A narrative review is presented on the diagnosis, treatment and management of accidental hypothermia. Although all these processes form a continuum, for descriptive purposes in this manuscript the recommendations are organized into the prehospital and in-hospital settings.
At prehospital level, it is advised to: (a) perform high-quality cardiopulmonary resuscitation for cardiac arrest patients, regardless of body temperature; (b) establish measures to minimize further cooling; (c) initiate rewarming; (d) prevent rescue collapse and continued cooling (afterdrop); and (e) select the appropriate hospital based on the clinical and hemodynamic situation of the patient.
Extracorporeal life support has revolutionized rewarming of the hemodynamically unstable victim or patients suffering cardiac arrest, with survival rates of up to 100%.
The new evidences indicate that the management of accidental hypothermia has evolved favorably, with substantial improvement of the final outcomes.
La presente revisión narrativa se centra en el diagnóstico, el tratamiento y la gestión de la hipotermia accidental. Si bien todos estos procesos son continuos, en el presente manuscrito las recomendaciones se organizan con fines descriptivos en prehospitalarias y hospitalarias.
En el ámbito prehospitalario se recomienda: a) reanimación de alta calidad de toda víctima en parada cardiaca, independientemente de la temperatura corporal; b) instaurar medidas para detener la pérdida de calor; c) iniciar el recalentamiento; d) prevenir el colapso del rescate y el efecto de recaída (afterdrop) y e) elegir adecuadamente el hospital de referencia de acuerdo con la situación clínica y hemodinámica de la víctima.
El soporte vital extracorpóreo ha revolucionado, con tasas de supervivencia que han llegado al 100%, el recalentamiento de víctimas con inestabilidad hemodinámica o paro cardiaco.
Las nuevas evidencias indican que la gestión de la hipotermia accidental ha evolucionado y ha conseguido mejorar sustancialmente el pronóstico final.
Accidental hypothermia (HT) is defined as an unintentional drop in core body temperature (CBT) to under 35°C.
Although HT is related to cold and typically to parts of the world with a harsh winter, it can also be seen in warmer climates, in the summer months, and in hospitalized patients. In addition, it can be accompanied by other situations such as trauma, drowning, snow avalanche, sepsis, metabolic, endocrinological or other diseases such as cancer, or cerebrovascular diseases, that affect thermoregulation.1
Body temperature reflects the balance between heat production and heat loss. Heat is generated by cell metabolism, particularly in the heart and liver, and is lost through the skin and lungs. The processes involved are2: evaporation (vaporization of water through insensible losses and perspiration), radiation (heat transfer in the form of infrared electromagnetic radiation), conduction (direct heat transfer to an adjacent colder object or medium) or convection (direct heat transfer to air or water currents). Heat loss through convection in cold air environments and conductive heat loss in a medium such as water are the most common mechanisms underlying accidental HT.3
The normal human CBT is 37±0.5°C. The body maintains that temperature whenever possible, using a series of autonomous mechanisms that regulate heat loss or gain, depending on the environmental conditions. However, since the physiological capacity to respond to cold environmental conditions is limited, there are a series of adaptive behaviors (clothing or seeking refuge) that are essential for combating HT.
The hypothalamus is the anatomical region where the body thermostat is located, and controls temperature through the information it receives from the central and peripheral thermal receptors.2,3 The main neurohumoral mechanisms that participate in this complex process, from the start and until disappearance of the vital signs, are summarized in Table 1.1,3–11
Neurohumoral processes intervening in accidental hypothermia.1,3–11
| Cardiovascular |
| Initial effect |
| •Elevation of blood pressure and cardiac output (due to increase in catecholamines) |
| •Vasoconstriction (sympathetic reaction: increased vascular resistance) |
| Posterior effect |
| •Linear progressive bradycardia (due to decrease in cardiac pacemaker cell automatism) |
| •Decrease in atrial and cardiac arrhythmias threshold (due to increase in the duration of the action potentials and decrease in transmembrane resting potential of the His-Purkinje system) |
| •Ventricular fibrillation (due to hypovolemia, hypoxia, pH alteration and mechanical irritation) |
| •Changes in ECG tracing (due to effect of cold upon membrane channels and currents) |
| •Diminished cardiac output (due to increase in afterload, lowered heart rate and diminished calcium sensitivity) |
| •Cessation of vasoconstriction (due to drop in vascular resistance) |
| •Decrease in blood pressure and low organ flow status |
| Central and peripheral nervous system |
| Initial effect |
| •Stimulation of brain metabolism |
| Posterior effect |
| •Decrease in oxygen consumption concomitant to temperature (6% for each grade) |
| •Transient cerebral organic syndrome: behavioral changes, disorientation, amnesia, apathy, dysarthria, ataxia (due to reduction or failure of the function of enzymes dependent upon temperature and ion channels) |
| •Ischemic tolerance to periods of low or no flow (due to decrease in oxygen consumption and possible reduction of cerebrovascular membrane permeability) |
| •ECG alterations, to the point of a flat tracing (due to disappearance of cortical and thalamic responses) |
| •Pupil dilatation and non-reactivity, and absent corneal reflexes (therefore of no prognostic use in hypothermia) |
| •Lowered or absent reflexes (due to decrease in peripheral nervous activity) |
| Respiratory |
| Initial effect |
| •Hyperventilation (due to strong influence of skin thermoreceptors upon respiratory function) |
| •Increase in oxygen consumption and metabolism (due to increase in catecholamines and thyroxin) |
| Posterior effect |
| •Decrease in tidal volume, respiratory frequency, compliance, thoracic elasticity, and increase in dead space |
| •Failure of ventilation neurocontrol in brainstem |
| •Decrease in consumption of O2 and production of CO2 |
| •Respiratory acidosis (due to decrease in tidal volume and respiratory frequency) |
| •Decrease in protective reflexes of the airway, ciliary motility, increased secretions viscosity and bronchospasm |
| Endocrinological |
| Initial effect |
| •Increased production of stress hormones: cortisol, catecholamines, thyroxin (to increase metabolic rate, produce more energy, and try to keep core body temperature constant) |
| Posterior effect |
| •Inefficacy of the stress hormones in maintaining core body temperature |
| Electrolyte balance and renal function |
| Initial effect |
| •Peripheral vasoconstriction in response to cold, fluid passage from intracellular to extracellular compartment, increased in hematological concentration and hematocrit |
| •Inhibition of antidiuretic hormone: cold diuresis due to relative central hypervolemia, increased blood pressure |
| •Temperatures<25°C: alterations in tubule function appear, referred to sodium, calcium, chloride, potassium and hydrogen ions |
| •Immersion in cold water: increases urine elimination 3.5-fold (due to effect of peripheral vasoconstriction) |
There have been substantial advances in the management of accidental HT. The hospital mortality rate of severe HT victims has decreased from a reported 53.4% in the year 2001 (mortality study corresponding to the period 1992–2001)12 to zero in 2012 (in a published series comprising 15 victims).13 This radical change is fundamentally attributable to the adoption of extracorporeal life support (ECLS), which will be described further below.11–14
The present narrative review analyses the recent advances in the diagnosis, treatment and management of accidental HT, without addressing the physiopathological and clinical aspects, which can be found in other reviews.1
For descriptive purposes and improved understanding, the narrative review has been organized into pre-hospital and in-hospital recommendations – though all the processes involved form a continuum, since they are part of the same management chain.
Pre-hospital management of accidental hypothermiaEvaluationClassification of hypothermia based on the measurement of core body temperatureCore body temperature is the most standardized physiological parameter for diagnosing and classifying the severity of HT. Mild HT is defined as CBT between 32 and 35°C, while moderate HT is defined as CBT between 28 and 32°C, and severe HT is defined as CBT<28°C.15,16 Furthermore, some experts also include deep hypothermia (CBT 20–24°C)7,15 or modify mild HT (temperature 36°C in the presence of trauma).17
Pre-hospital classification of accidental hypothermia: the Swiss systemThe Swiss system for the pre-hospital classification of HT, developed to help rescue teams, estimates CBT from the observation of clinical signs and allows the stratification of severity without having to actually measure CBT (such measurement often being difficult to obtain in the rescue zone17). Based on observation of the level of consciousness and the patient vital signs, 5 grades of HT are identified, with the corresponding correlation to estimated CBT15:
- •
Mild (grade I or HT I): conscious and shivering victim (35–32°C).
- •
Moderate (grade II or HT II): drowsy and non-shivering victim (32–28°C).
- •
Grave (grade III or HT III): unconscious victim, but with positive vital signs (28–24°C).
- •
Deep (grade IV or HT IV): apparent death, due to absence of vital signs (13.7–24°C).
- •
Irreversible (grade V or HT V): irreversible death due to HT: totally frozen body (<9–13°C).
The main limitation of the Swiss system is the individual physiological variability in relation to HT. Because of this variability, the estimation of CBT based only on the clinical signs represents an approximation. For example, in some victims shivering may be present at temperatures of under 30°C, or the vital signs may be present at under 24°C – a temperature at which the risk of ventricular fibrillation (VF) is high.18,19 An analysis of the published cases found a strong correlation between CBT and the grade of HT, though in other cases CBT was seen to be overestimated. A revision of this classification, with the analysis of the mentioned cases, corrected CBT to levels lower than those observed. Thus, CBT for HT I would be 28.1°C, versus 22.1°C for HT II and 19.3°C for HT III.18,20
On the other hand, shivering and level of consciousness can be affected by factors such as age, gender, body composition, race, associated conditions such as trauma, central nervous system diseases and intoxication caused by toxic agents, etc., or the administration of drugs such as sedatives, muscle relaxants and opiate analgesics.11
Measurement of core body temperatureThe body measurement zones, in decreasing order of invasiveness, are the pulmonary artery, esophagus, bladder, rectum, eardrum (epitympanic measurement), mouth and skin. The most reliable measurement is that obtained from the pulmonary artery, but it is not advised because of its invasiveness and the risk of triggering arrhythmias.
Esophageal temperature measurement is minimally invasive, correlates well to pulmonary artery temperature, and is very useful in the monitoring and treatment of victims with diminished level of consciousness.18,19 The esophageal catheter should be placed in the lower third of the esophagus in order to avoid overestimating CBT when rewarming is made with warm and humidified oxygen.21
Epitympanic temperature recording correlates well to carotid temperature. It is useful in victims that breathe spontaneously, but is categorically discarded (due to measurement error) in the presence of very low external temperatures, water or snow within the external auditory canal, hemodynamic instability or cardiac arrest (CA).22,23
Rectal and bladder temperature measurements are not recommended outside warm environments or in the rewarming of unconscious victims. Measurement during rewarming may result in underestimated (delay of up to 1h with the real CBT value) or overestimated readings (if performed with peritoneal or colon lavage).11,18,19 Oral cavity or skin temperature measurement is only useful in normothermia.11
The so-called temporal artery thermometers, which measure at the skin surface, do not afford accurate recordings in situations of HT.24
The heat flux thermometer is a novel and noninvasive method which in the Intensive Care Unit (ICU) offers an accurate CBT value.25 If such accuracy is confirmed in the pre-hospital setting, it could prove useful for evaluating and monitoring the treatment of HT.
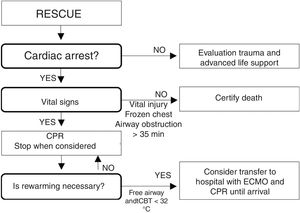
Temperature as a guiding factor for treatmentCore body temperature is a standardized parameter for classifying HT.14–16 However, a drop in CBT is accompanied by great individual clinical variability referred mainly to level of consciousness, the intensity of shivering or hemodynamic stability.26 Based on this variability, and since it is not always possible to measure CBT in the pre-hospital setting, or many rescue teams lack the necessary measuring device,17,27–29 the recommended key factors guiding treatment are the level of consciousness, the intensity of shivering and hemodynamic stability based on blood pressure and heart rate (Fig. 1).11,18,19 The measurement of CBT affords useful additional information.18
Decision algorithm for the pre-hospital management of accidental hypothermia.11,18,19 (a) HT II (drowsiness)/HT III (unconsciousness). (b) Decapitation, full sectioning of the trunk, decomposition or totally frozen body (HT V). ECMO: extracorporeal membrane oxygenation; HT: hypothermia; CA: cardiac arrest; CPR: cardiopulmonary resuscitation; ICU: Intensive Care Unit.
In HT, oxygen consumption decreases 6% for every 1°C drop in CBT, and this decrease also affects the central nervous system. The drop in oxygen consumption means that HT has a preventive effect in terms of cerebral and spinal cord hypoxia – thus allowing full neurological recovery after prolonged situations of CA.4,30Table 2 describes the most extreme published cases of accidental HT and their neurological recovery, which proved practically complete in all instances.31–38
Most extreme published cases of accidental hypothermia and their neurological recovery.
| •Longest time without vital signs: 42 years, 7min under water and 70min of transfer in asystolia to hospital. Complete neurological recovery31 |
| •Longest manual CPR: 42 years, 6h 30min. Rewarming with noninvasive methods. Complete neurological recovery32 |
| •Longest mechanical CPR: 25 years; start of manual CPR 3h and 5min and 2h with 40min of mechanical CPR. One hour rewarming with ECMO until electrical activity with pulse achieved. Total 6h 45min. Complete neurological recovery33 |
| •Longest intermittent CPR: 57 years; alternating 1min of CPR and 1min walking for 25min. In total, 5h of CPR. Rewarming with ECMO. Complete neurological recovery34 |
| •CPR with longest total resuscitation time: 8h and 40min; cardiac arrest: 4h and 48min. ECMO: 3h and 52min. Complete recovery except minimum semantic memory defect not affecting normal life of the patient35 |
| •Lowest temperature with recovery: 29 years; CBT: 13.7°C. Fall into a ravine with frozen water. In situation of cardiac arrest for about 45min. Rewarming with ECMO. Complete neurological recovery36 |
| •Longest immersion: 2.5 years; immersion in cold water for at least 66min. CBT: 19°C. Rewarming with ECMO. Complete neurological recovery37 |
| •7 years; immersion in cold water for at least 83min. CBT: 13.8°C. CPR during 64min. Serum potassium: 11.3mmol/l. Rewarming with ECMO. Complete neurological recovery38 |
CPR: cardiopulmonary resuscitation; CBT: core body temperature.
Of all the factors that have been related to drowning survival rate, the only established predictive parameter has been immersion time. In this regard, an immersion of under 5min is associated to favorable outcomes, while immersion periods of over 25min invariably prove fatal.39,40
There has been much speculation about the relationship between survival and the age of the victim. Children, and especially small infants, cool much faster than adults following immersion in cold water (<6°C),41,42 and exhibit inefficient trembling,43 have less subcutaneous fat44,45 and present a larger surface area in relation to body weight compared with adults.42 No clear relationship has been evidenced to date, however.39,40
Cases of miraculous survival with good neurological recovery after immersion in cold water, particularly in children37,38,46–48 but also in adults,36,44,49,50 led to the belief that the temperature of the water prevented cerebral hypoxia.11 This relationship likewise has not been confirmed, however.39,40
Burial by snow avalancheMost deaths due to snow avalanches are attributable to asphyxia, trauma and HT,51 with asphyxia being the predominant mechanism: it causes 80% of all avalanche fatalities.52 When the airway is not permeable, death occurs in the first 35min of becoming buried. Any open air space around the mouth or nose increases survival.53
The cooling of a victim buried by an avalanche may be rapid, particularly if asphyxia is present.19 The average cooling rates are between 0.8°C/h and 3°C/h, though there have been reports of cooling rates of 9°C/h.19,51,52
In 2015, the European Resuscitation Council (ERC), based on prognostic factors such as the severity of trauma (lethal or non-lethal), the duration of complete burial (>60min or ≤60min), CBT (≥30°C) and serum potassium (<8mmol/l or >8mmol/l) modified its previous recommendations and established a new recommendation for the resuscitation of avalanche victims (Fig. 2).51 More recent algorithms (Fig. 3)52 propose returning to the burial times indicated in the guide of the year 200154: do not start cardiopulmonary resuscitation (CPR) if the airway is obstructed and the burial time has been >35min. They consider that CPR can only prove successful with a burial time of under 35min, regardless of airway patency.
Algorithm for assessment and intervention in the case of victims that have been completely buried by a snow avalanche. Indications of ECLS51. EAWP: electrical activity without pulse; VF: ventricular fibrillation; CPR: cardiopulmonary resuscitation; ECLS: extracorporeal life support; VTWP: ventricular tachycardia without pulse.
Triage and decision making algorithm for avalanche victims under conditions of cardiac arrest. Source: Modified from Kornhall DK, Martens-Nielsen J. The prehospital management of avalanche victims. J R Army Med Corps. 2016;162:406–412. doi:10.1136/jramc-2015-000441.52
The first priority of rescue is the safety of the intervening team. The scenario may be dangerous, and staying there might be possible only once and for a brief period of time. Under these circumstances, and except in the clear presence of fatal injuries, the victim must be moved to a safer place before any decision can be made, including CPR if the victim is in CA.18,19
Insulation and rewarmingMaintaining CBT is the next priority. The body of the victim should be wrapped in insulating material during and after rescue, with the purpose of avoiding further heat loss. Most heat loss occurs as a result of exposure of the head and neck to the environmental cold, and direct contact of the victim with the ground or stretcher.11,18,19
At present, pre-hospital rewarming is considered to be safe and beneficial, and the most effective insulation systems combine insulation with a vapor barrier.53
The vapor barrier protects against convection and evaporation, and can be applied with bubble plastic material, insulating blankets, plastic sheeting, trash bags or any other material capable of affording an impermeable and sealed layer, though always leaving the face exposed in order to allow breathing.55 In victims with dry clothing, the material is applied as the outermost layer. If the clothing is wet and cannot be changed, placing the barrier between the wet clothing and the dry layers could be an effective measure.18,19,56 Although further research is required to demonstrate its true efficacy,28 not changing the wet clothing would be of great benefit, since the victim would be moved less, with less exposure to the environmental cold, and with a lesser risk of further drops in CBT.
Shivering and active movements (where indicated) remain very effective for producing warmth and for rewarming conscious victims capable of movement (HT I). Shivering, which increases energy expenditure and oxygen demand, is uncomfortable for the victim and moreover requires the administration of warm liquids and carbohydrate-rich foods. Exhaustion of the energy reserves would cause the disappearance of trembling.57 The temperature of the liquids and foods must be controlled to avoid burns.
Other still valid alternative or complementary active external rewarming techniques are the use of reflectant blankets, electric cushions, chemical heat packs of sufficient size for the axillas, chest and back, or the administration of warm and humidified oxygen.1 These measures attenuate shivering, avoid energy depletion, and afford comfort for the victim. The heat sources should never be applied directly to the skin, as this may cause burns. Rewarming of the upper trunk is safer and more effective than rewarming of the extremities. Body-to-body rewarming inside a sleeping bag with a warm person also serves to reduce shivering, but should not be allowed to delay evacuation of the victim.11,18,19
Guaranteeing safe rescue and rewarming of a victim not in a situation of CA implies the prevention of rescue cardiovascular collapse and further drops in CBT (afterdrop).
Rescue collapseRescue cardiovascular collapse refers to syncope or sudden death in victims immersed in cold water occurring just before rescue, during or after rescue, or even later. It is attributed to sudden hypotension or ventricular fibrillation.58 The cessation of the hydrostatic pressure exerted by the water upon the body may trigger such hypovolemic shock.1,19 It has also been related to arterial hypotension secondary to a decrease in catecholamine release, coinciding with mental relaxation, when rescue is imminent.44 In order to prevent this situation, it is advisable to move the victim carefully – as with all hypothermia victims – and keep him/her in a horizontal position.1,18,19,44 This type of collapse has also been described in terrestrial rescue operations.31,59
AfterdropAfterdrop refers to the additional drop in CBT once the victim has been protected from the cold and rewarming has started. The highest incidence of afterdrop is observed during the rewarming of moderate to severe HT. This serious complication, which can trigger ventricular fibrillation, has been related to peripheral vasodilatation and the return to the heart of the cold blood with acidemia accumulated within the extremities. Exclusive rewarming of the lower extremities or applying hot showers or baths facilitates the appearance of afterdrop. There is still controversy as to whether this effect is exclusively related to active external rewarming or to any other form of rewarming.5
Experimental studies have shown that small changes in temperature (0.5–1°C) in conscious and collaborative victims (HT I) can cause this effect with minimally invasive rewarming accompanied by physical exercise. For this reason, some experts consider that the victims should remain at rest for 30min, if allowed by the circumstances and provided there is no undue risk for the rescuers.18,19 In practice, mobilization should not be impeded if the victim is conscious and can contribute to rescue.11,60
Airway and oxygenationIt is difficult to measure oxygen saturation in the HT patient. Using supplementary oxygen at altitudes of over 2500m could be useful for avoiding hypoxemia.18
The indications for securing the airway are the same as in normothermal patients. Endotracheal intubation in HT can cause ventricular fibrillation, but the advantages outweigh this risk.51 If the cuff of the endotracheal tube is too insufflated with cold air, it could rupture during rewarming as a result of expansion.19 Trismus caused by cold is usually resistant to neuromuscular block and could impede laryngoscopy. In these cases the use of a supraglottic device is the first choice for management of the airway.
Neuromuscular block is ineffective below 30°C, and since metabolism is diminished until normothermia is reached, the effect is prolonged during rewarming.19 If succinylcholine is used for intubation, it must be taken into account that HT increases its capacity to elevate the potassium levels, reduces neuromuscular transmission, and enhances sensitivity to non-depolarizing muscle relaxants.11,61
The metabolism of most anesthetic agents is decreased in HT, including that of ketamine and propofol – a fact that may produce toxicity and hemodynamic alterations. It is advisable to administer such agents at lower doses and at greater intervals.62 Ketamine may be used, but its sympathomimetic effects upon the hypothermic and irritable heart could increase the instability.57
Hyperventilation in HT has many potential harmful effects, including a decrease in cerebral blood flow. Capnography should not be used in severe HT as the main criterion guiding the ventilatory parameters due to dissociation between end-tidal CO2 (EtCO2) and the partial arterial pressure of CO2 (pCO2). A drop in value reflects hemodynamic instability, with practically complete disappearance in the presence of CA. Monitoring the values is an alternative for assessing cardiac output.63
Hemodynamic supportVenous accessVenous access is usually difficult because of the peripheral vasoconstriction. An important alternative, due to its similar multifunctionality, is an intraosseous access.1,19 The femoral route is free of the risk of ventricular fibrillation and is therefore the only accepted central access, but should be reserved for extracorporeal life support (ECLS).
Management of fluid therapyThe circulatory volume in moderate to severe HT is reduced. This situation begins to manifest during rewarming as peripheral vasoconstriction gradually subsides. In order to secure hemodynamic stability, it is advisable to administer the required amount (with control of overload) of physiological saline solution warmed to 41–42°C. In order to maintain the temperature, the most practical approach is to administer it in bolus form rather than as a continuous infusion.7
However, fluid therapy as a measure to warm the victim is not very effective. Danzl and Huecker calculated that each liter administered at 42°C provides 14kcal to a 70-kg victim with a CBT of 28°C, and elevates CBT by only 0.33°C.64 Enormous warm fluid volumes therefore would be needed to substantially elevate CBT.
Future investigations are needed to evaluate the effectiveness of recently developed battery-equipped liquid warming devices.53
Dosing of vasoactive drugs and antiarrhythmic agentsMost studies of these drugs have been carried out in animals. Because of the limited available evidence, they should not be administered to patients with CBT<30°C.65
In the presence of bradycardia with hypotension, the use of a percutaneous pacemaker should be considered (intravenous pacemakers are contraindicated due to the risk of arrhythmias).19
DefibrillationElectrocardiographic monitoring is the best method for diagnosing lethal arrhythmias or CA. Lethal arrhythmias such as ventricular tachycardia or ventricular fibrillation usually do not respond to defibrillation until CBT has risen to reach 30°C – though there have been reports of successful defibrillation with CBT 24.2°C.66 It is advisable to attempt three cycles of adrenalin/defibrillation (at maximum discharge) in situations below 30°C. If unsuccessful, CPR should be continued, and repetition should not be made until CBT rises 1–2°C or until 30°C is reached.52 Once the latter temperature has been reached, we should continue with the recommendations of the current CPR guides.51,67
Cardiopulmonary resuscitationTemperature as resuscitation criterionThe lowest CBT successfully resuscitated in an accidental HT victim was 13.7°C.36 The lowest therapeutically induced CBT was 9°C.68 In both cases recovery was without neurological sequelae. Since cardiac surgery uses hypothermia induction to as low as 10°C, this temperature has been suggested as the lowest temperature for starting resuscitation.18 Nevertheless, although with the existing technology it is unlikely that successful resuscitation can be achieved with temperatures under 10°C, there are no convincing data for setting a lower limit for successful resuscitation. The recommendation is that in the absence of contraindications to CPR, we should attempt resuscitation in all deep HT victims, regardless of CBT.18,19
Cardiopulmonary resuscitation: continuous or intermittentIn the absence of vital signs for 1min (including carotid pulse), CPR should be started unless echocardiography (if available) evidences cardiac contractions.19
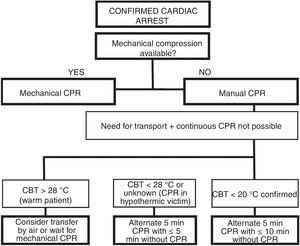
Hypothermia victims often require prolonged high-quality CPR.31–35 Manual CPR might prove technically impossible during rescue or evacuation. Mechanical thoracic compression devices help maintain continuous and quality CPR during evacuation and transport and, in severe HT, facilitate sufficient oxygen supply to the vital organs.11 However, maintaining continuous CPR also might not be possible. In these situations, and conditioned to the CBT, we could delay CPR or apply it manually and intermittently (Fig. 4).69
Manual and intermittent CPR algorithm for hypothermic victims when continuous CPR is not possible.69 CA: cardiac arrest; CPR: cardiopulmonary resuscitation; CBT: core body temperature.
Echocardiography or capnography can be used to monitor the efficacy of CPR or check the recovery of spontaneous heart rate.63
Determination of serum potassium as a biomarker for deciding the continuation of cardiopulmonary resuscitationHyperpotassemia is a cell lysis and death marker. The highest known potassium level where resuscitation proved successful was 11.8mmol/l.70 The experts and guides recommend suspending CPR and declare patient death if the serum potassium concentration exceeds 12mmol/l.11,18,19
In avalanche victims, the highest concentration where resuscitation proved successful in the absence of associated trauma was 6.4mmol/l.71 According to the European Resuscitation Council (ERC), the potassium cut-off point for not starting or for suspending CPR should be over 8mmol/l (Fig. 2).51 Recent algorithms (Fig. 3) propose a revision in which the potassium levels are not taken into acount.52
Since the introduction of ECLS as a rewarming technique, routine practice and the literature question the validity of potassium as a viability marker.13 Recently, Pasquier et al. have developed a scoring system with multiple independent variables (the HOPE score) that is superior to dichotomic triage based on the potassium concentration, for predicting which victims stand to benefit from ECLS. Further studies are needed to validate this tool, however.72
Triage and transferFig. 1 shows an algorithm that includes triage, transfer and choice of hospital, according to HT grade.11,18,19 If ECLS is indicated, the destination hospital should be alerted in order to not delay rewarming. If the distance or the weather conditions do not allow transfer, the victim should be moved to the nearest hospital with possibilities for rewarming using other techniques.19
The ideal temperature for victim transfer units is 28°C – the thermoneutral temperature of humans exposed to the open air7. However, this temperature is too warm for the accompanying staff, who are usually well equipped (rescuers, medical staff, drivers or pilots). Accordingly, a reasonable temperature for keeping the victim during transfer is about 24°C.18,19
Pre-hospital management: an approach to the real life situationTwo studies on the pre-hospital management of accidental HT have recently been published.28,29 One has been carried out in the United Kingdom among the different rescue groups related in some way to such management.28 The other publication is an international study on this subject in mountain rescue operations.29 The aim was to determine whether the first interveners had an operating plan based on the best available evidence; whether their knowledge was adequate; and whether the rescue material used allowed for correct intervention.
Both studies found that the teams were not prepared for following the recommendations of the guides regarding the management of severe HT, particularly when accompanied by CA. There were also other very worrisome findings, such as poor CBT monitoring, a lack of prevention of victim cooling after rescue, or transfer of the victims to the nearest hospital instead of to a center with ECLS – these being factors correlated to survival and neurological prognosis.
Since the year 2005, the ERC publishes resuscitation guidelines referred to CA in special situations.51 The resuscitation guidelines in relation to urban settings are easy to follow. However, doing so correctly in settings that are hostile and far from hospital centers (e.g., mountainous environments) may prove difficult and complicated: it might be necessary to adapt to the circumstances, or simply the required equipment might not be available.17 The mentioned publications28,29 have evidenced that many of the intervening teams lack medical staff or adequate material, and count on non-healthcare professionals or volunteers. According to Gordon and Paal,17 while these first interveners have all the necessary information, they may not be used to the format of medical publications, and the lack of specialized expert counseling might not allow them to adequately adapt to or apply the established guidelines. Nevertheless, these same authors acknowledge that the management of accidental HT has advanced greatly in the last 25 years – though there is still room for improvement.
Hospital management of accidental hypothermiaManagement of victims with cardiac arrest in a hospital without extracorporeal membrane oxygenationHospital reception of a HT victim under conditions of CA implies continuation of the previously adopted measures, the start or continuation of active internal rewarming (AIR), and the maintenance of continuous, prolonged and quality CPR until spontaneous recovery of heart rate. The most common AIR techniques include orotracheal intubation, mechanical ventilation with humidified oxygen warmed to 40°C, the infusion of warm fluids, and warm lavage of organ cavities.4 The most recommended forms of lavage in unstable victims or patients under conditions of CA where ECLS is not possible are peritoneal and pleural lavage.7 Another AIR option is continuous venovenous hemofiltration, though this technique requires adequate hemodynamic conditions and may require heparinization.5,11 The optimum rewarming rate is not clear. Theoretically, the most hazardous moment in AIR is on reaching CBT>28°C without spontaneous heart rate.11
Interpretation of blood gasesGas analyzers are programmed to operate with a CBT of 37°C. Because of this, it classically has been recommended to correct the values of pH, pO2 and pCO2 to the real CBT of the victim1. However, the current tendency is only to correct for pO2.73,74
Extracorporeal life supportIn severe HT, adequately selecting the destination hospital for rewarming with ECLS results in clear improvements in both survival,11–14,75–78 which has reached up to 100%13, and in the neurological outcomes,12–14,75,76 where the complete recovery rates have also reached 100%.76
Among the different ECLS rewarming systems, the extracorporeal circulation pump and venoarterial extracorporeal membrane oxygenation (ECMO-VA) are the techniques of choice in the presence of CA, severe hemodynamic instability, respiratory failure, refractory acidosis, or when other rewarming methods prove ineffective. In this context, ECMO-VA has become the method of choice, since it is similar to the extracorporeal circulation pump, with lesser heparinization requirements (important in trauma victims with CA and at high bleeding risk), greater portability, easy configuration without having to interrupt CPR, and no need for sternotomy. Furthermore, the technique is familiar in the ICU setting.35,78 In contrast, it does not seem advisable when the expected rewarming time is under 6h.79
Venovenous ECMO (ECMO-VV) is ineffective in CA (CPR is required), but it could be used in hemodynamically stable victims with severe respiratory failure after rewarming with ECMO-VA.11
During rewarming, adequate general anesthesia is indicated in order to prevent the victim from being awake. In general, the recommendation is to start rewarming with a temperature similar to the CBT of the victim, and to increase it gradually in order to avoid high temperature gradients.80
Chain of survival and coordinationThe key elements influencing the final outcome of severe HT are adequate planning and coordination of the rescue operation, the anticipation of possible problems, intervention adherent to the established protocols (including immediate and high-quality CPR), rewarming with ECMO, and adequate cardiorespiratory support.76–79
The severe HT center created in Krakow (Poland) in 2013 (and dependent upon the UCI) has shown that with these elements it is possible to shorten time to arrival in hospital, implement effective treatment, improve survival, and improve the final neurological outcome.33,76–79
The development and implementation of a national ECMO plan should not focus only on the management of severe respiratory distress, but should also contemplate the rewarming of severe HT in the presence of hemodynamic instability or CA.
ConclusionsAccidental HT is a potentially fatal condition that can occur in different scenarios.
In the pre-hospital setting, the following recommendations apply: (a) high quality resuscitation of victims under conditions of CA, independently of body temperature; (b) the adoption of measures to stop heat loss; (c) the start of rewarming using the means available; (d) the prevention of rescue collapse and afterdrop; and (e) adequate selection of the reference hospital conditioned to the clinical and hemodynamic situation of the victim.
Extracorporeal life support, with survival rates which in some cases reach 100%, has revolutionized the rewarming of victims with hemodynamic instability or CA.
The new evidences indicate that the management of accidental HT has progressed and has been able to substantially improve patient survival and the final neurological outcome.
Financial supportThe authors declare that this study has received no financial support.
Conflicts of interestThe authors declare that they have no conflicts of interest.
Please cite this article as: Avellanas Chavala ML, Ayala Gallardo M, Soteras Martínez Í, Subirats Bayego E. Gestión de la hipotermia accidental: revisión narrativa. Med Intensiva. 2019;43:556–568.