To determine whether the implementation of a protocol for the management of patients with acute pancreatitis (AP) in an Intensive Care Unit (ICU) improves the clinical outcomes.
DesignA retrospective, before-after observational case series study was carried out.
Study period1 January 2001 to 31 December 2016, divided in 2 periods (pre-protocol 2001–2007, post-protocol 2008–2016).
ScopeAn ICU with 48 beds and a recruitment population of 700,000 inhabitants.
ParticipantsAP patients admitted to the ICU, with no exclusion criteria.
InterventionsThe recommendations proposed in the 7th Consensus Conference of the SEMICYUC on AP (5 September 2007) were applied in the second period.
Main variables of interestPatient age, sex, APACHE II, SOFA, study period, pre-ICU hospital stay, nutrition, surgery, antibiotic prophylaxis, hospital mortality, ICU length of stay, hospital length of stay, determinant-based classification.
ResultsThe study comprised 286 patients (94 in the pre-protocol period, 192 in the post-protocol period), with a global in-hospital mortality rate of 23.1% (n=66). Application of the protocol decreased the pre-ICU hospital stay and the use of antibiotic prophylaxis, and increased the use of enteral nutrition. Hospital mortality decreased in the second period (35.1 vs. 17.18%; P=.001), with no significant changes in ICU and hospital stays. In the multivariate logistic regression analysis, the variable period of treatment remained as a variable of statistical significance in terms of hospital mortality (OR 0.34 for the period 2008–2016, 95% CI 0.15–0.74).
ConclusionsThe implementation of a protocol could result in decreased mortality among AP patients admitted to the ICU.
Conocer si la implantación de un protocolo para el manejo de la pancreatitis aguda (PA) en Medicina Intensiva (MI) redundó en la mejora de los resultados clínicos.
DiseñoSerie de casos, observacional, retrospectivo, con un diseño antes-después.
Periodo de estudio1/01/2001-31/12/2016, dividido en 2 periodos (preprotocolo 2001-2007; posprotocolo 2008-2016).
ÁmbitoUn servicio de MI con 48 camas y población de 700.000 habitantes.
ParticipantesPacientes ingresados en MI con PA. No hubo criterios de exclusión.
IntervencionesSe aplicaron las recomendaciones propuestas en la 7.a Conferencia de Consenso (2007) de la SEMICYUC sobre la PA en el segundo periodo.
Variables de interés principalesEdad, sexo, APACHE II, SOFA, periodo a estudio, días previos al ingreso en MI, tipo de nutrición, cirugía, profilaxis antibiótica, mortalidad hospitalaria, estancia en MI, estancia hospitalaria, clasificación basada en determinantes.
ResultadosDoscientos ochenta y seis pacientes (94 preprotocolo, 192 posprotocolo), mortalidad hospitalaria de 66 casos (23,1%). La aplicación del protocolo supuso una disminución de la estancia hospitalaria previa al ingreso en MI, y de la profilaxis antibiótica, con un aumento del uso de nutrición enteral. Se evidenció un descenso de la mortalidad hospitalaria en el segundo periodo (35,1 vs. 17,18%, p=0,001), sin cambios significativos en la estancia en MI ni en la hospitalaria. En el análisis multivariante, la variable «periodo de tratamiento» mantuvo significación estadística respecto a la mortalidad hospitalaria (OR 0,34 en 2008-2016, IC 95% 0,15-0,74).
ConclusionesEl establecimiento de un protocolo podría estar relacionado con un descenso de la mortalidad de los pacientes ingresados en MI por PA.
Acute pancreatitis (AP) is a potentially serious disease whose incidence has been growing1 to up to 50 and 80 cases for every 100,000 inhabitants-year in the United States. This is why pancreatic disease is considered a common disease in children and adults alike.2 Over half the cases in adults are associated with biliary disease and alcoholism. Its clinical course is variable and 80% of its forms of presentation are mild.3,4 However, the most serious cases can lead to mortality rates of up to 25–45% regardless of what the cause may be.5
Mortality has 2 peaks here: one early peak due to systemic inflammatory response syndrome (SIRS) that is severe compared to the development of pancreatic necrosis and multi organ failure, and a late peak due to infected pancreatic necrosis and/or sepsis.6,7 Being able to recognize early those patients with multi organ failure is essential to be able to guide resuscitation and start intensive treatment in an intensive care unit (ICU), thereby reducing morbimortality.8 As a matter of fact, an early stratification of the severity of the disease improves clinical results and reduces significantly the length of hospital stays.9
Back in 2007 SEMICYUC held the VII Consensus Conference on AP and established a series of recommendations for the comprehensive management of the disease. A few years later, in 2012, these recommendations10 were modified and the following changes were included:
- -
Early stratification of the severe forms of the disease with strict clinical and analytical follow-up during the first 48–96h, and early ICU admission.
- -
Initiation of early artificial feeding (within the first 72h) always using, if possible, enteral feeding through nasogastric probes, whether nasojejunal or transpyloric.11
- -
The use of prophylactic antibiotic therapy is not recommended.
- -
Indicate surgical treatment basically for the management of infected pancreatic necrosis or abscess and delay the surgery for another 21 days to see what the clinical course of the disease is.12
This study tries to verify if the implementation of a protocol based on this Consensus Conference organized by SEMICYUC had an impact on the clinical progression of patients with AP admitted to ICUs. Therefore, we conducted one 16-year retrospective study before and after the implementation of a protocol based on these recommendations.
The primary endpoint of this study is to know whether the recommendations proposed at the VII Consensus Conference organized by SEMICYUC on the Management of Acute Pancreatitis in Intensive Medicine (05-09-07) had an impact on mortality, length of intra-ICU stays, and length of hospital stays in patients admitted to a critical care service due to AP; the study secondary endpoint was to evaluate whether such recommendations had an impact on the management of these patients when it comes to early ICU admissions, use of early enteral feeding, non administration of empirical antibiotic therapy, and, if possible, delay surgery for another 21 days to see what the clinical course of the disease is.
Patients and methodsPrimary endpoints: show whether the recommendations suggested at the VII Consensus Conference organized by SEMICYUC on the Management of Acute Pancreatitis in Intensive Medicine (05-09-07) had an impact on mortality, the length of ICU stays, and the length of hospital stays.
Secondary endpoints: assess whether the recommendations proposed at the VII Consensus Conference organized by SEMICYUC on the Management of Acute Pancreatitis in Intensive Medicine (05-09-07) changed the management of these patients.
Study design: observational, retrospective study designed before and after the VII Consensus Conference organized by SEMICYUC on the Management of Acute Pancreatitis in Intensive Medicine (05-09-07).
Population studied and reference setting: all patients admitted to the critical care service of Hospital Donostia due to AP were included consecutively and without any exclusion criteria. This critical care unit has 48 bed available and provides healthcare to a population of over 700000 people.
Study periods: the study period was divided into two (2) periods. The first period from January 1, 2001 to December 31, 2016 and prior to the SEMICYUC Consensus Conference (between 2001 and 2007), and the second one after the SEMICYUC Consensus Conference between 2008 and 2016.
Variables: the following variables were collected in this study: affiliation variables (number of patients, age, sex); study period (pre-consensus conference or post-consensus conference); time of hospital admission (days of hospital admission-ICU admission, days of ICU stay, days of hospital stay); etiology that triggered the clinical signs (biliary, alcoholic, idiopathic, post-ERCP, other); degree of ultrasound-guided severity using the Balthasar score; severity scores including the SOFA and APACHE II scores within the first 24h and Ranson's score; need for mechanical ventilation support (MVS) and continuous renal replacement therapy (CRRT); maximum intra-abdominal pressure (IAP) achieved during the ICU stay; feeding technique used in the patient within the first 48h following admission (none, enteral, parenteral or mixed feeding); local complications developed by the patient during his hospital stay (infected necrosis, intra-abdominal hemorrhage, perforated hollow viscus), need for surgery; mortality and if mortality occurred why (early SIRS, pancreatic infection, nosocomial extrapancreatic infection, other); development of pancreatic sepsis; development of extrapancreatic sepsis; use of empirical antibiotic therapy at admission, and severity measured using the determinant-based classification.6
Definitions used in this study- -
Days of hospital admission-ICU admission: days elapsed ever since the patient was admitted to the hospital until he was admitted to the intensive care unit.
- -
Period of treatment protocol: 2 different periods were established, pre- (2001–2007) and post- (2007–2016) consensus conference.
- -
Etiology:
- •
Alcoholic: excessive consumption of alcohol (>60g/day) sustained for over 5 years with no other defined cause for pancreatitis.
- •
Biliary: presence of stones in the biliary duct with no other defined cause for pancreatitis.
- •
Post-endoscopic retrograde cholangiopancreatography: pancreatitis that kicked in 7 days after performing one endoscopic retrograde cholangiopancreatography.
- •
Other: other causes for pancreatitis including post-traumatic pancreatitis, postoperative pancreatitis, and hypertriglyceridemia-induced AP, apart from other less common causes.
- •
Idiopathic: whenever the criteria for the remaining etiologies are not met.
- •
- -
APACHE II and SOFA scores: maximum score obtained in the APACHE II and SOFA scores within the first 24h after ICU admission.
- -
Local complications13: development, at any time and during hospital admission, of infected necrosis (defined as the presence of gas in the pancreatic tissue, a positive result in the Gram staining method or in samples obtained using the fine needle puncture-aspiration technique guided by imaging modalities, in surgical or drain samples), intra-abdominal hemorrhages (defined as the presence of a fluid collection of blood density as seen in the imaging modalities [CT scan, MRI], especially if active extravasation was confirmed after the administration of contrast or the direct visualization of the hemorrhage during surgery) or perforated hollow viscus (defined as a direct visualization during surgery or as the presence of some of the following findings in the imaging modalities: pneumoperitoneum, presence of grouped gas bubbles adjacent to the bowell loop wall, wall thickening, and loss of continuity or discontinuity in the bowell loop wall).
- -
Cause of death: early SIRS (patients who died due to AP-induced organ failure within the first seven days following hospital admission without any data indicative of infection in the pancreatic region), pancreatic infection (based on the definition of infected necrosis given in section “local complications”), local complications (intra-abdominal hemorrhages or perforated hollow viscus based on the previously described definitions [note that the cause of death defined as “local complications” did not include pancreatic infection which, due to its importance, is a well-differentiated cause perse6,7]), and nosocomial extrapancreatic infections [an infection occurring during hospital admission that became evident 72h or more after the patient's hospital admission and was not present when the patient was admitted to the hospital or during the incubation period]; this section included catheter-related infections, respiratory infections [mainly MVS-related pneumonias], and urinary tract infections. Infections were defined using the definitions established by SEMICYUC Infectious Diseases and Sepsis Working Group.14,15
- -
Use of MVS: defined as the need for invasive mechanical ventilation at any time during the ICU stay.
- -
Use of CRRT: defined as the use of CRRT due to acute renal failure at any time during the ICU stay. During the first period of the protocol (2001–2007) the criteria for the use of CRRT were not well regulated and CRRT was started following orders from the treating physician. During the second period of the protocol (2008–2016) the Failure criterion proposed by the RIFLE classification16 was established the following protocol changes made at our ICU for all patients.
- -
Measurement of IAP: the IAP was measured using urinary catheters and based on the definitions established by the International Conference of Experts on Intra-abdominal Hypertension and Abdominal Compartment Syndrome.17 The highest value measured during the ICU stay was recorded.
- -
Need for surgery: defined according to SEMICYUC Consensus Conference on the management of AP from 2012.10 According to our hospital protocol, all surgeries performed on the pancreatic cell due to AP complications required the prior admission of the patient to the ICU. The main indications were these: infected necrosis or pancreatic abscess that could not be treated through minimally invasive step-up drainage approach, perforated hollow viscus, intra-abdominal hemorrhages that could not be treated using endovascular techniques, and abdominal compartmental syndrome that could not be treated with conservative treatment.
The management of sterile necrosis was initially conservative except for cases of 4-week duration and persistence of clinical symptoms.
Depending on when the surgery was performed, it was categorized as early surgery when performed less than 21 days after symptom onset, and late surgery when performed more than 21 days after symptom onset.
- -
Determinant-based classification4:
Mild acute pancreatitis: characterized by the lack of peripancreatic necrosis and organ failure.
Moderate acute pancreatitis: characterized by the presence of any type of peripancreatic sterile necrosis and transient organ failure.
Severe acute pancreatitis: characterized by the presence of any degree of infected peripancreatic necrosis or persistent organ failure.
Critical acute pancreatitis: characterized by the presence of infected peripancreatic necrosis and persistent organ failure.
Statistical analysisWe created one anonymous database with all the information from this study.
All data were analyzed according to the corresponding statistical methodology. The absolute and relative frequencies of qualitative variables were estimated. The quantitative variables that follow a normal distribution were expressed as mean and standard deviation. The qualitative variables that follow a non-parametric distribution, were expressed as mean and percentiles p25–p75.
Quantitative variables were compared using the Student's t test and means were compared using the analysis of variance (ANOVA) to compare the means. When variables were not normally distributed, the Kruskal–Wallis test or the Mann–Whitney-U test were used. Proportions were compared using the chi-square test or Fisher's exact test.
In order to determine the influence of the protocol used and the period of admission, and in an attempt to avoid any confounding factors, one univariate analysis was performed to know which factors impacted mortality. Afterwards, variables with P values<.1 were included in one multivariate logistic regression analysis. The lost values of the variables that were not picked were interpreted using the multiple imputation procedure.
Ethical and legal aspectsThis study has been approved by the Guipuzkoa Clinical Trials Committee. Both the Organic Law 15/1999 on Personal Data Protection and the Royal Decree 994/1999 that passed a series of safety for of automatized files containing personal data were observed. The data from patients were collected anonymously from the electronic database using a numerical code. At no time data that may identify the patients were picked and there was no way of putting together their affiliation and clinical data.
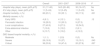
ResultsTwo-hundred-and-eighty-six (286) patients were studied, 94 in the 2001–2007 period and 192 in the 2008–2016 period with a mean age of 59 years old, predominantly males with mainly biliary AP and a 23.07% overall mortality rate. Table 1 shows the general characteristics of the patients included in the study.
Distribution of the sample general variables based on the study period (2001–2007 vs 2008–2016).
| Overall | 2001–2007 | 2008–2016 | P | |
|---|---|---|---|---|
| Number (%) | 286 | 94 (32.8) | 192 (67.1) | |
| Sex (male), n (%) | 193 (67.5) | 62 (65.9) | 131 (68.2) | ns |
| Age (years), mean±SD | 59.5±15.3 | 58.3±15.7 | 60.1±15.2 | ns |
| Etiology, n (%) | ||||
| Biliary | 119 (41.3) | 25 (26.6) | 94 (48.4) | .015 |
| Idiopathic | 55 (19.2) | 25 (26.6) | 30 (15.6) | |
| Enolic | 60 (21) | 24 (25.5) | 36 (18.7) | |
| Other | 52 (18.2) | 20 (21.3) | 32 (16.7) | |
| APACHE II, mean±SD | 13.9±6.2 | 15.5±6.8 | 13.2±5.7 | .003 |
| SOFA, mean±SD | 5.2±3.4 | 7.1±5.1 | 5.1±3.3 | .03 |
| Ranson's score, mean±SD | 1.6±1.1 | 1.9±1.1 | 1.5±0.9 | .002 |
| Balthazar, mean±SD | 6.6±2.6 | 5.8±2.5 | 7±2.6 | .001 |
| Maximum IAP (mmHg), mean±SD | 21.1±6.9 | 25.6±7.1 | 19.8±6.3 | .003 |
| Local complications, n (%) | ||||
| Intestinal perforation | 18 (6.3) | 5 (5.3) | 13 (6.8) | ns |
| Abdominal hemorrhage | 22 (7.7) | 10 (10.6) | 12 (6.3) | |
| Infected necrosis | 112 (39.2) | 31 (33.0) | 81 (42.2) | |
| Use of MVS, n (%) | 165 (57.7) | 66 (69.4) | 99 (51.6) | <.01 |
| Use of CRRT, n (%) | 87 (30.4) | 19 (20) | 68 (35.4) | <.01 |
| Determinant-based classification, n (%) | ||||
| Moderate | 69 (24.1) | 17 (18.1) | 52 (27.1) | ns |
| Severe | 107 (37.4) | 39 (41.5) | 68 (35.4) | |
| Critical | 110 (38.5) | 38 (40.4) | 72 (37.5) | |
APACHE II, Acute Physiology and Chronic Health Evaluation II; CRRT, continuous renal replacement therapy; maximum IAP, maximum intra-abdominal pressure achieved during the ICU stay; MVS, mechanical ventilation support; ns, non-significant; SD, standard deviation; SOFA, Sequential Organ Failure Assessment.
The implementation of the protocol for the management of AP reduced the days prior to the ICU admission, increased the use of enteral feeding, and reduced the use of parenteral feeding and antibiotic prophylaxis. However, the rate of late surgeries did not go up (31.4 vs 26.4%, ns). Table 2 shows the results obtained after the implementation of the protocol.
Distribution of the variables of the management protocol based on the study period (2001–2007 vs 2008–2016).
| 2001–2007 | 2008–2016 | P | |
|---|---|---|---|
| Days of hospital admission-ICU admission, mean (p25–p75) | 2 (1–7) | 1 (1–3) | .033 |
| Type of early feeding (<48h), n (%) | |||
| Parenteral | 84 (89.5) | 88 (45.9) | |
| Enteral | 2 (2.1) | 57 (29.7) | <.01 |
| Mixed | 0 | 7 (3.6) | |
| None | 8 (8.5) | 44 (22.9) | |
| Antibiotic prophylaxis, n (%) | 80 (85.1) | 67 (34.8) | <.01 |
| Surgical procedure, n (%) | 47 (50) | 87 (45.3) | ns |
| Day of procedure, mean (p25–p75) | 17 (7–28) | 10 (3–25) | .015 |
| Late surgery (>21 days), n (%) | 30 (31.4) | 52 (26.4) | ns |
ICU, intensive care unit; ns, non-significant.
There were changes between both periods when it comes to the characteristics of the patients and the number of patients included in the study. During the second period, there was a larger number of patients hospitalized with lower Ranson's, APACHE II and SOFA scores within the first 24h with a higher degree of ultrasound-guided damage according to the Balthasar score. Similarly, the patients included in the second period showed a higher percentage of biliary AP, a lower maximum IAP, required less MVS, and had a pressing need for CRRT.
When it comes to clinical results, we can confirm a drop in the hospital mortality rate between both periods (35.1 vs 17.18%, P=.001) with a variation in the causes of death: less extra-abdominal infections and early SIRS during the 2008–2016 period, and more local complications (intestinal perforations, intraabdominal hemorrhages) and other causes. The analysis of mortality following the determinant-based classification showed a significant drop in the subgroup of patients with severe AP (37 vs. 19.1%) during the 2008–2016 period. No other significant changes were seen with respect to the ICU stay or the hospital stay. Table 3 shows a comparison of the results obtained between both periods.
Distribution of the variables of clinical progression based on the study period (2001–2007 vs 2008–2016).
| Overall | 2001–2007 | 2008–2016 | P | |
|---|---|---|---|---|
| Hospital stay (days), mean (p25–p75) | 31 (17–60) | 34.5 (20–62) | 30 (16–57) | Ns |
| ICU stay (days), mean (p25–p75) | 11 (5–24) | 12 (5–25) | 11 (5–23) | Ns |
| Hospital mortality, n (%) | 66 (23.1) | 33 (35.1) | 33 (17.2) | .001 |
| Mortality causes, n (%) | ||||
| Early SIRS | 4 (6.1) | 4 (12.1) | 0 (0) | .12 |
| Pancreatic infection | 19 (28.3) | 10 (30.3) | 9 (27.3) | |
| Local complications | 27 (40.9) | 9 (27.3) | 18 (54.5) | |
| Extra-abdominal infection | 7 (10.6) | 5 (15.2) | 2 (6.1) | |
| Other | 9 (13.7) | 5 (15.2) | 4 (12.2) | |
| DBC-based hospital mortality, n (%) | ||||
| Moderate | 1 (1.1) | 1 (5.9) | 0 (0) | Ns |
| Severe | 28 (18.9) | 15 (37) | 13 (19.1) | .043 |
| Critical | 38 (33.9) | 18 (47.4) | 20 (27.8) | .057 |
DBC, determinant-based classification; ICU, intensive care unit; ns, non-significant; SIRS, systemic inflammatory response syndrome.
As the methodology describes, one univariate analysis of the different quantitative and qualitative factors associated with mortality was performed in the first place (Table 4). The variables associated with mortality in a statistically significant way were age, the APACHE II score, IAP, the SOFA score, Ranson's score, the protocol period, etiology, the use of MVS and CRRT, and severity according to the determinant-based classification.
Univariate analysis of qualitative/quantitative variables with respect to hospital mortality.
| Variable | Alive (n=220) | Dead (n=66) | P |
|---|---|---|---|
| Age (years), mean±SD | 57.1±15.6 | 67.6±11.4 | .000 |
| Sex (male), n (%) | 154 (70) | 39 (59.1) | ns |
| Body mass index (kg/m2), mean±SD | 29.1±23.6 | 26.7±5.2 | ns |
| Protocol period, n (%) | |||
| 2001–2007 | 61 (27.7) | 33 (50) | |
| 2008–2016 | 159 (72.3) | 33 (50) | .001 |
| Hospital-ICU days, mean (p25–p75) | 2 (0–4) | 1 (0.75–2) | ns |
| Etiology, n (%) | |||
| Alcoholic | 51 (23.2) | 9 (13.6) | .017 |
| Biliary | 94 (42.7) | 24 (36.4) | |
| Hyperlipidemia | 14 (6.4) | 3 (4.5) | |
| Idiopathic | 32 (14.5) | 23 (34.8) | |
| Post-ERCP | 23 (10.5) | 6 (9.1) | |
| Other | 6 (2.7) | 1 (1.5) | |
| Maximum APACHE II score within the first 24h, mean±SD | 12.3±5.2 | 19.8±6.2 | .000 |
| Maximum SOFA score within the first 24h, mean±SD (lost values=87 cases) | 4.7±3.1 | 7.8±4.0 | .000 |
| Ranson's score, mean±SD | 1.5±1.0 | 2.1±1.1 | .000 |
| CT scores (Balthazar), mean±SD | 6.5±2.6 | 7.1±2.7 | ns |
| Maximum IAP within the first 24h (mmHg), mean±SD (lost values=216 cases) | 19.3±6.4 | 24.7±6.7 | .002 |
| Surgery, n (%) | 97 (44.1) | 37 (56.1) | ns |
| SP day, mean (p25–p75) | 15 (4.5–27) | 8 (2–20) | ns |
| Use of CRRT, n (%) | 50 (22.7) | 37 (56.1) | .000 |
| Use of MVS, n (%) | 106 (48.2) | 59 (89.4) | .000 |
| Feeding within the first 48h, n (%) | |||
| Parenteral | 134 (60.9) | 38 (57.6) | ns |
| Enteral | 42 (19.1) | 13 (19.7) | |
| Mixed | 6 (2.7) | 1 (1.5) | |
| None | 38 (17.3) | 14 (21.2) | |
| Local complications, n (%) | |||
| Intestinal perforation | 10 (4.5) | 8 (12.1) | ns |
| Abdominal hemorrhage | 15 (6.8) | 7 (10.6) | ns |
| Infected necrosis | 83 (37.7) | 29 (43.9) | ns |
| Determinant-based classification, n (%) | |||
| Moderate | 68 (30.9) | 1 (1.5) | |
| Severe | 80 (36.4) | 28 (42.4) | .000 |
| Critical | 72 (32.7) | 37 (56.1) | |
APACHE II, Acute Physiology and Chronic Health Evaluation II; CRRT, continuous renal replacement therapy; CT, computed tomography scan; IAP, intra-abdominal pressure; ICU, intensive care unit; MVS, mechanical ventilation support; ns, non-significant; Post-ERCP, post-endoscopic retrograde cholangiopancreatography; SD, standard deviation; SOFA, Sequential Organ Failure Assessment; SP day, surgical procedure day.
Then one multivariate logistic regression analysis was performed (Table 5). These were the variables that showed losses: maximum SOFA score withing the first 24h (87 cases, 30.4%), maximum IAP during the ICU stay (216 cases, 75.5%), body mass index (19 cases, 6.64%), the Balthazar score (6 cases, 2.10%), and Ranson's score (37 cases, 12.93%). The values lost were treated using the multiple imputation procedure to avoid excluding any cases, except for the IAP, that due to its high percentage of losses was eliminated right away from the multivariate analysis.
Hospital mortality-adjusted multivariate analysis.
| Variable | B | SE | Wald | df | OR (95%CI) | P |
|---|---|---|---|---|---|---|
| Period 2008–2016 | −1.069 | 0.396 | 7.275 | 1 | 0.34 (0.15–0.74) | .007 |
| Maximum APACHE II score within the first 24h | 0.162 | 0.038 | 17.765 | 1 | 1.17 (1.09–1.267) | .000 |
| Surgical procedure, no | −1.563 | 0.597 | 6.856 | 1 | .009 | |
| Use of mechanical ventilation | 1.984 | 0.670 | 8.765 | 1 | 7.27 (1.95–27.04) | .003 |
| Age (years) | 0.044 | 0.017 | 7.005 | 1 | 1.04 (1.01–1.07) | .008 |
| Determinant-based classification | 2 | .054 | ||||
| Moderate | 5.822 | 1 | ||||
| Severe | 1.116 | 1.132 | 0.973 | 3.05 (0.33–28.06) | .324 | |
| Critical | 2.219 | 1.199 | 3.423 | 9.19 (0.87–96.52) | .064 | |
95%CI, 95% confidence interval; APACHE II, Acute Physiology and Chronic Health Evaluation II; df, degrees of freedom; MVS, mechanical ventilation support; OR, odds ratio; SE, standard error.
The period when the protocol was implemented showed a statistically significant correlation with mortality for those admissions occurring during the 2008–2016 period vs the 2001–2007 period (Table 5). Other factors associated in a statistically significant way were age, the APACHE II score, the use of MVS and not performing any surgeries. The Determinant-based Classification showed P values=.054 that were not considered statistically significant.
DiscussionThis paper studied the clinical impact of implementing a protocol for the management of patients with AP who were admitted to an ICU based on SEMICYUC Consensus Conference from 2007.10 We studied a retrospective series of 286 patients with a high percentage of severe and critical forms of the disease according to the determinant-based classification.4 This is the largest series ever published to this day.
The recommendations established by the Consensus Conference described several issues with room for improvement on the management of patients with AP admitted to ICUs such as the use of early enteral feeding, early ICU admissions, delayed surgeries, and withdrawal of antibiotic prophylaxis. The degree of accomplishment of the study endpoints was significant with respect to early admissions, use of early enteral feeding,18 and withdrawal of antibiotic prophylaxis,19,20 except for late surgeries, which means that there is still room for improvement in our ICU. The protocolized monitoring of IAP was another improvement included back in 2012 following changes in the SEMICYUC recommendations for that year,10,21 since its impact on the clinical progression of AP has been well-documented.22,23 However, since data mining was retrospective, there was a high percentage of cases where IAP could not be recorded so a decision was made not to include it as a result of the change in the management of patients or in the multivariate analysis either. The minimally invasive or zero invasive management of infected pancreatic necrosis started back in 201312 and it may have impacted the final outcomes, yet this was not specifically addressed in this study.
When it comes to the clinical outcomes, there were significant changes between 2001–2007 and 2008–2016: more cases, lower scores in severity markers, and a significant reduction of hospital mortality with changes in the causes of death. It is striking to see that there were no significant changes when it comes to the ICU and hospital stays between both periods. That is why data should be interpreted with caution. There was a 50% relative reduction of the mortality rate between both protocol periods, whereas the absolute hospital mortality rate was <20% in the second period. This mortality rate was much lower that the one described in other series: for instance, Bumbasirevic et al. described a 53.6% mortality rate in patients with AP admitted to ICUs5; one recent multicentric study conducted in 46 ICUs confirmed mortality rates of up to 28.7%.13 If we analyze the categories from the Determinant-based Classification, the decreased mortality rate observed was significant in the case of severe APs, whereas the mortality rate shown in this study by patients with severe and critical AP was lower compared to other series.24–28 It seems that this reduced mortality rate was due not only to more admissions of milder forms of the disease during the 2008–2016 period but also to a better management of these patients.
Similarly, there were changes in the causes of death since the mortality rate associated with extra-abdominal infections such as early SIRS was significantly reduced, while the mortality rate associated with local complications went up (intestinal perforations, intra-abdominal hemorrgages). We believe that early admission together with improved support measures may explain the lower mortality rate due to early SIRS as other authors have already described.9,29–31 When it comes to local complications, there were not significant changes in the percentage of patients who developed these complications between both periods or in the mortality rate, similar to what has already been reported by other series.30–32 However, there was a percentage gain in the overall mortality of patients who died due to intestinal perforations and intra-abdominal hemorrhages. The decrease of mortality rate due to early SIRS and extra-abdominal infections may have been a contributing factor together with how difficult it is to treat these complications, added to their late onset, in patients who already had significant organ damage, and infected necrosis previously treated on many occasions.
Since there may have been confounding factors that would explain the reduced mortality seen between both periods, one multivariate logistic regression analysis was conducted where the period of treatment was variable and significantly associated with hospital mortality. This multivariate analysis had several limitations particularly if we take into consideration that data were collected retrospectively. There were very few lost values, except for the maximum SOFA score within the first 24h of the ICU stay that were handled using the multiple imputation procedure. As we have already said, the maximum IAP collected was excluded right away due to its high percentage of lost cases, which may have impacted the final outcomes.
Added to the retrospective nature of the study and the potential impact of the lost values, there were other limitations that make us be extra cautious when it comes to interpreting the good results coming from a lower mortality rate. As we said before, during the 2008–2016 period there was a change in the patients’ clinical profile, with more patients and less severity according to the APACHE II, SOFA and Ranson scores and probably due to earlier admissions. Also, there were changes in the etiology of these patients, less use of MVS and greater use of CRRT. The greater use of CRRT had to do with general changes taking place in our ICU when the Failure criterion proposed by the RIFLE classification was established. Several studies confirm that the use of CRRT may reduce mortality in the most severe cases of AP, which may have impacted our results.33,34 Also, the long period of data mining and its single-center nature may have impacted other general changes and in turn conditioned our own results; we are talking about something we may have missed in our study such as safety policies or campaigns for the reduction of nosocomial infections.35,36
It would be interesting that the experience from our center were somehow validated by other hospitals or studied retrospectively in larger multicentric series and in a shorter period of time to see whether there is an improvement in the clinical progression of patients with AP admitted to ICUs.
ConclusionsThe implementation of a protocol for the management of patients with AP admitted to ICUs based on the VII Consensus Conference organized by SEMICYUC resulted in better approaches for these patients when it comes to early ICU admissions, use of enteral feeding, and withdrawal of prophylactic antibiotic therapy. Also, all of this may have reduced hospital mortality.
AuthorsBoth Leyre Amas and Felix Zubia contributed to the processes of data mining, data analysis and interpretation, study design, and writing of the manuscript. Both of them approved the final version of this manuscript too.
Conflicts of interestThe authors declared no conflicts of interest whatsoever.
We wish to thank Gabriel Txoperena and Iñaki Arcega for their contribution in the statistical analysis and proofreading stage of this manuscript.
Please cite this article as: Amas Gómez L, Zubia Olaskoaga F. Resultados de la modificación de un protocolo de manejo para la pancreatitis aguda en Medicina Intensiva. Med Intensiva. 2019;43:546–555.