The clinical care of hospitalized seriously ill patients must be suitably proportionate independently of the functional unit to which they have been admitted. Most of these patients are admitted to the Intensive Care Unit (ICU), where uninterrupted management is provided, with important technological and care resources. However, hospitalization of the seriously ill patient must be understood as a continuum starting and ending beyond hospital stay. Anticipating critical worsening requiring admission to the ICU would be of benefit to the patient, avoiding greater clinical worsening, and also would be of benefit to the hospital, by allowing improved resource management.
Intensivists are the professionals best suited for this purpose, since they are trained to recognize the seriousness of an always dynamic clinical situation. Addressing this task implies a change in the traditional way of working of the ICU, since a critical patient is not only a patient already admitted to the Unit but also any other patient admitted to hospital whose clinical situation is becoming destabilized. In this context, our ICU has established two strategic lines. One consists of the identification of patients at risk outside the Unit and is based on the recognition, diagnostic orientation and early treatment of the seriously ill patient, in collaboration with other clinical specialties and independently of the hospital area to which the patient has been admitted. The second line in turn comprises clinical care within the actual Unit, and is based on the promotion of safety and the vigilance of nosocomial infections.
Los cuidados clínicos del paciente gravemente enfermo hospitalizado deben ser adecuadamente proporcionados independientemente de la unidad funcional en la que esté ingresado. La mayoría de estos enfermos se encuentran ingresados en la Unidad de Cuidados Intensivos (UCI), donde se aseguran sus cuidados de forma ininterrumpida, con un elevado nivel tecnológico y asistencial. Sin embargo, la hospitalización del enfermo grave debe ser entendida como un continuo, que empieza y termina más allá de ella. Anticiparse al empeoramiento crítico que obligue al ingreso en la UCI supondría un beneficio para el enfermo, evitando un mayor empeoramiento clínico, y un beneficio para la institución hospitalaria, permitiendo gestionar mejor sus recursos.
El médico intensivista es el más adecuado para este propósito, al estar entrenado en el reconocimiento de la gravedad de una situación clínica siempre dinámica. Y desempeñar esta labor significa un cambio en la forma de trabajo tradicional de la UCI, porque el enfermo crítico ya no es solo aquel ingresado en la Unidad sino cualquier enfermo ingresado en el hospital cuya condición clínica se esté inestabilizando. En este contexto, nuestra UCI ha establecido dos líneas estratégicas. La primera consiste en la identificación de los pacientes de riesgo fuera de la Unidad y está basada en el reconocimiento, orientación diagnóstica y tratamiento temprano del paciente grave, en colaboración con otras especialidades clínicas e independientemente de su lugar de hospitalización. La segunda consiste en la atención clínica dentro de la propia Unidad y está basada en el fomento de la cultura de seguridad y la vigilancia de la infección nosocomial.
The clinical care of the hospitalized seriously ill patient must be ensured by the healthcare institution throughout the clinical evolution of the individual, from hospital admission to discharge home. When the presenting clinical condition is sufficiently serious, such care starts in the Emergency Area, and immediately thereafter continues in the Intensive Care Unit (ICU). Following clinical improvement, the patient is moved to a conventional hospital ward, where he or she remains until hospital discharge, provided the clinical course is favorable. However, if the clinical condition worsens while in the ward, the patient may have to be readmitted to the ICU. However, in other cases the presenting clinical condition of the patient is not serious enough to warrant direct admission to the ICU, and after a more or less brief period of initial clinical stabilization, the patient is moved to a conventional hospital ward. Here again, if the clinical condition subsequently worsens, admission to the ICU (in this case for the first time) may prove necessary.
However, what would happen if we could identify patients at risk, before critical worsening occurs, when the subject is still in the Emergency Area or in the conventional hospital ward? Undoubtedly, anticipative clinical care in these patients at risk could have a positive impact upon the clinical course and prognosis of the illness. In effect, if the identified clinical condition was serious enough, necessary admission to the ICU could be decided earlier – thereby avoiding unnecessary delays in treatment. Furthermore, and perhaps even more importantly, if the clinical condition of the patient were to warrant a diagnostic reorientation or intensification of the therapeutic measures, it might be possible to achieve clinical improvement allowing us to avoid admission to the ICU–with the added advantage of better management of the available healthcare resources. Thus, the care of the seriously ill patient, while centered on the ICU, can be extended beyond the latter, representing a continuous process throughout the hospital stay of the patient.
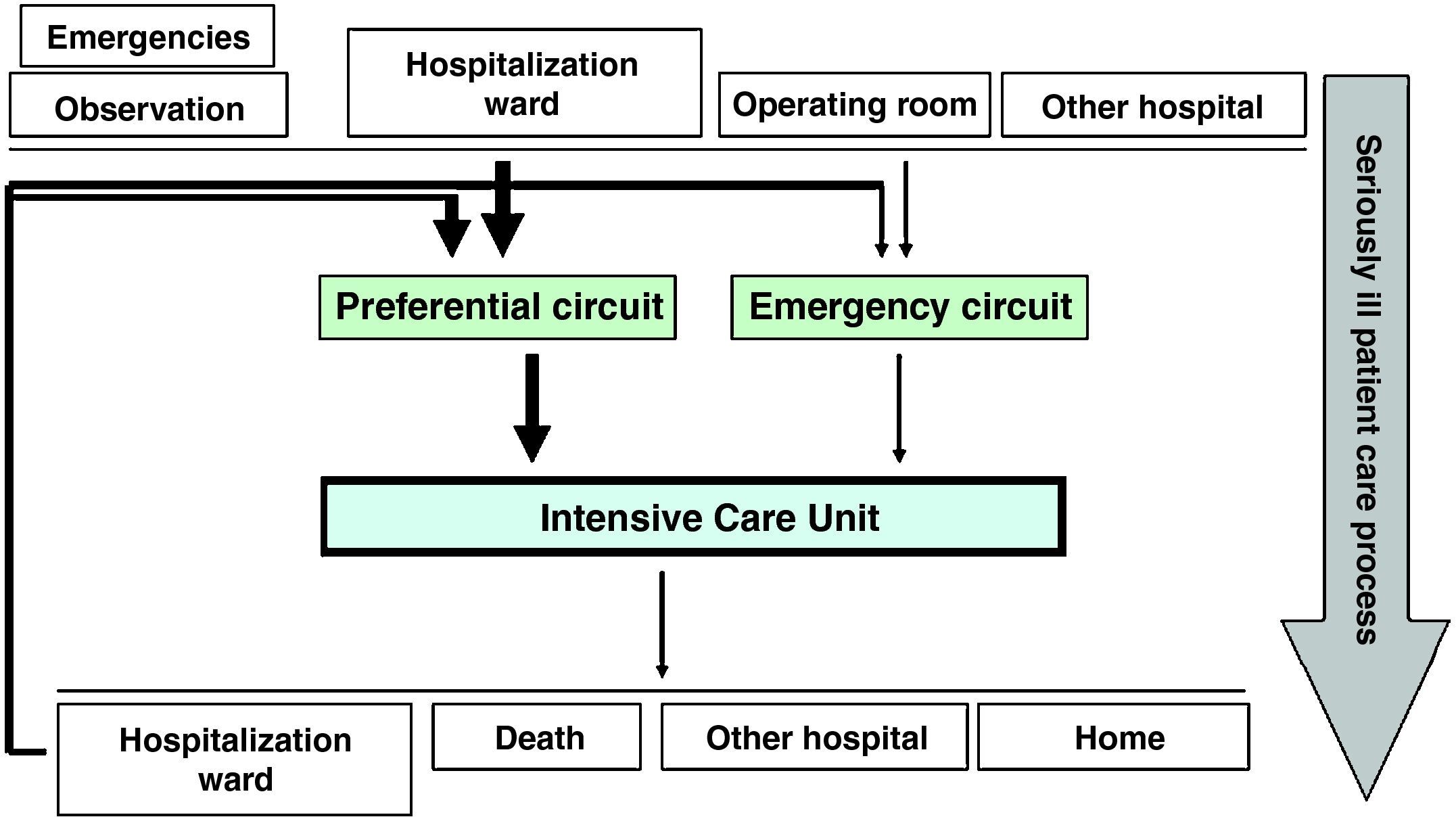
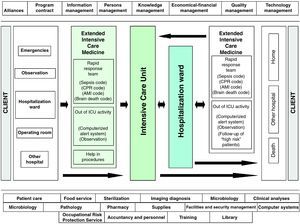
Stated in other words, if we were to define patient flow in the ICU, we would see that admission to the latter is either programmed or emergency based. Programmed admissions to the ICU normally correspond to high-risk postoperative patients, while the emergency cases can come from the Emergency and Observation Area, from a conventional hospitalization ward, or from some other hospital center. In turn, practically all patients admitted to the ICU are subsequently moved to a hospitalization ward (Fig. 1). The patient flow can vary in magnitude from one center to another, though globalizing the care process of the seriously ill patient could allow us to attempt to modify the flow in itself. Specifically, if we emphasize activity aimed at ensuring the early detection of seriously ill cases, we could transform emergency and possibly late patient inflow, attended by medical personnel on duty, into programmed and early management, with better distribution among the personnel members of the Unit. All this in turn would be valid in the settings of both the Emergency and Observation Area and the different conventional hospitalization wards.
The above idea gains importance with our awareness that delays in treatment, or the provision of inadequate care in the hospitalization ward, independently of the cause, often result in non-anticipated emergency admissions to the ICU, and imply longer hospital stay and even greater mortality,1–particularly in diseases regarded as being “time-dependent”, where delays in starting treatment can lead to a marked increase in patient morbidity–mortality. This circumstance has been documented in the literature for quite some time.2 Indeed, it has been estimated that up to 50% of all hospitalized patients do not receive adequate treatment before their admission to the ICU, and that on the other hand a full 40% of admissions to the ICU could be avoided.3 Furthermore, patients admitted to the ICU from a conventional hospital ward may suffer greater mortality than those directly admitted to the ICU from the Emergency Area.4,5 However, the early identification of these patients at risk is not always easy in a conventional hospital ward. This is due to a number of reasons, including a possible lack of sufficient human or material resources, inadequate organization of the functional area, insufficient personnel training, a lack of supervision of the activities carried out, underestimation of the clinical condition of the patient, late identification of the alarms signs and symptoms, a delay in the diagnostic or treatment decision-taking process, or delays in requesting necessary clinical counseling. In any case, and as an example, almost 80% of all patients suffering cardiorespiratory arrest in hospital manifest physiopathological alterations in the previous 6–24h, in the form of undetected or unnoticed changes in blood pressure, heart or breathing rate, oxygenation, diuresis or level of consciousness.6–9
Intensivists, thanks to their professional capacitation and daily clinical activities, are undoubtedly the hospital professionals with the best training not only for the early identification of serious illness with an integral vision of the patient, but also for establishing therapeutic priorities and taking quick clinical decisions. In recent years, this has led to the development of medical care teams with different integrating members and different particularities in different centers and countries–though almost always dependent upon an intensivist, and with the same purpose in mind: the early identification of risk patients outside the ICU.10–12 In fact, in the United States these teams form part of the “five million lives” program of the Institute for Healthcare Improvement, as one of the evidence-based interventions designed to improve patient prognosis and reduce the number of unnecessary deaths.13 Although the individual results vary,14–16 the benefits afforded by such teams appear clear–particularly as regards reduction in the risk of cardiorespiratory arrest (RR: 0.66; 95%CI: 0.54–0.80)17–and they have already been incorporated to the clinical guides on cardiopulmonary resuscitation.18 However, and explained in part by differences in the composition of these medical teams, their different intervention methods or different evaluated objectives, the benefits derived in terms of lessened mortality remain to be adequately defined (RR: 0.96; 95%CI: 0.84–1.09).17,19,20
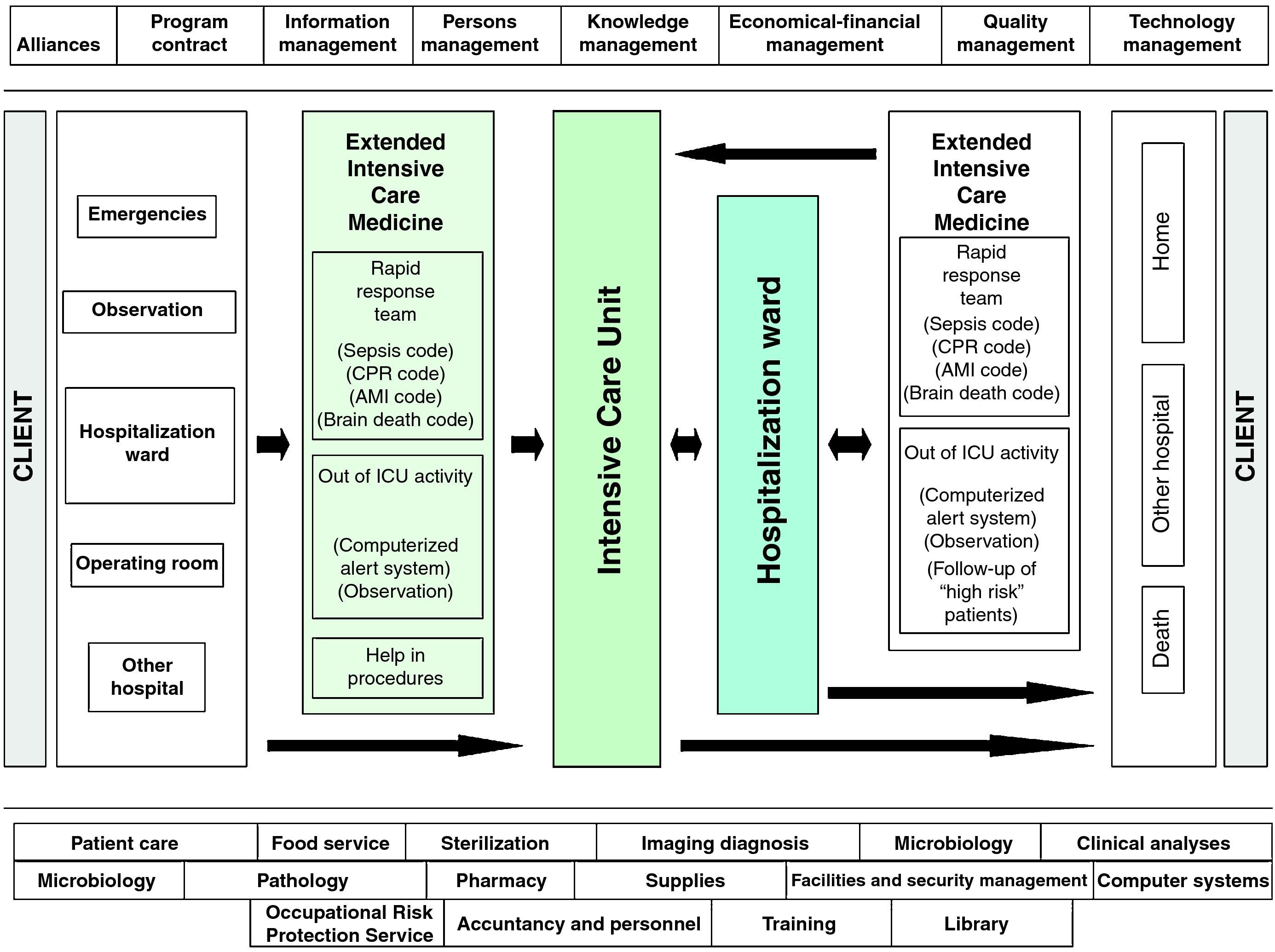
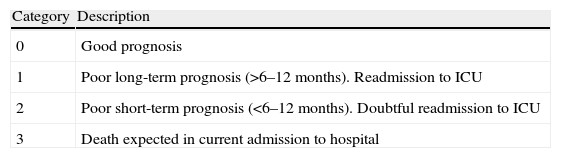
With these premises, our Unit has developed a management system in Intensive Care Medicine, based on the safety of the seriously ill patient during the entire hospitalization process, and which we refer to as an Extended Intensive Care Service (EICS) (Fig. 2). Specifically, we have established two well differentiated strategic lines, according to the place of hospitalization of the patient: “Early detection of the seriously ill patient outside the ICU” and “Patient safety in the ICU”. The first of these strategic lines refers to the identification of patients at risk outside the ICU, based on the identification, diagnostic orientation and early treatment of the seriously ill patient, in collaboration with other clinical specialties and independently of the actual place or hospitalization involved. Thus, either when the patient meets a series of well defined severity criteria and the supervising physician or nurse alerts the EICS team, or when the EICS team in the course of its daily programmed activities directly identifies a patient at risk, the required level of medical care is assessed, and decisions are taken regarding the best location for such care–always in coordination with the supervising physician. Such activity focuses on patients still in the Emergency and Observation Area, patients admitted to a conventional hospitalization ward, and patients admitted to such wards after discharge from the ICU but who are considered to be at high risk (postsurgical cases with concomitant medical disorders, patients with evolving organ failure, patients still strongly dependent upon nursing care, early discharges forced by healthcare necessities, etc.). A tool of help in the required follow-up of a concrete patient, and which moreover serves as quality control, is the so-called Sabadell index.21 This instrument, recently validated in a Spanish national multicenter study,22 is a subjective scale that grades the patient prognosis at discharge from the ICU in terms of survival of the hospital episode (Table 1).
The Sabadell index.
| Category | Description |
| 0 | Good prognosis |
| 1 | Poor long-term prognosis (>6–12 months). Readmission to ICU |
| 2 | Poor short-term prognosis (<6–12 months). Doubtful readmission to ICU |
| 3 | Death expected in current admission to hospital |
The second strategic line logically refers to clinical care in the actual ICU, and is based on two aspects: (a) the promotion of safety and the adoption of a dynamic related incidents communicating system allowing the rapid adoption of corrective actions; and (b) the vigilance of nosocomial infections specifically and directly related to known risk factors and/or associated to increased morbidity–mortality among critical patients: mechanical ventilation-associated pneumonia, urethral catheter-related urinary infections, primary bacteremias and bacteremias related to catheters and secondary bacteremia. This distinction is necessary, since Departments of Intensive Care Medicine are hospital units with an added potential risk for the patient, due to the inherent seriousness of the clinical condition of such cases, the sometimes simultaneous undertaking of multiple activities, invasive diagnostic and treatment procedures, and the ever increasing sophistication and complexity of the care provided. Indeed, it has been estimated that the risk of suffering an incident without damage as a mere consequence of having been admitted to the ICU is 73%, and that the risk of suffering an adverse event is 40%.23 In turn, the estimated probability of suffering at least one safety-related incident (including nosocomial infection) is almost 62%,23 while the risk of experiencing an adverse event in the ICU increases between 8 and 26% for each added day of stay in the Unit.24,25 The national and international literature regularly points to medication-related problems as the most common incidents, representing almost a quarter of all cases. Other frequent incidents in turn are related to medical apparatuses or equipment, the care received, the use of vascular accesses and catheters, and problems related to the artificial airway and mechanical ventilation. Although more serious, incidents related to nosocomial infections are less frequent (8%).23
DevelopmentEarly detection of the seriously Ill patient outside the Intensive Care UnitThe system is based on active search and follow-up of the patient at risk–regardless of whether no admission to the ICU has been required, or whether the patient have already been discharged from the ICU–and on the development of Early Warning Systems (EWS) allowing the physician supervising the patient to decide early activation of the EICS.
Intervention referred to the first strategic line commented above (“Activity outside the ICU”) is fundamental on three basic points: the elaboration of a hospital laboratory test alert system; the daily evaluation of patients in certain hospitalization areas; and the follow-up of those patients considered to be at high risk and who have already been discharged from the ICU. Specifically, an electronic database is updated daily first thing in the morning, registering laboratory test data considered to be determinant for our intervention, and which have been collected from the previous day up until that morning. Once a certain threshold value has been exceeded (troponin I>0.3μg/l, pH<7.30, PCO2>50 mmHg, platelet count<100,000/μl, lactate>3mmol/l), the specific information is identified, including sampling time and value of the parameter, with correlation to the identity of the patient (full name and case history number). Then, on a daily and successive basis, one of the intensivists checks each of the patients alerted through the electronic case history (Selene®), and decides whether intervention is needed or not. If intervention proves necessary, the intensivist contacts the physician in charge of the patient, and both jointly evaluate the clinical situation to decide the course to be taken. The possibilities therefore comprise help in treatment adjustment or diagnostic approach, with close patient follow-up over the subsequent hours; early admission to the ICU, supervising transfer and admission to the Unit; or participation in the decision to limit life support management measures. Independently of the number of patients alerted through the electronic system and of where these patients are located, daily evaluation is also made with the same purpose of those patients admitted to the Emergency and Observation Area, in coordination with the supervising physician. In a similar manner, daily clinical evaluation is made of those patients who have already been discharged from the ICU and which are considered to be at high risk. These subjects, with Sabadell index scores of 1 or 2, are those who have been in the Unit for a long time (>10 days), still require too much nursing care, have been discharged with a tracheotomy, or–for example–have been hospitalized in a surgical ward and at discharge are still receiving treatment for infectious complications. At the end of the morning, during the clinical session of the Unit, the activities carried out are commented, informing of the clinical situation of the evaluated patients, the expected outcomes, and whether admission to Intensive Care was decided.
Regarding such admission, and determined by the type of disease predominantly dealt with in our Unit and by the need to ensure earlier intervention with a view to improving the patient prognosis, we have defined certain disease processes as being of priority concern. A specific multidisciplinary intervention plan has been implemented, and in some cases an Early Warning System (EWS) with certain clinical-laboratory test severity criteria, in order to optimize clinical care. An example is provided by the intervention plan in the case of acute coronary syndrome (“Ischemic heart disease code”), which was presented and approved by the Medical Management Board of the center. Likewise, a plan has been developed referring to in-hospital emergency care and cardiopulmonary resuscitation (“CPR code”), which establishes, maintains and informs of the communication system guaranteeing immediate activation of the intervention protocol in the event of any hospital medical emergency.
The “Sepsis code” in turn aims to ensure the early identification of septic patients, in accordance with the guidelines of the Surviving Sepsis Campaign.26,27 Following the pertinent informative sessions, the distribution of supporting graphic material and diffusion of the guide, the communication system in response to initial signs of alert has been established for both early treatment and activation of the EICS. Lastly, the next step, which is still under development, will be the introduction of an intervention protocol for the identification of patients with serious brain damage and the early reporting of such cases to the EICS and to the organ transplant coordinator of the center, in order to facilitate posterior decision taking (“Brain death code”)–as advised by the Spanish National Transplant Organization.28
Patient safety in the ICUIn order to guarantee safe care of the patients admitted to the ICU, a specific functional group has been created, representing each of the implicated professional areas. In general terms, its main tasks are to provide and promote an adequate environment referring to patient safety, document and analyze critical incidents, inform of the corrective measures taken, and supervise follow-up and adherence to the adopted measures. The registry of incidents comprises several data collection systems. On one hand we have a specific sheet which is voluntarily placed in the corresponding booth for posterior analysis, and which is accessible at all times, and on the other hand we have the data checklist corresponding to the information collected daily at several points during the day: on occasion of the change in nursing shift in the morning and at night, and in the clinical check conducted at midday–with participation of all the personnel in the Unit related to the patient, commenting the planned treatment and reflecting the clinical data on-screen (laboratory tests, radiological explorations, etc.), as well as the current treatment being provided.
Special attention focuses on the vigilance of nosocomial infections specifically and directly related to known risk factors and/or associated to increased morbidity–mortality among critical patients: mechanical ventilation-associated pneumonia, urethral catheter-related urinary infections, primary bacteremias and bacteremias related to catheters and secondary bacteremia. In this context we follow the corresponding national and international recommendations and guidelines, with use of the common methodology of the ENVIN-HELICS study,29 which allows us to compare and present results in both the local and national setting. A specific detail to be taken into account here is the common use in our Unit of selective digestive decontamination (SDD), based on a continuous floral vigilance system, with preventive isolation of those patients presenting hospital stays of over 5 days before admission to the ICU, with recent needs for healthcare, or with antecedents of colonization by some multiresistant microorganism.
ConclusionsThe approach adopted by this organizational model of the activities of the Intensive Care Unit has several connotations. A first and simple concern is to actively ensure the care of those patients admitted to the ICU properly in an efficient, effective and safe manner. This is easily generalizable, requiring the modifications logically related to the individual characteristics of each center and Unit. It is also necessary, and to one degree or other, and in a more or less systematized manner, has always been present in our professional activity.
A second and not always easily generalizable concern is the change in the traditional functional model of the ICU at both organizational and conceptual levels. In effect, the patient is no longer seen as only the individual admitted to the Unit, but now moreover also includes those individuals whose clinical condition can worsen, regardless of where they are hospitalized, because early clinical care in such cases can benefit the ulterior patient course. Benefit in this case is not limited to the patient, since modifying patient flow from the emergency circuit to the preferential care circuit makes it possible to lessen the burden upon the former–supervised only by professionals on duty. More precise knowledge of the clinical situation of these evaluated patients therefore allows for improved management of the existing resources. Lastly in our experience, working closer to the rest of the clinical specialties has served to improve knowledge of our daily work as intensivists, affording greater professional recognition and, undoubtedly, a greater institutional influence on the part of our Unit within the hospital.
Conflict of interestThe authors have no conflict of interest to declare.
Please cite this article as: Calvo Herranz E, et al. Implantación de un sistema de gestión en Medicina Intensiva basado en la seguridad del paciente gravemente enfermo durante todo el proceso de hospitalización: servicio extendido de Medicina Intensiva. Med Intensiva. 2011;35:354–60.