To determine the measurement properties of the Spanish version of the COMFORT Behavior Scale developed by van Dijk et al (2000) in paediatric critical care patients.
DesignProspective observational and psychometric study.
SettingLevel III Intensive Care Area at a university’s children hospital.
PatientsA total of 311 children with median age of 5.07 years (IQR = 0.9-11.7).
InterventionsNone.
Principal variables and resultsTo determine the measurement properties the Spanish version of the COMFORT Behavior Scale was simultaneous administered by two nurses to 311 patients admitted to an eighteen-bed critical care unit of a third level paediatric hospital. The Spanish version of the COMFORT Behavior Scale obtained a Cronbach alpha coefficient of 0.715 and it is a tool made up of three factors with two items in each domain: i) alertness and physical movement; ii) calmness/agitation and respiratory response/crying, and iii) muscle tone and facial tension.
ConclusionsThe COMFORT B was adapted to Spanish and it has shown to be a valid an reliable tool to assess comfort in a group of children admitted to an Spanish Intensive Care Unit.
Determinar las propiedades métricas de la escala COMFORT Behavior Scale desarrollada por van Dijk et al. (2000) en el contexto del paciente crítico pediátrico.
Diseñoestudio observacional, psicométrico y prospectivo.
Lugar de estudioUnidad de Cuidados Intensivos de un hospital pediátrico y universitario de tercer nivel asistencial.
PacientesUn total de 311 niños con una mediana de edad de 5,07 años (0,9-11,7).
Intervencionesninguna.
Principales variables y resultadosLa escala fue administrada de forma simultánea por dos enfermeros a 311 pacientes ingresados en una unidad de críticos de 18 camas de un hospital pediátrico de tercer nivel asistencial. La versión española de la COMFORT Behavior Scale obtuvo un alpha de Cronbach de 0,715 y está compuesta por tres factores, con dos ítems cada uno: (i) alerta y movimiento físico; (ii) calma/agitación y respuesta respiratoria/llanto; y (iii) tono muscular y tensión facial.
ConclusionesLa escala COMFORT B logró ser adaptada al idioma español y mostró ser válida para determinar y cuantificar el grado de confort en un grupo de niños ingresados en una unidad de cuidados pediátricos española.
The management of comfort in pediatric critically ill patients admitted to intensive care units (ICU) is one of the biggest challenges for health professionals,1,2 especially because assessing comfort in these patients is complex due to their low level of consciousness, severity of the disease, and use of sedatives.3
The management of these critically ill children is often invasive and aggressive and requires numerous traumatic procedures that can cause fear, pain, and discomfort in children.4,5 The pain felt by pediatric patients admitted to an ICU is one of the symptoms associated with the discomfort experienced by these patients. Therefore, the International Association for the Study of Pain defines it as a displeasing subjective sensory and emotional experience associated with an actual or potential lesion.1
Analgesia is essential in these pediatric critically ill patients to avoid pain and discomfort.6–8 It allows the nursing staff to perform invasive procedures safely, favors synchronization, and brings comfort to patients on mechanical ventilation.7 It prevents accidental extubations, and reduces metabolic9 and oxygen consumption in case of shock.10
At the same time, discomfort is an essential issue to take into consideration, especially in patients on deep sedation and mechanical ventilation who are unable to communicate.3 Therefore, sedation and analgesia become useful strategies to keep an optimal and safe level of comfort in critically ill children.11
Optimizing and protocolizing pain plus an optimal level of sedation early on during the management of pediatric critically ill patients reduces the child’s anxiety levels while at a hostile environment with techniques and procedures derived from clinical management.12,13 Also, an optimal control of the level of analgesia and sedation in the pediatric critically ill patient reduces the risk of impairment of the immune system and impacts morbidity.14
Over the last few years several tools have been designed to assess the degree of pediatric pain including physical and psychological aspects.15–19 The ability to communicate, the stage of development, and whether the child is undergoing an invasive procedure (such as intubation with sedation)21,41 are some of the aspects that should be taken into consideration when designing these pain assessment tools.20,21 Still, in order to be as objective as possible when categorizing this symptom, some authors say that it is important to include new physiological parameters such as skin conductance, the heart rate variability, and the electroencephalogram.22–24 A few examples of pediatric pain assessment tools are the Face, Legs, Activity, Cry, Consolability (FLACC) scale, based on the pediatric COMFORT scale and one of the most widely used in children25 or the Behavioral Pain Scale.
Regarding the assessment of the level of sedation and to minimize unnecessary exposure to sedatives and pain killers in pediatric intensive care units (PICU), several specific scales have been designed for quantification purposes. A few examples of these are the Motor Activity Assessment Scale, the Sedation-Agitation Scale, the Richmond Agitation Sedation Scale,14 the Ramsay Scale, and the COMFORT Scale.26,27
Also, there are 2 original scales available originally expressed in English language for a valid and reliable measurement of the concept of comfort in pediatric critically ill patients (from 0 years to 18 years): the COMFORT Behavior Scale (CBS) (2000)28–32 and the COMFORT Scale (1992).33,34 The goal of both scales is to assess the level of comfort from a psychological perspective as behaviors with negative effects on the human body and associated with fear, anxiety, and pain in critically ill children.31
In the specific context of Spanish-speaking countries there is no validated scale or tool to objectively quantify the degree of comfort in pediatric critically ill patients. That is the reason why this study was designed in the first place: to analyze the psychometric properties of the Spanish version of the COMFORT Behavior Scale (CBS-ES) by determining structural validity and reliability. We should mention that from now on we will be using the word and acronym COMFORT (in capital letters) to refer to the name of the scale and avoid confusions with the state of comfort.
MethodsThe validation and determination of the metric properties of the Spanish version of the COMFORT Behavior Scale developed by van Dijk et al. (2000) was conducted while taking into consideration the recommendations established by the Consensus-Based Standards for the Selection of Health Measurement Instruments (COSMIN) guidelines.35
Design and study centerWe conducted an observational and prospective study of transcultural adaptation, and validation of a tool in the ICU setting of an 18-bed tertiary pediatric hospital of Barcelona, Spain. The study period was from September 2015 through September 2016.
SampleThe study population included the total number of patients admitted in the context of the study (around 1450 a year). In an attempt to obtain relevant results and to eliminate bias as much as possible, it was estimated that a minimum sample of 221 individuals would be required (95% confidence interval and precision estimates of ± 5%). The anticipated population percentage was around 80% and that of necessary replacements around 5%.
The probabilistic stratified random sampling technique by age was used. Taking into consideration the recommendations of the World Health Organization (WHO), the sample was categorized into: infants (from 0 days to 28 days), babies (from 29 days to 2 years), preeschoolers (from 3 years to 5 years), schoolers (from 6 years to 12 years), and teenagers (from 13 years to 18 years).
The inclusion criteria were: 1) pediatric patients (from 0 years to 18 years) admitted to the critical care unit during the study period, and 2) acceptation and signing of the informed consent by the legal representatives and, in the case of mature minors (> 12 years), acceptation/consent of the subject. Patients excluded: 1) in palliative care; 2) with language barriers, and 3) those who had been receiving muscle relaxants in continuous infusion.
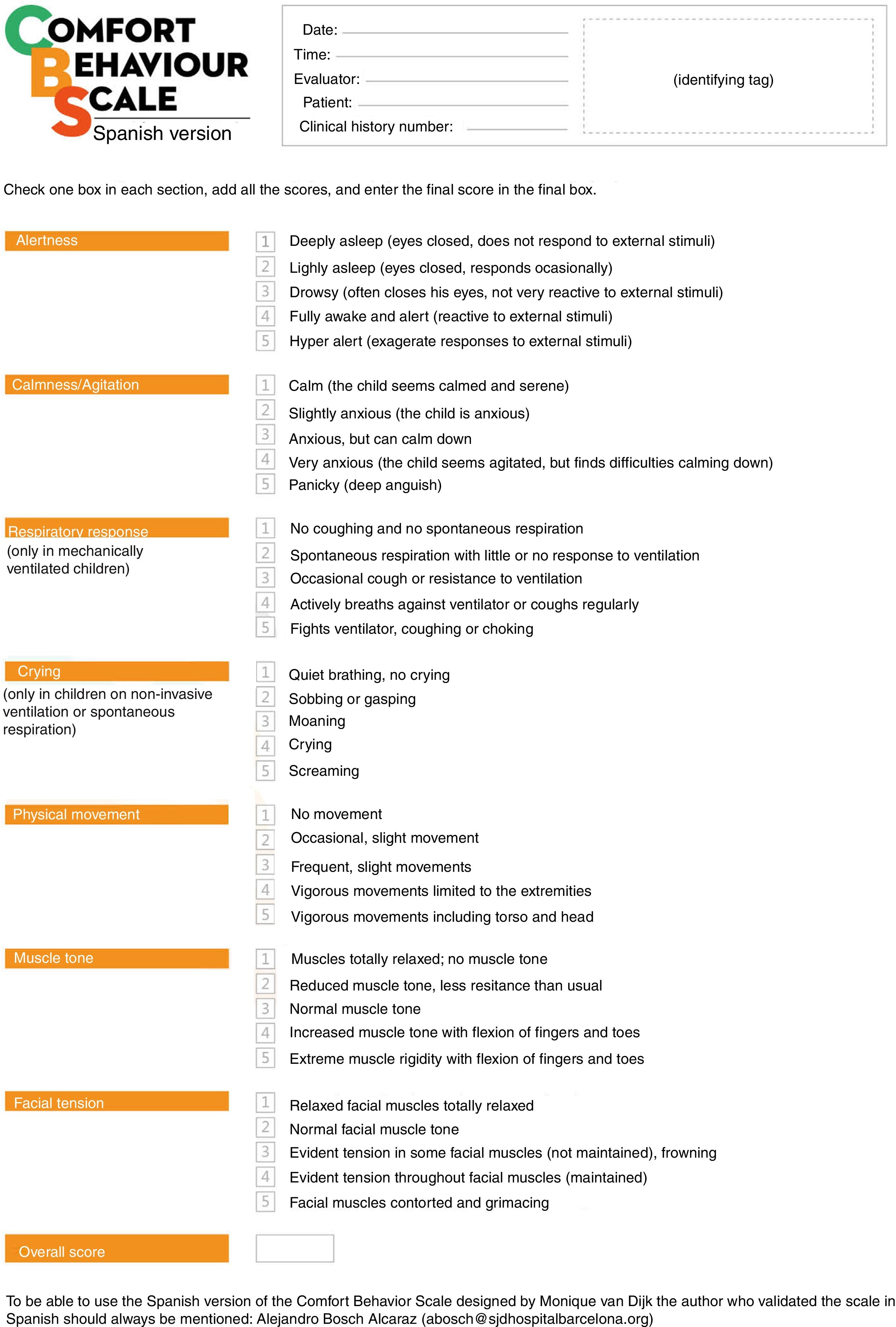
ScalesAs we mentioned before, there are currently 2 valid scales to assess the confort of critically ill patients: the COMFORT Scale (1992) and the COMFORT Behavior Scale (2001). Both scales measure 6 behavioral parameters (vigil, level of agitation/calmness, crying or respiratory response, physical movement, muscle tone, and facial tension) and 2 physiological parameters in the case of the 1992 scale (heart rate and mean arterial blood pressure). Because the heart rate and the mean arterial blood pressure can vary depending on different circumstances (drugs, improved or worsened pathological process, etc.),32 it was decided to accept and validate the CBS for the purpose of the present study.
During the process of validating the COMFORT Behavior Scale, Cronbach’s alpha coefficient was 0.78, but it went up to 0.84 after excluding the heart rate and mean arterial blood pressure from the scale.30 The COMFORT Behavior Scale assesses the correct management of the patient’s postoperative pain with scores ≤ 17. Regarding sedation, the authors define scores ≤ 11 as oversedation and they recommend checking scores from 11 to 22 using the Nurses Interpretation of Sedation Scale (NISS), that still has not been validated in Spain. Also, scores ≥ 23 are indicative of undersedation.
Prior to the study, the research team proceeded with a transcultural adaptation of the COMFORT Behavior Scale. For this purpose, the recommendations established by the International Test Commission36–38 were followed. Also, 4 bilingual professionals collaborated to determine which were the best semantic expressions of the scale using a process of translation-retranslation. Also, the content validity indices were estimated. Scores were between 0.76 and 0.80 in every item and 0.87 in the overall scale.39
Determining the psychometric properties of the COMFORT Behavior Scale-Spanish versionA group of 12 nurses with at least 5 years of experience managing critically ill pediatric patients was used to analyze the psychometric properties of the CBS-ES.
The social and demographic variables included were: 1) the unit of admission (PICU/Pediatric Semi-Intensive Care Unit [PSICU]); 2) sex (masculine/femenine); 3) age (in days, months or years); 4) medical diagnosis at admission (respiratory/postoperative/infectious/oncological/other); 5) the administration of sedoanalgesia (yes/no); 6) mechanical ventilation (yes/no), and 7) the overall stay at the critical care unit (in days). The main differences between patients admitted to the PICU and those admitted to the PSICU were the severity of their clinical condition and need to administer mechanical ventilation, complex cardiovascular support or extra-renal depuration techniques.
Data miningFirst, a team of 12 nurses from the critical care unit was assembled. In order to guarantee an adequate process of data mining, the principal investigator (ABA) designed a theoretical/practical training that included: a presentation in PowerPoint® (Microsoft) that explained the concept of comfort, the aspects to take into consideration regarding comfort, the final version of the CBS-ES, and the documents pertaining to the study data mining process. The theoretical session started by explaining what we understand as comfort. Then, the main objectives and procedure to be followed during research were established together with the scale that would be used (CBS-ES). The practical part of the training included an assessment of the level of comfort using the CBS-ES. For this purpose, every nurse screened 5 patients admitted in the context of the study. Finally, all the lingering doubts that emerged during the process of data mining were solved. Training lasted 5 hours. After training the CBS-ES required zero changes.
After performing all the necessary procedures that the patients admitted to the unit required, the patients’ informed written consent to participate in the study was formally requested. After obtaining it, 2 nurses per shift (morning, afternoon, and night) performed simultaneous assessments of the patients’ level of comfort using the CBS-ES. Therefore, data were collected 3 times a day (morning, afternoon, and night) within the first 48 hours after admission.
Data mining spanned throughout 7 months (from March to September 2016).
Statistical analysisA descriptive analysis of data was conducted. The derivatives of categorical variables were expressed as frequencies (n) and percentages (%), while the derivatives of quantitative variables were expressed as mean and standard deviation or median and interquartile range.
In order to determine the validity of the construct CBS-ES a factorial analysis of the main components was conducted.
The reliability of the CBS-ES was assessed using Cronbach’s alpha coefficient of the scale and every individual factor (valid with values > 0.7). Also, interobserver concordance was assessed using Cohen’s kappa coefficient (values > 0.60 were considered good values).
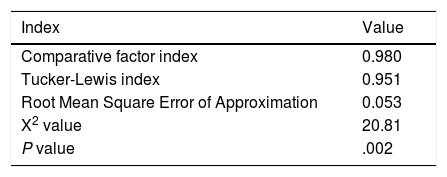
In order to determine the validity of the scale and taking into consideration the postulates posed by Satorra and Bentler back in 2001,40 a factorial analysis was conducted using the Robust Unweighted Least Squares (RULS) as the estimation method and the polychoric correlation matrix as the baseline matrix. The number of tool factors was determined through the parallel analysis method using the Comparative Factor Index (CFI > 0.90), the Tucker-Lewis Index (TLI > 0.90), and the Root Mean Square Error of Approximation index (RMSEA < 0.08). The adjustment indices were considered satisfactory according to the criteria established by Ullman in 2006.41 The comparisons in the models found were drawn using the S-B χ2 test envisioned by Satorra and Bentler back in 2001.40
The discomfort scores obtained in the CBS-ES were established while taking into consideration the mean and percentiles observed in the sample.
A 95% confidence interval was assumed in all the tests. Also, the data obtained were considered statistically significant with P values < 0.05.
Ethical considerationsThe hospital Ethics and Clinical Reseach Committee approved the study before it was conducted. The Bioethics Commission of a public university approved it as well. Also, Dr. Monique van Dijk, the author of the COMFORT Behavior Scale, gave her written informed consent to the study.
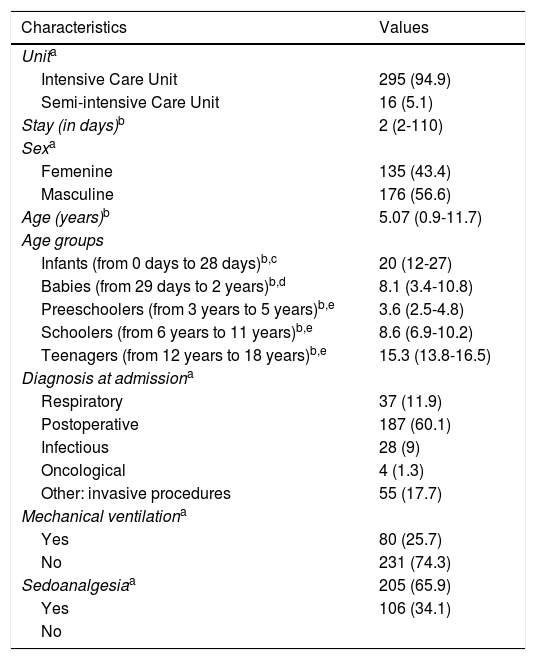
ResultsSocial and demographic characteristics of the patientsThis study included a total of 311 pediatric patients of whom 94.9% were hospitalized at the PICU. Fifty-six-point-six per cent were children with a median age of 5.07 years (0.9-11.7). The diagnosis that triggered the highest number of admissions in the critical care unit was postoperative in 60.1% (n = 187), being heart surgery (14.4%, n = 44) and scoliosis (10.9%, n = 34) the most prevalent ones. Of the total of patients admitted to the PICU, 25.3% were on mechanical ventilation and 65.9% (n = 205) on some sort of sedoanalgesia in continuous infusion. Morphine hydrochlorine (22.5%, n = 70) and fentanyl (5.5%, n = 17) were the analgesics most common of all. Pain was assessed using the FLACC scale, the PAIN scale, and the numeric scale and the following parameters were categotized: no pain = 0; mild pain = 1 to 3 points; moderate pain = 3 to 7 points, and severe pain = 7 to 10 points. Most patients reported no pain (n = 240) since they were on analgesia in continuous infusion (fentanyl or morphine hydrochlorine) sometimes combined with sedation (midazolam or propofol) or because they had an indication for some sort of discontinuous analgesia (metamizol, paracetamol or tramadol, mainly). The mean stay at the critical care unit was 2 days (2-110). No differences were seen in the social or demographic variables between patients admitted to the PICU and those admitted to the PSICU. Table 1 shows the social and demographic characteristics of the sample in detail.
Clinical and sociodemographic characteristics of the sample (n = 311).
| Characteristics | Values |
|---|---|
| Unita | |
| Intensive Care Unit | 295 (94.9) |
| Semi-intensive Care Unit | 16 (5.1) |
| Stay (in days)b | 2 (2-110) |
| Sexa | |
| Femenine | 135 (43.4) |
| Masculine | 176 (56.6) |
| Age (years)b | 5.07 (0.9-11.7) |
| Age groups | |
| Infants (from 0 days to 28 days)b,c | 20 (12-27) |
| Babies (from 29 days to 2 years)b,d | 8.1 (3.4-10.8) |
| Preeschoolers (from 3 years to 5 years)b,e | 3.6 (2.5-4.8) |
| Schoolers (from 6 years to 11 years)b,e | 8.6 (6.9-10.2) |
| Teenagers (from 12 years to 18 years)b,e | 15.3 (13.8-16.5) |
| Diagnosis at admissiona | |
| Respiratory | 37 (11.9) |
| Postoperative | 187 (60.1) |
| Infectious | 28 (9) |
| Oncological | 4 (1.3) |
| Other: invasive procedures | 55 (17.7) |
| Mechanical ventilationa | |
| Yes | 80 (25.7) |
| No | 231 (74.3) |
| Sedoanalgesiaa | 205 (65.9) |
| Yes | 106 (34.1) |
| No | |
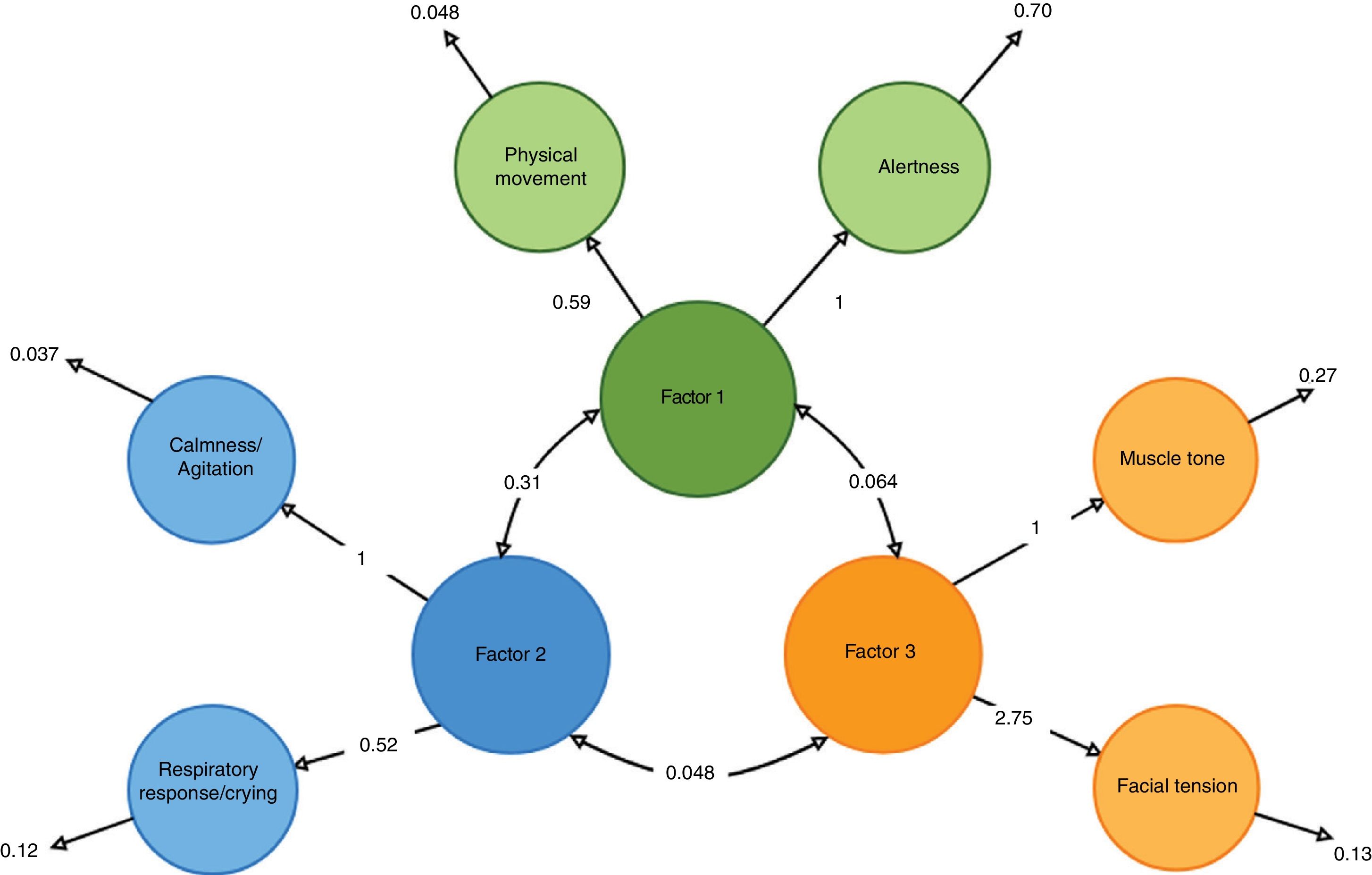
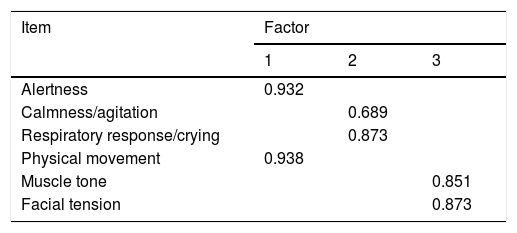
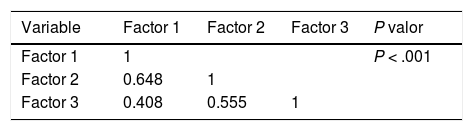
The main components were analyzed to determine the validity of the construct. It was confirmed that the factorial load of each item was > 0.40, indicative of an adequate relevance of the items (Table 2). The CBS-ES consists of 3 factors with 2 items per factor: 1) alertness and physical movement; 2) calmness/agitation and respiratory response/crying, and 3) facial tension and muscle tone. The correlation among the 3 factors of the scale was good (Table 3) as well as the adjusted goodness of fit indices of the model (Table 4).
Main factors of the COMFORT Behavior Scale-Spanish version.
| Item | Factor | ||
|---|---|---|---|
| 1 | 2 | 3 | |
| Alertness | 0.932 | ||
| Calmness/agitation | 0.689 | ||
| Respiratory response/crying | 0.873 | ||
| Physical movement | 0.938 | ||
| Muscle tone | 0.851 | ||
| Facial tension | 0.873 | ||
The numbers are the factors obtained.
The overalll item correlation was considered acceptable with values > .30.
Taking into account the mean and percentiles obtained in the distribution of the sample, it was determined tha the CBS-ES categorized discomfort as: no discomfort (≤ 11 points); medium discomfort (between 12 points and 22 points), and high levels of discomfort (≥ 23 points).
Fig. 1 shows a graphical representation of the structure of the CBS-ES.
Graphical representation of the correlation between factors and items of the COMFORT Behavior Scale-Spanish version.
The items of the CBS-ES were represented using circles.
A straight line shows the item factor load in the overall of the scale.
A bidirectional arrow unifies the factors of the CBS-ES.
Residual variance is shown next to each item.
The reliability of the CBS-ES was assessed by estimating the overall item correlation, Cronbach’s alpha coefficient, and the interobserver reliability. The internal consistence of the CBS-ES obtained a Cronbach’s alpha coefficient of 0.715. All the overall item correlations were > 0.30 except for respiratory response/crying (0.10) and muscle tone (0.22). Still, when establishing the matrix of item interrelation was established and and confirming whether the reliability of the scale would go up, it was confirmed that Cronbach’s alpha coefficient would have a slight increase (0.718). Still, this piece of information does not justify the elimination of the items of the scale. Taking into consideration the different age groups established the following values were obtained: infants obtained a Cronbach’s alpha coefficient of 0.785; babies, 0,736; preschoolers, 0.720; schoolers, 0.719, and teenagers, 0.632.
Regarding the interobserver correlation, when comparing the 311 pairs of observations, most items obtained Cohen’s kappa coefficients > 0.60 except for calmness/agitation (0.52), muscle tone (0.30), and facial tension (0.29). The kappa indices obtained based on the age group were infants, between 0.30 and 1; babies, between 0.51 and 0.71; preschoolers, between 0.52 and 0.68; schoolers, between 0.60-0.83, and teenagers, between 0.30 and 0.72.
DiscussionThe construct of comfort, especially in the pediatric critical care setting, should be assessed on a routine basis during the comprehensive management of these patients. The development of a valid and reliable scale such as the CBS-ES adapted to the Spanish social and demographic setting would allow health professionals to determine the level of discomfort of pediatric critically ill patients. As a matter of fact, this could improve the quality of the healthcare provided to patients assisted at the PICU setting.
As some studies conclude, the vital signs of a patient admitted to an ICU can be influenced by the treatments administered there. That is why the CBS or the CBS-ES don’t take arterial blood pressure or heart rate into consideration.32,39
There are several methods to do transcultural adaptation, but the translation-retranslation method is considered the most comprehensive one of all and the one that guarantees the highest quality in the scales adapted to this or that culture. That is why this was the method used in the Spanish adaptation of the COMFORT Behavior Scale.39
The results of this study show how the CBS-ES has an adequate reliability (Cronbach’s alpha coefficient of 0.715) although the data obtained are inferior to the ones obtained from other reference scales: the COMFORT Scale (0.90) and the COMFORT Behavior Scale (between 0.90 and 0.92).32,33
All the overall item coreelations were > 0.30 except for respiratory response/crying (0.10) and muscle tone (0.22). Further analyses did not justify the elimination of the items of the scale. Researchers believe that this is due to the fact that, at times, the variability of pediatric patients assisted in one of the units studied, their complexity and treatments complicate the objective assessment of these items. For this reason, future training sessions will be focused on how to understand these patients even better. Also, the kappa coefficients obtained were adequate, which shows the correct understanding of the items included in the scale.
The scores that determine situations of discomfort (no discomfort ≤ 11 points; discomfort 12-22 points, and high levels of discomfort ≥ 23 points) established after analyzing the characteristics of the CBS-ES are similar to those of the CBS regarding pain. According to van Dijk et al. (2000), scores > 17 in the CBS require revisiting the analgesic pattern of patients and comparing the values obtained with the numeric scale of pain to make sure that the patient has this symptom.23 We still don’t have statistical data to establish the predictive capabilities of the CBS-ES to determine situations of discomfort associated with the patient under or oversedation. Nonetheless, we should mention that the CBS defines that scores < 11 may lead to patient oversedation. In this sense, it is also important to emphasize that when the level of sedation was assessed and scores between 11 and 22 were obtained, the authors used the NISS score to compared these values. In this study, this could not be compared because after our reference search this tool could not be found transculturally adapted and validated to the Spanish population. Finally, we should mention that the authors of the CBS speak of undersedation situations with scores > 23.27 Here it is important to emphasize that it is agreed that comfort cannot be determined only with the scores obtained in the CBS-ES scale, but by comparing these scores with those of pain and sedation in pediatric critically ill patients.27
To this day, the fact that the scales used to measure the discomfort of pediatric critically ill patients have not been properly adapted or validated in Spanish language has complicated the possibility of assessing and managining it effectively enough. This would also explain the reason why there are very few empirical studies on the levels of discomfort and the impact of specific healthcare to bring comfort in samples of patients from non-English-spanish clinical settings. The validation of the CBS-ES scale made up of 3 factors with 2 items each (Fig. 2) is an advance in the comprehensive management of pediatric critically ill patients. Also, the CBS-ES scale could trigger future studies to determine the levels of discomfort of pediatric patients admitted to the ICU setting and the associated social, demographic, and clinical characteristics.
LimitationsOne of the main limitations of this study is the possibility of reproducing the results in other settings without previous specific training of the health professional on the CBS-ES. At the same time, future studies will be required to determine the predictive capabilities of the CBS-ES to detect situations of discomfort associated with pain and sedation, especially in patients on mechanical ventilation.
The COMFORT B scale was adapted to Spanish language and proved to be a valid tool to determine and quantify the level of comfort in a group of children admitted to a Spanish PICU.
This CBS-ES will allow health professionals to assist and assess pediatric critically ill patients. Also, treat the factors leading to their discomfort and analyze the impact of specific interventions to provide comfort. This will make us be more efficient when having to prioritize activities especially when providing comprehensive care as part of the process and healthcare setting of the pediatric critically ill patient.
AuthorsThe very first draft of this manuscript was written by ABA who designed the study and the documents used for data mining purposes. All the documents were reviewed by AFP and IJ. The statistical analysis was conducted by JGO and ABA. All the authors approved the final version of the manuscript.
FundingThis research obtained funding from 2 different competitive calls for tender: the one posted by the Nursing Research Projects of the Barcelona Official College of Nurses 2016 (PR 009-16) and that posted by the Catalonya Department of Health as part of the Health Research and Innovation Strategic Plan (PERIS) 2016-2020 (SLT002/16/00185).
Conflicts of interestNone reported.
We wish to thank the panel of experts who helped us in the transcultural adaptaion of the scale. Also, we wish to thank the nurses who helped us collect all the data. Last but not least, we wish to thank the children and their families for participating in this study.
Please cite this article as: Bosch-Alcaraz A, Jordan I, Guàrdia Olmos J, Falcó-Pegueroles A. Adaptación transcultural y características de la versión española de la escala COMFORT Behavior Scale en el paciente crítico pediátrico. Med Intensiva. 2020;155:542–550.