied with the changes introduced by the ERC.9,14
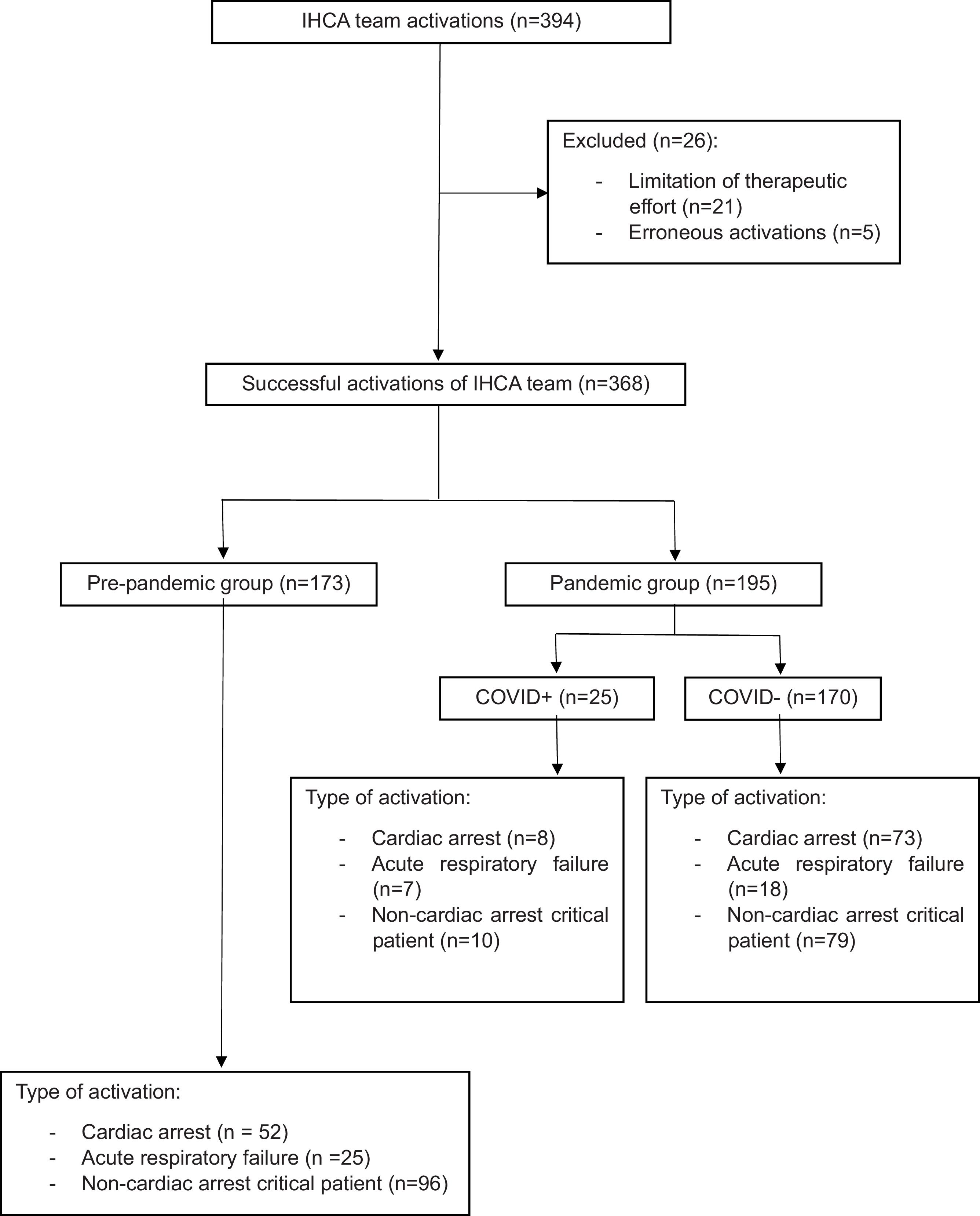
Selection of participants (Fig. 1)Patients over 18 years of age who, while admitted to our center during the study period, required attention by the IHCA care team were included in the study.
Team activations were classified according to activation reason:
- -
ARF: a patient requiring invasive or noninvasive ventilatory support.
- -
CA: a patient who is unconscious, not breathing and requires CPR maneuvers.
- -
Non-arrest critical patient: individuals with signs and symptoms of shock of any cause, and individuals with decreased level of consciousness.
Patients with limitation of therapeutic effort (LTE) instructions and erroneous activations were excluded.
Two groups were compared: “pre-pandemic” (2018–2019) and “pandemic” (2020–2021). In turn, within the pandemic group, two subgroups were analyzed: COVID+ (patients testing positive for COVID-19) and COVID− (patients testing negative for COVID-19).
Study variablesThe study variables were collected using a registry based on the Utstein registry18 completed prospectively upon any activation of the IHCA team.
The following variables were collected:
- •
Demographic characteristics (age, sex, diagnosis at hospital admission, positivity in any COVID-19 detection test, and previous bed rest — with bed rest >50% being defined as having spent more than half the time of admission in bed).
- •
Number and mode of activation of the team (critical patient, ARF or CA), area (conventional or peripheral hospitalization) and activation timetable.
- •
CA data: main cause, time to team arrival, first recorded rhythm and CPR duration.
- •
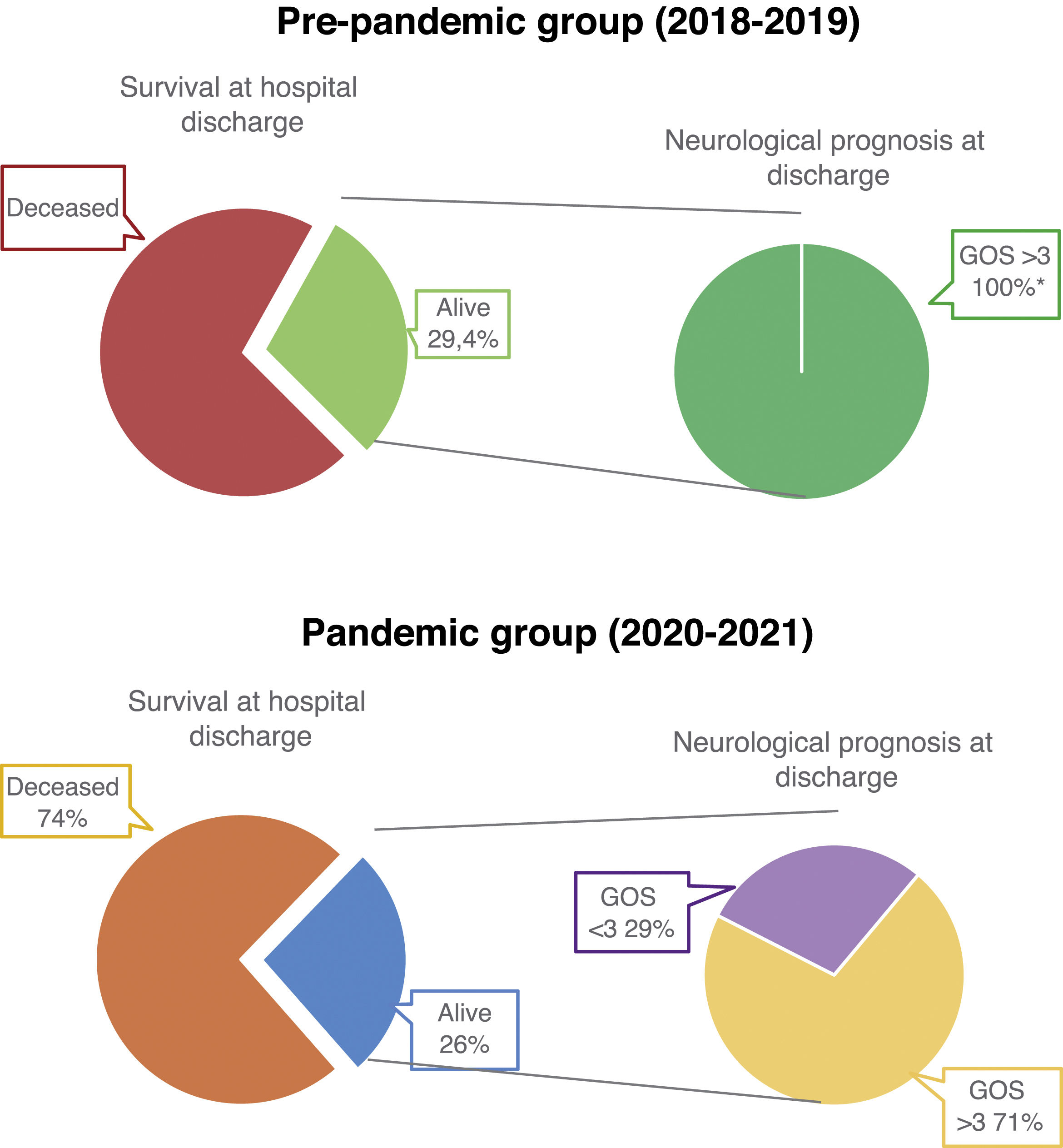
Clinical outcome parameters: immediate survival and survival at discharge, length of ICU and hospital ward stay, and neurological prognosis based on the Glasgow Outcome Scale (GOS) at discharge (Fig. 2).19
Figure 2.Graphical representation of survival at hospital discharge and neurological outcome of patients who suffered a CA during the study period.
*p-value&#¿;<&#¿;0.05, statistically significant.
GOS: Glasgow Outcome Scale, divided into 5 categories: 1 (death), 2 (permanent vegetative state), 3 (severe neurological sequelae: the patient is conscious, with disability and totally dependent), 4 (moderate neurological sequelae: the patient has some disability, but is independent), and 5 (good recovery: the patient may have some minor neurological deficit). Adapted from the original classification described in 1975 by Jennet et al.19
(0.28MB).
- -
A descriptive analysis was performed on patient- and event-related clinical-epidemiological variables and clinical outcome parameters using measures of central tendency and deviation for quantitative variables, and absolute and relative frequencies for categorical variables.
- -
Group and subgroup analyses were performed, using the Student t-test for continuous variables and the chi-square test for categorical variables. Statistical significance was defined as p&#¿;<&#¿;0.05 in all tests.
Missing data were processed by pairwise elimination (analysis of available cases), excluding those observations with missing values for a specific variable. The IBM SPSS version 27.0 statistical package was used throughout.
ResultsFrom January 2018 through December 2021, 394 IHCA team activations were recorded: 188 in the pre-pandemic period and 206 in the pandemic period. Twenty-six were considered incorrect and were excluded from the analysis. Finally, 368 patients were included: 173 in the pre-pandemic group and 195 in the pandemic group.
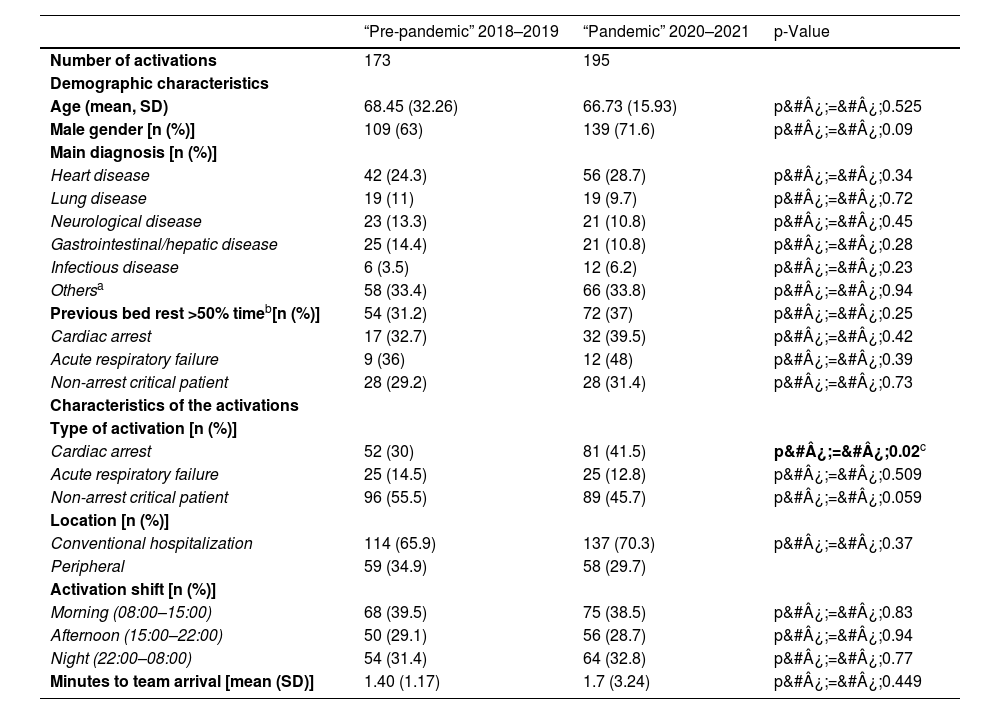
Table 1 shows the demographic and clinical characteristics of the patients who required care by the IHCA team, as well as the characteristics of the activations.
Demographic characteristics of the patients and of the IHCA team activations during the study period.
| “Pre-pandemic” 2018–2019 | “Pandemic” 2020–2021 | p-Value | |
|---|---|---|---|
| Number of activations | 173 | 195 | |
| Demographic characteristics | |||
| Age (mean, SD) | 68.45 (32.26) | 66.73 (15.93) | p&#¿;=&#¿;0.525 |
| Male gender [n (%)] | 109 (63) | 139 (71.6) | p&#¿;=&#¿;0.09 |
| Main diagnosis [n (%)] | |||
| Heart disease | 42 (24.3) | 56 (28.7) | p&#¿;=&#¿;0.34 |
| Lung disease | 19 (11) | 19 (9.7) | p&#¿;=&#¿;0.72 |
| Neurological disease | 23 (13.3) | 21 (10.8) | p&#¿;=&#¿;0.45 |
| Gastrointestinal/hepatic disease | 25 (14.4) | 21 (10.8) | p&#¿;=&#¿;0.28 |
| Infectious disease | 6 (3.5) | 12 (6.2) | p&#¿;=&#¿;0.23 |
| Othersa | 58 (33.4) | 66 (33.8) | p&#¿;=&#¿;0.94 |
| Previous bed rest >50% timeb[n (%)] | 54 (31.2) | 72 (37) | p&#¿;=&#¿;0.25 |
| Cardiac arrest | 17 (32.7) | 32 (39.5) | p&#¿;=&#¿;0.42 |
| Acute respiratory failure | 9 (36) | 12 (48) | p&#¿;=&#¿;0.39 |
| Non-arrest critical patient | 28 (29.2) | 28 (31.4) | p&#¿;=&#¿;0.73 |
| Characteristics of the activations | |||
| Type of activation [n (%)] | |||
| Cardiac arrest | 52 (30) | 81 (41.5) | p&#¿;=&#¿;0.02c |
| Acute respiratory failure | 25 (14.5) | 25 (12.8) | p&#¿;=&#¿;0.509 |
| Non-arrest critical patient | 96 (55.5) | 89 (45.7) | p&#¿;=&#¿;0.059 |
| Location [n (%)] | |||
| Conventional hospitalization | 114 (65.9) | 137 (70.3) | p&#¿;=&#¿;0.37 |
| Peripheral | 59 (34.9) | 58 (29.7) | |
| Activation shift [n (%)] | |||
| Morning (08:00–15:00) | 68 (39.5) | 75 (38.5) | p&#¿;=&#¿;0.83 |
| Afternoon (15:00–22:00) | 50 (29.1) | 56 (28.7) | p&#¿;=&#¿;0.94 |
| Night (22:00–08:00) | 54 (31.4) | 64 (32.8) | p&#¿;=&#¿;0.77 |
| Minutes to team arrival [mean (SD)] | 1.40 (1.17) | 1.7 (3.24) | p&#¿;=&#¿;0.449 |
n (Number of patients), SD (standard deviation), % (percentage).
Bold values are the statistically significant values (p&#¿;<&#¿;0.05).
Team calls were more frequent in males between the sixth and seventh decade of life, with cardiac disease being the most common underlying pathology in both groups (pre-pandemic and pandemic). In all groups, 30%–40% of the patients had been previously bedridden >50% of the time.
The number of activations due to CA was significantly higher in the pandemic group (41.5% vs. 30%, p&#¿;=&#¿;0.02). ARF activations did not differ between the two groups. Daytime activations were more likely to originate from hospital wards during the daytime hours, with no differences between groups. The mean time to arrival of the team at the location originating the call was greater in the pandemic group, though no statistically significant differences were recorded.
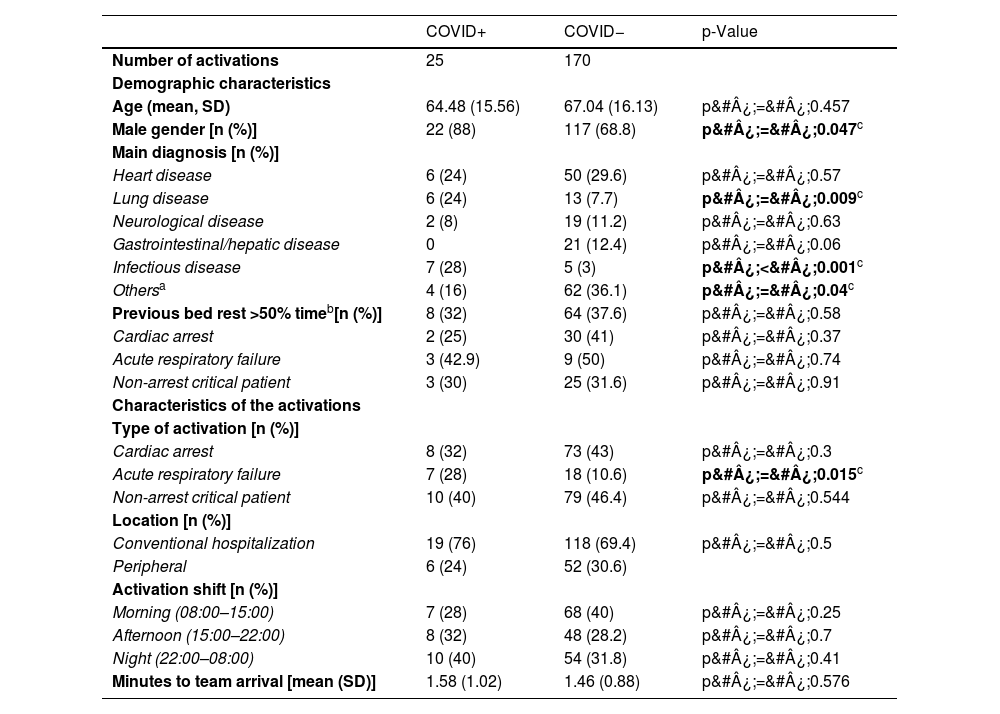
Table 2 shows the demographic and clinical data of the patients and activations included in the pandemic group. Twenty-five patients had documented COVID-19 infection. This group included a higher proportion of males (88% vs. 68.8%, p&#¿;=&#¿;0.047), whose diagnosis upon admission was pulmonary (24% vs. 7.7%, p&#¿;=&#¿;0.009) or infectious disease (28% versus 3%, p&#¿;<&#¿;0.001).
Demographic characteristics of the patients and of the IHCA team activations during the study period, recorded in the sub-analysis of the pandemic group.
| COVID+ | COVID− | p-Value | |
|---|---|---|---|
| Number of activations | 25 | 170 | |
| Demographic characteristics | |||
| Age (mean, SD) | 64.48 (15.56) | 67.04 (16.13) | p&#¿;=&#¿;0.457 |
| Male gender [n (%)] | 22 (88) | 117 (68.8) | p&#¿;=&#¿;0.047c |
| Main diagnosis [n (%)] | |||
| Heart disease | 6 (24) | 50 (29.6) | p&#¿;=&#¿;0.57 |
| Lung disease | 6 (24) | 13 (7.7) | p&#¿;=&#¿;0.009c |
| Neurological disease | 2 (8) | 19 (11.2) | p&#¿;=&#¿;0.63 |
| Gastrointestinal/hepatic disease | 0 | 21 (12.4) | p&#¿;=&#¿;0.06 |
| Infectious disease | 7 (28) | 5 (3) | p&#¿;<&#¿;0.001c |
| Othersa | 4 (16) | 62 (36.1) | p&#¿;=&#¿;0.04c |
| Previous bed rest >50% timeb[n (%)] | 8 (32) | 64 (37.6) | p&#¿;=&#¿;0.58 |
| Cardiac arrest | 2 (25) | 30 (41) | p&#¿;=&#¿;0.37 |
| Acute respiratory failure | 3 (42.9) | 9 (50) | p&#¿;=&#¿;0.74 |
| Non-arrest critical patient | 3 (30) | 25 (31.6) | p&#¿;=&#¿;0.91 |
| Characteristics of the activations | |||
| Type of activation [n (%)] | |||
| Cardiac arrest | 8 (32) | 73 (43) | p&#¿;=&#¿;0.3 |
| Acute respiratory failure | 7 (28) | 18 (10.6) | p&#¿;=&#¿;0.015c |
| Non-arrest critical patient | 10 (40) | 79 (46.4) | p&#¿;=&#¿;0.544 |
| Location [n (%)] | |||
| Conventional hospitalization | 19 (76) | 118 (69.4) | p&#¿;=&#¿;0.5 |
| Peripheral | 6 (24) | 52 (30.6) | |
| Activation shift [n (%)] | |||
| Morning (08:00–15:00) | 7 (28) | 68 (40) | p&#¿;=&#¿;0.25 |
| Afternoon (15:00–22:00) | 8 (32) | 48 (28.2) | p&#¿;=&#¿;0.7 |
| Night (22:00–08:00) | 10 (40) | 54 (31.8) | p&#¿;=&#¿;0.41 |
| Minutes to team arrival [mean (SD)] | 1.58 (1.02) | 1.46 (0.88) | p&#¿;=&#¿;0.576 |
n (number of patients), SD (standard deviation), % (percentage).
Bold values are the statistically significant values (p&#¿;<&#¿;0.05).
The type of activation in both groups (COVID+ and COVID−) was mostly due to critical patients without CA, though there was a statistically significant increase in activations due to ARF in COVID+ patients (28% vs. 10.6%, p&#¿;=&#¿;0.015).
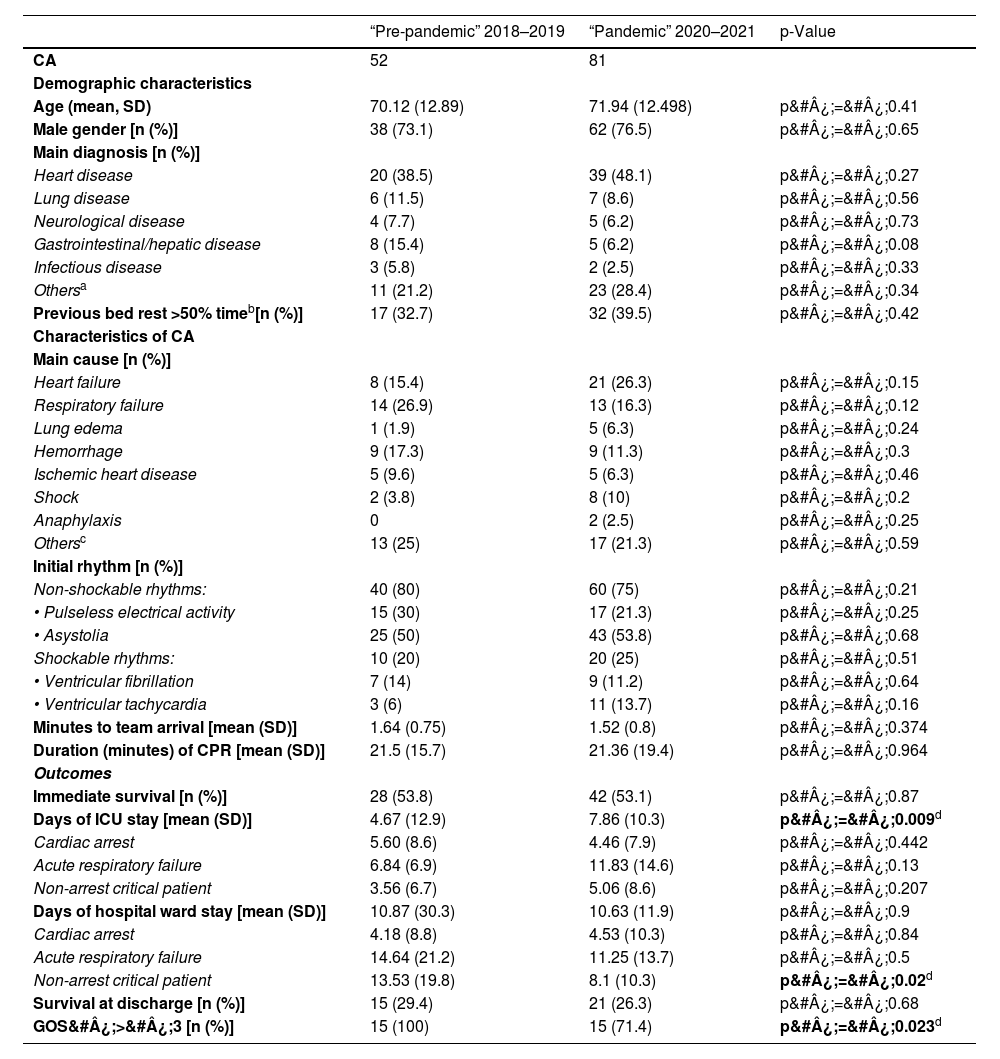
Tables 3 and 4 refer to CA during the study period. Table 3 reflects the demographic and clinical data of the patients, the characteristics of CA, resuscitation and outcomes. Demographically and clinically, there were no differences between the groups in the two periods. There were no differences in the main cause of CA or in the initial rhythm, with a predominance of non-shockable rhythms. None of the groups showed differences in the time of arrival of the team, in the duration of CPR, or in immediate survival or survival at hospital discharge.
Demographic characteristics of the patients, characteristics of the cardiac arrest, the resuscitation maneuvers and patient outcomes during the study period.
| “Pre-pandemic” 2018–2019 | “Pandemic” 2020–2021 | p-Value | |
|---|---|---|---|
| CA | 52 | 81 | |
| Demographic characteristics | |||
| Age (mean, SD) | 70.12 (12.89) | 71.94 (12.498) | p&#¿;=&#¿;0.41 |
| Male gender [n (%)] | 38 (73.1) | 62 (76.5) | p&#¿;=&#¿;0.65 |
| Main diagnosis [n (%)] | |||
| Heart disease | 20 (38.5) | 39 (48.1) | p&#¿;=&#¿;0.27 |
| Lung disease | 6 (11.5) | 7 (8.6) | p&#¿;=&#¿;0.56 |
| Neurological disease | 4 (7.7) | 5 (6.2) | p&#¿;=&#¿;0.73 |
| Gastrointestinal/hepatic disease | 8 (15.4) | 5 (6.2) | p&#¿;=&#¿;0.08 |
| Infectious disease | 3 (5.8) | 2 (2.5) | p&#¿;=&#¿;0.33 |
| Othersa | 11 (21.2) | 23 (28.4) | p&#¿;=&#¿;0.34 |
| Previous bed rest >50% timeb[n (%)] | 17 (32.7) | 32 (39.5) | p&#¿;=&#¿;0.42 |
| Characteristics of CA | |||
| Main cause [n (%)] | |||
| Heart failure | 8 (15.4) | 21 (26.3) | p&#¿;=&#¿;0.15 |
| Respiratory failure | 14 (26.9) | 13 (16.3) | p&#¿;=&#¿;0.12 |
| Lung edema | 1 (1.9) | 5 (6.3) | p&#¿;=&#¿;0.24 |
| Hemorrhage | 9 (17.3) | 9 (11.3) | p&#¿;=&#¿;0.3 |
| Ischemic heart disease | 5 (9.6) | 5 (6.3) | p&#¿;=&#¿;0.46 |
| Shock | 2 (3.8) | 8 (10) | p&#¿;=&#¿;0.2 |
| Anaphylaxis | 0 | 2 (2.5) | p&#¿;=&#¿;0.25 |
| Othersc | 13 (25) | 17 (21.3) | p&#¿;=&#¿;0.59 |
| Initial rhythm [n (%)] | |||
| Non-shockable rhythms: | 40 (80) | 60 (75) | p&#¿;=&#¿;0.21 |
| • Pulseless electrical activity | 15 (30) | 17 (21.3) | p&#¿;=&#¿;0.25 |
| • Asystolia | 25 (50) | 43 (53.8) | p&#¿;=&#¿;0.68 |
| Shockable rhythms: | 10 (20) | 20 (25) | p&#¿;=&#¿;0.51 |
| • Ventricular fibrillation | 7 (14) | 9 (11.2) | p&#¿;=&#¿;0.64 |
| • Ventricular tachycardia | 3 (6) | 11 (13.7) | p&#¿;=&#¿;0.16 |
| Minutes to team arrival [mean (SD)] | 1.64 (0.75) | 1.52 (0.8) | p&#¿;=&#¿;0.374 |
| Duration (minutes) of CPR [mean (SD)] | 21.5 (15.7) | 21.36 (19.4) | p&#¿;=&#¿;0.964 |
| Outcomes | |||
| Immediate survival [n (%)] | 28 (53.8) | 42 (53.1) | p&#¿;=&#¿;0.87 |
| Days of ICU stay [mean (SD)] | 4.67 (12.9) | 7.86 (10.3) | p&#¿;=&#¿;0.009d |
| Cardiac arrest | 5.60 (8.6) | 4.46 (7.9) | p&#¿;=&#¿;0.442 |
| Acute respiratory failure | 6.84 (6.9) | 11.83 (14.6) | p&#¿;=&#¿;0.13 |
| Non-arrest critical patient | 3.56 (6.7) | 5.06 (8.6) | p&#¿;=&#¿;0.207 |
| Days of hospital ward stay [mean (SD)] | 10.87 (30.3) | 10.63 (11.9) | p&#¿;=&#¿;0.9 |
| Cardiac arrest | 4.18 (8.8) | 4.53 (10.3) | p&#¿;=&#¿;0.84 |
| Acute respiratory failure | 14.64 (21.2) | 11.25 (13.7) | p&#¿;=&#¿;0.5 |
| Non-arrest critical patient | 13.53 (19.8) | 8.1 (10.3) | p&#¿;=&#¿;0.02d |
| Survival at discharge [n (%)] | 15 (29.4) | 21 (26.3) | p&#¿;=&#¿;0.68 |
| GOS&#¿;>&#¿;3 [n (%)] | 15 (100) | 15 (71.4) | p&#¿;=&#¿;0.023d |
CA (cardiac arrest), n (number of patients), SD (standard deviation), % (percentage), CPR (cardiopulmonary resuscitation), ICU (Intensive Care Unit), GOS (Glasgow Outcome Scale).
Bold values are the statistically significant values (p&#¿;<&#¿;0.05).
Demographic characteristics of the patients, characteristics of the cardiac arrest, the resuscitation maneuvers and patient outcomes during the pandemic period.
| COVID+ | COVID− | p-Value | |
|---|---|---|---|
| CA | 8 | 73 | |
| Demographic characteristics | |||
| Age (mean, SD) | 71.25 (11.23) | 72.01 (12.7) | p&#¿;=&#¿;0.86 |
| Male gender [n (%)] | 8 (100) | 54 (74) | p&#¿;=&#¿;0.09 |
| Main diagnosis [n (%)] | |||
| Heart disease | 4 (50) | 35 (48) | p&#¿;=&#¿;0.9 |
| Lung disease | 1 (12.5) | 6 (8.2) | p&#¿;=&#¿;0.68 |
| Neurological disease | 0 | 5 (6.8) | p&#¿;=&#¿;0.44 |
| Gastrointestinal/hepatic disease | 0 | 5 (6.8) | p&#¿;=&#¿;0.44 |
| Infectious disease | 1 (12.5) | 1 (1.4) | p&#¿;=&#¿;0.054 |
| Othersa | 2 (25) | 21 (28.8) | p&#¿;=&#¿;0.82 |
| Previous bed rest >50% timeb[n (%)] | 2 (25) | 30 (41.1) | p&#¿;=&#¿;0.37 |
| Characteristics of CA | |||
| Main cause [n (%)] | |||
| Heart failure | 0 (0) | 21 (29.2) | p&#¿;=&#¿;0.07 |
| Respiratory failure | 5 (62.5) | 8 (11.1) | p&#¿;=&#¿;0.0001d |
| Lung edema | 0 (0) | 5 (6.9) | p&#¿;=&#¿;0.44 |
| Hemorrhage | 1 (12.5) | 8 (11.1) | p&#¿;=&#¿;0.89 |
| Ischemic heart disease | 0 (0) | 5 (6.9) | p&#¿;=&#¿;0.44 |
| Shock | 0 (0) | 8 (11.1) | p&#¿;=&#¿;0.89 |
| Anaphylaxis | 0 (0) | 2 (2.9) | p&#¿;=&#¿;0.64 |
| Othersc | 2 (25) | 15 (20.8) | p&#¿;=&#¿;0.78 |
| Initial rhythm [n (%)] | |||
| Non-shockable rhythms: | 7 (87.5) | 53 (74.6) | p&#¿;=&#¿;0.4 |
| • Pulseless electrical activity | 2 (25) | 15 (21.1) | p&#¿;=&#¿;0.8 |
| • Asystolia | 5 (62.5) | 38 (53.5) | p&#¿;=&#¿;0.62 |
| Shockable rhythms: | 1 (12.5) | 18 (25.3) | p&#¿;=&#¿;0.47 |
| • Ventricular fibrillation | 1 (12.5) | 7 (9.9) | p&#¿;=&#¿;0.81 |
| • Ventricular tachycardia | 0 (0) | 11 (15.5) | p&#¿;=&#¿;0.23 |
| Minutes to team arrival [mean (SD)] | 1.87 (1.36) | 1.49 (0.71) | p&#¿;=&#¿;0.19 |
| Duration (minutes) of CPR [mean (SD)] | 17.5 (15.35) | 21.8 (19.9) | p&#¿;=&#¿;0.55 |
| Outcomes | |||
| Immediate survival [n (%)] | 4 (50) | 39 (53.4) | p&#¿;=&#¿;0.85 |
| Days of ICU stay [mean (SD)] | 15.7 (19.3) | 6.57 (7.53) | p&#¿;<&#¿;0.001d |
| Cardiac arrest | 1.33 (0.58) | 9 (9.36) | p&#¿;=&#¿;0.02d |
| Acute respiratory failure | 26 (19.25) | 6.38 (6.55) | p&#¿;=&#¿;0.0007d |
| Non-arrest critical patient | 12.6 (19.5) | 5.2 (6.16) | p&#¿;=&#¿;0.0117d |
| Days of hospital ward stay [mean (SD)] | 7.9 (12.5) | 11.5 (11.86) | p&#¿;=&#¿;0.18 |
| Cardiac arrest | 16 (26) | 9.7 (12.48) | p&#¿;=&#¿;0.23 |
| Acute respiratory failure | 9.4 (8.44) | 15.8 (15.3) | p&#¿;=&#¿;0.3 |
| Non-arrest critical patient | 4 (7.35) | 11.3 (10.66) | p&#¿;=&#¿;0.03d |
| Survival at discharge [n (%)] | 1 (12.5) | 20 (27.4) | p&#¿;=&#¿;0.36 |
| GOS&#¿;>&#¿;3 [n (%)] | 1 (100) | 14 (70) | p&#¿;=&#¿;0.52 |
CA (cardiac arrest), n (number of patients), SD (standard deviation), % (percentage), CPR (cardiopulmonary resuscitation), ICU (Intensive Care Unit), GOS (Glasgow Outcome Scale).
Bold values are the statistically significant values (p&#¿;<&#¿;0.05).
Neurological recovery at discharge was better in the pre-pandemic group compared to the pandemic group (GOS&#¿;>&#¿;3 in 100% of the patients vs. 71.4%, p&#¿;=&#¿;0.023) (Fig. 2).
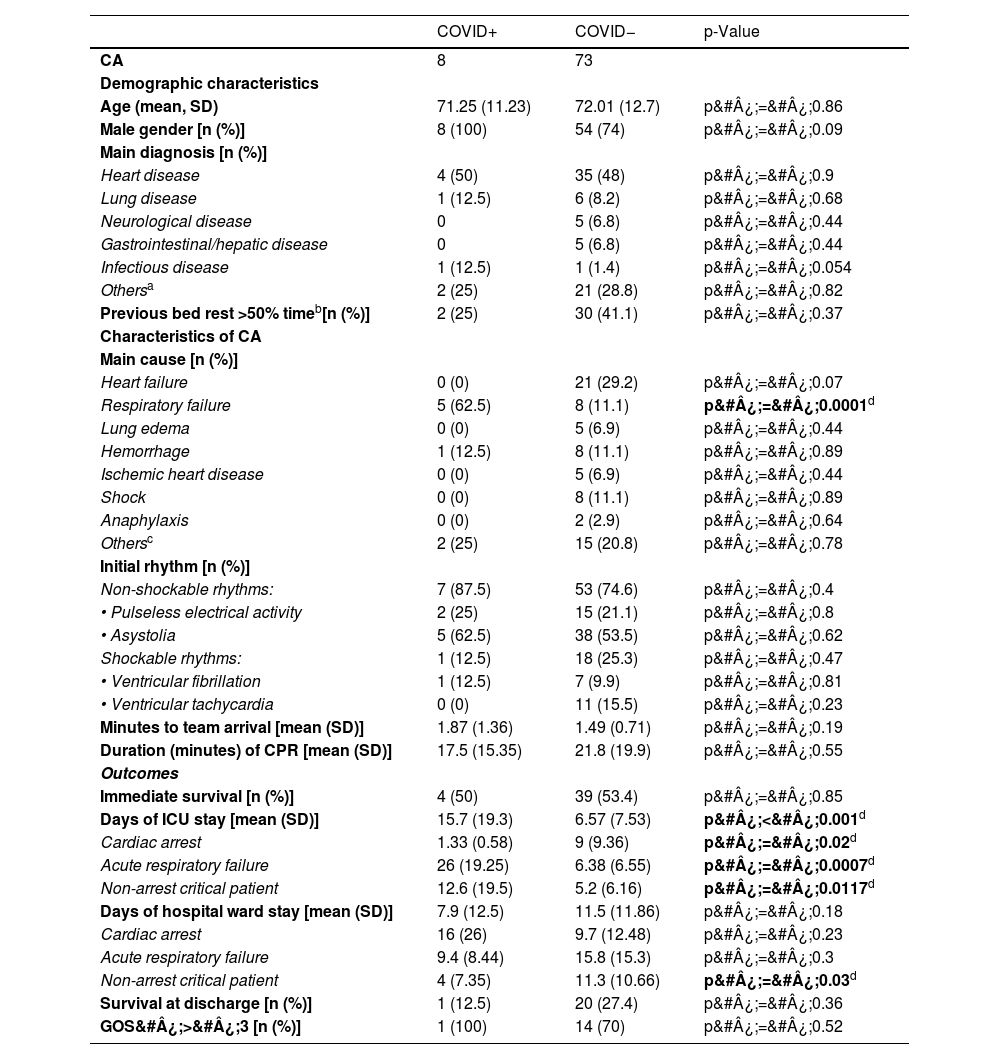
Table 4 shows the characteristics of the patients during the pandemic period, the main characteristics of CA, resuscitation and outcomes. All COVID+ patients with CA were male, and the main underlying disease condition was cardiac, followed by pulmonary and infectious diseases.
ARF was the main cause of CA in the COVID+ group (62.5%). In the COVID- group the causes were more varied, with cardiac causes being the most frequent (29.2%). Non-shockable rhythms were the most frequent conditions in both groups. No significant differences were observed in the arrival times of the team or in immediate survival or survival at hospital discharge. Of the eight COVID+ patients, only one survived at hospital discharge with a GOS&#¿;>&#¿;3, while 14 of the 20 COVID- patients who survived had a GOS&#¿;>&#¿;3.
The ICU length of stay was significantly longer in the pandemic group, with no differences in terms of hospital ward days. A significant increase in ICU stay was observed among COVID+ patients regardless of the reason for ICU admission (CA, ARF or critical patient condition).
DiscussionThe present study provides a snapshot of the activities of the IHCA care team during two very different periods, separated by the declaration of an international viral pandemic in March 2020. The SARS-CoV-2 pandemic was a major challenge for healthcare workers. Aerosol-generating procedures such as orotracheal intubation or cardiopulmonary resuscitation carried a high risk of infection, which could lead to reluctance and delays in initiating the necessary maneuvers.20–22 In response to the health crisis, changes in protocols were implemented to ensure the safety of the professionals, although the IHCA team at our center maintained a high level of activity during the pandemic, showing great commitment and professionalism on the part of all the health care personnel. The increase in activations could be partly attributed to the increase in the number of critical patients in conventional hospital wards, due to the shortage of ICU beds.23,24 It should also be noted that this was a period of extreme care overload, where in addition to the usual patients, the center also had to deal with patients infected with this virus. In addition, patients with other illnesses may have presented to the hospital in a more severe condition due to fear of infection, which may also have contributed to the increase in team activations in this period.
During the pandemic, the number of team activations in COVID+ patients was lower than in COVID− patients. This could be explained by the unfavorable prognosis of patients with advanced COVID-19, leading to an earlier implementation of LTE.25,26 The profile of the patients attended by the team (males between 60–70 years of age with a main diagnosis of heart disease and frequently bedridden >50%) showed no significant differences between the two periods under study. This profile varied somewhat in COVID+ patients, however, with males admitted due to respiratory or infectious causes requiring more frequent attention.
There was also a statistically significant increase in CA in the pandemic period, but paradoxically there were no differences in activations due to ARF, and there was also a nonsignificant decrease in calls to attend critical patients without CA. This may be because, at the beginning of the pandemic, patients were intubated earlier and on a programmed basis to minimize the risk of contagion among the personnel.
The second part of our analysis focuses exclusively on IHCA. The CPR protocols were also modified to prioritize rescuer safety.27 Correct donning of the PPE may have slowed the start of maneuvers, and this could have affected survival.23,24,28,29 Surprisingly, we found no significant differences in arrival or resuscitation times, or in survival rates (initial or at discharge). These findings are in line with the most recent evidence,17 and appear to indicate that the modifications made did not result in significant delays in patient care. This could be explained by the anticipated use of PPE on the part of the healthcare personnel, since it was presumed that any admitted patient could be infected.13,20,25 In addition, pandemic-adapted ALS training and accumulated experience could also have contributed to the early recognition of patients with severe clinical deterioration, increasing activations and improving early care in cases of IHCA.
The literature comparing the characteristics of CA and the patients suffering from it before and during the COVID-19 pandemic is scarce. The individuals most susceptible to CA were males in their seventh decade of life, with underlying cardiac diseases and, in many cases, with previous bed rest >50%.6 This patient profile was maintained in both study periods, even in COVID+ patients.
According to the literature, the most common etiology underlying CA in COVID+ patients was respiratory disease.16,24,29,30 This is consistent with our own study, where among the eight cases of CA in COVID+ patients, respiratory failure was the most common precipitating event. On the other hand, heart failure was the most common cause in the COVID− subgroup, which is also consistent with the reviewed literature. However, future studies could evidence an increase in cardiac etiology, since COVID-19 infection also caused acute cardiac events such as acute coronary syndrome, arrhythmias or heart failure due to the cardiotoxic side effects of certain therapies or due to the prothrombotic effect of the infection itself.21
The most frequent electrocardiographic alterations in both periods were non-shockable rhythms, with a clear predominance among COVID+ patients (87.5%). This coincides with the existing literature and could be due to the hypoxemia associated with ARDS in these patients.29,31
In terms of patient survival, the initial survival rate after CA is usually around 50%, but the survival rate at discharge is much lower (around 20%). In this study, initial survival in the pre-pandemic group was 53.8%, which is similar to that reported in the literature,1,5,8 while in the pandemic period it was 53.1% — which is higher than the 30.5% reported in a meta-analysis conducted by Szarpak et al.31. This difference could be due to the efficiency and organization of the IHCA team during the pandemic, which did not show significant delays in arrival or maneuvering times. Survival at discharge, although also similar to that reported in the literature in both groups, was slightly lower among the COVID+ patients (12.5%). In the studies published by Acharya et al., Hayek et al. and Sheth et al., survival at discharge was even lower (6.8%, 0% and 0.7%, respectively),24–26 which could be attributed to the greater severity of the patients included in their series (patients admitted to the ICU) and to the collapse and lack of healthcare resources in the United States during this period.
Regarding the neurological prognosis, a significantly better neurological outcome (GOS&#¿;>&#¿;3) was observed in the pre-pandemic period. Although it might be expected that COVID+ patients would have a better neurological recovery, since respiratory illness was the most common precipitating cause, the literature describes the opposite, with a poorer neurological prognosis in these patients after CA. Prolonged hypoxia, systemic effects and the sequelae of the virus itself could be behind this poor prognosis.16,30,32,33 In the present study, only one COVID+ patient survived at discharge after CA, which limits the interpretation of these observations. A larger sample may provide more conclusive results.
Although no significant differences in survival rates or neurological outcomes after CA were observed between infected and non-infected individuals, the ICU stay of COVID+ patients who suffered CA was considerably shorter than in the case of COVID− patients, which could be related to the higher mortality among the former. In contrast, COVID+ patients had longer overall hospital stays, particularly in the ICU, due to a more complex recovery process and the sequelae and complications they presented (myopathy, greater need for supplementary oxygen therapy, etc.).
Our study is not without limitations. Its retrospective, single-center design with a small sample size, particularly in the COVID+ subgroup, makes it difficult to generalize the results. In addition, the rapid progression of disease due to COVID-19 resulted in greater severity and futile treatments, with the use of LTE and symptomatic/palliative treatment measures. These patients were therefore excluded from the IHCA team activations, which may have biased the overall results of the COVID+ patients. Lastly, the previous baseline status of the patients was not accurately assessed, nor were comorbidity severity indices such as the Acute Physiology and Chronic Health Evaluation II (APACHE II) used, which prevented us from ensuring homogeneity of baseline patient characteristics. To obtain more robust and generalizable results, multicenter and long-term studies with larger samples would be needed.
Nearly 5 years after the onset of the public health crisis caused by the COVID-19 pandemic, the results of the present study underscore the importance of continuously adapting and improving protocols and training personnel in the recognition and dynamic management of medical emergencies. Although SARS-CoV-2 is now a less lethal virus, we cannot rule out new epidemics or pandemics that may affect the way we care for patients. Studying what happened, through systematic data collection is important to increase our knowledge, improve our response capacity, and optimize care for possible future health crises.
CRediT authorship contribution statementGhali Ballout: statistical analysis and drafting of the manuscript. Introduction of changes.
Marta Magaldi-Mendaña: drafting of the manuscript. Introduction and correction of changes.
Bartomeu Ramis-Pou: data acquisition and statistical analysis.
Cristian Torres-Quevedo: data acquisition.
Adriana Capdevila-Freixas: data acquisition.
Silvia Moreno-Jurico: data acquisition.
Enrique Jesús Carrero-Cardenal: study conception and REC, final supervision of the manuscript.
Jaime Fontanals-Dotras: study conception and REC, final supervision of the manuscript.
Cardiac Arrest Commission (Comisión a la Atención a la Parada Cardiorespiratoria) of Hospital Clínic de Barcelona (Spain): assessment of the entire in-hospital cardiac arrest care circuit, analysis of results.
FundingThe present study has received no funding from public or private agencies, research entities or foundations.
Jaime Fontanals, Marta Magaldi, Carlos Ferrando, María Teresa Peix, Mercè Agustí, Eva Sánchez, Sara Fernández, Ana Sandra Hernández, Gerard Sánchez-Etayo, Susana Millán, Pedro Castro, Teresa López
Affiliation: Hospital Clínic of Barcelona.